Review Article Open Access
Synchronous Colorectal Cancer Liver Metastasis: Is Simultaneous Approach the Best Strategy
Perini MV*, Coelho FF, Kruger JAP and Herman P
Department of Gastroenterology, Digestive Surgery Unit, University of São Paulo Medical SchoolSão Paulo, Brazil
- *Corresponding Author:
- Perini MV
University of Sao Paulo Medical School Gastroenterology
Rua Dr Eneas de Carvalho Aguiar 255 Sao Paulo, Brazil
Tel: 511981797885
E-mail: perini.marcos@gmail.com
Received date: January 29, 2014; Accepted date: February 19, 2014; Published date: February 28, 2014
Citation: Perini MV, Coelho FF, Kruger JAP, Herman P (2014) Synchronous Colorectal Cancer Liver Metastasis: Is Simultaneous Approach the Best Strategy. J Gastroint Dig Syst 4:174. doi:10.4172/2161-069X.1000174
Copyright: © 2014 Perini MV. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Synchronous colorectal cancer with liver metastasis (SCLM) represents a challenge for both surgeons and oncologists once 15-25% of patients diagnosed with colon cancer present metastatic liver disease. Surgical strategies have been developed in order to stratify patients and achieve better outcomes as simultaneous resection and reversal approach.
Keywords
Colorectal cancer; Liver metastasis; Simultaneous resection
Introduction
Synchronous colorectal cancer with liver metastasis (SCLM) represents a challenge for both surgeons and oncologists once 15-25% of patients diagnosed with colon cancer present metastatic liver disease [1]. Despite a worse prognosis when compared with metachronous metastases, surgical resection of all liver disease remains the only curative treatment of patients with SCLM with 5y survival ranging from 22-58% [2-6]. Simultaneous approach (SA) involves the resection of the primary tumor and the liver metastasis (with or with neoadjuvant chemotherapy) and contra pose to the classical colon first approach (CA). Reversal approach (RA) in which the metastatic liver disease is resected first is another therapeutic option that could be used in a minority of cases presenting with rectal cancer in which the amount of liver disease precludes a safe and margin free resection [7]. However the optimal surgical management of patients with SCLM remains controversial.
When facing the scenario of synchronic liver only metastasis of colorectal tumor, from the liver perspective, three main scenarios can be seen: 1-. unresectable, 2-potentialy resectable and 3-resectable liver disease.
Patients with Synchronic Unrespectable Liver Disease
Once patients with unrespectable liver lesion probably will not have a liver surgery performed upfront, these patients will be managed by oncologists and latter on, if substantial response occur, surgery could be discussed [8,9].
Patients with Synchronic Potentially Resectable Liver Lesions
These patients benefit from systemic chemotherapy based on oxaliplatin and eventually monoclonal antibodies. If the tumor responds (which can be seen from 30-80%), liver resection may be offered [10]. The main issue is if radiotherapy should be given to the patients with mid/low colorectal tumors. Patients with potentially resectable liver lesions will have systemic chemotherapy if tumors are located in the colon and associated radiotherapy if tumors are located in the mid/low rectum and considered advanced tumors (T3N+ or T4). Vigano et al. reported excellent long term results in patients with advanced rectal tumor and limited synchronic liver metastasis that had neoadjuvant chemo radiotherapy and simultaneous resection [11].
Patients with Synchronic Resectable Liver Lesions
For patients with resectable liver lesions, simultaneous, classical or reversal approach can be offered and the type of approach will depend in the amount of liver disease, primary stage, logistics between the colorectal and the liver team and patients’ performance status.
For patients with non metastatic locally advanced rectal cancer (T4 or T3N+), several randomized trials have shown that neoadjuvant chemoradiotherapy associated with total mesorectal excision (TME) is the best approach [12-14]. In a context of resectable liver metastasis only, one randomized trial showed increased disease free survival for patients that had neoadjuvant chemotherapy with FOLFOX [15]. So it seems a reasonable approach to patients with resectable liver disease and locally advanced rectal cancer to have systemic chemotherapy associated with radiotherapy. As conventional neoadjuvant 5-FU based chemoradiotherapy is inadequate to control distant metastases, oxaliplatin or irinotecan based schemes seem to be more rational (associated or not with target agents).
When using neoadjuvant treatment, the theoretical advantage of time test (tumor behavior) and eradication of micrometastatic disease is opposed to the liver injury secondary to its use. Parenchymal liver injury is a major concern in patients having more than 6 cycles of oxaliplatin/irinotecan [16,17] but its drawbacks could be overcome by two-stage hepatectomy or portal vein embolization [18,19]. Moreover, two retrospective series failed to demonstrate any survival advantage in patients with synchronic liver metastasis submitted to simultaneous liver and colonic resection that had neoadjuvant chemotherapy [20,21]. These data is contraposed by one bicentric study in which systemic chemotherapy was offered for patients with advanced liver disease (more than three resectable liver lesions) and locally advanced rectal cancer [11].
In order to better stratify patients in whom neoadjuvant chemotherapy could be useful, risk scores were proposed [22]. Indications for neoadjuvant chemotherapy in patients with SCLM have been suggested by some authors like patients with more than 3 lymph node metastasis, advanced rectal tumors (T4 or T3N+) and presence of extra-hepatic disease. In these patients, neoadjuvant chemotherapy seems to be reasonable but further studies are needed [23,24].
The effectiveness of new drugs (response rates ranging from 30- 70%) is challenging the use of radiotherapy in advanced mid/low rectal cancer [10]. Despite being the gold standard treatment of advanced distal rectal lesions (T3/4 and N+), radiotherapy lacks systemic effect and local complications are quite common [14]. On the other hand, with new drugs, systemic chemotherapy is as effective as radiotherapy in tumor response and spares patients unnecessary side effects [25,26]. Stronger evidence should be achieved in order to propose the best approach in patients with SCLM and advanced mid/low rectal cancer but preliminary data showed that in downsized patients, synchronic resection could be an interesting option, with good long term survival [11].
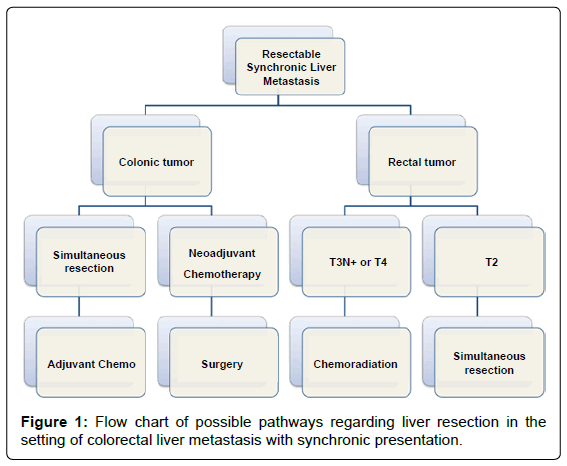
For patients with resectable liver lesions and not advanced mid/ low rectal tumors, upfront simultaneous surgery is an option for both liver and colon (Figure 1). As there in no prospective randomized study dealing with such approach, available data is mainly based in retrospective series and cohort studies.
After the advances in peri-operative management, simultaneous liver and colon resection (SLCR) has been proposed worldwide with acceptable morbidity and mortality and comparable survival [23,27-29]. Even more, some can argue that simultaneous resection in selected cases carries advantages such reduced length of hospital stay and costs over the classical approach. In which patient SLCR should be performed is still a matter of debate, but most hepatobiliary surgeons agree that specialized teams should do it and that minor liver resections are usually safe.
Regarding the type of resection most commonly performed in the simultaneous approach, one multicentric retrospective analysis showed a preponderance of colonic over rectal tumors and minor over major liver resections. Most of cases have unilateral liver disease and neoadjuvant chemotherapy was performed in less than one third of the cases when compared to the classical approach. Contrary, most cases submitted to reversal approach had chemotherapy before resection [6]. The timing of surgery is still a matter of debate, but most surgeons agree that the less chemotherapy patients have, the best. So, as soon as liver lesions are resectable, liver resection should be offered.
Many series have compared major liver resections and simultaneous colorectal tumor resection regarding staged vs. simultaneous approach [3,5,23,28-36]. Mortality rates were similar in in the two groups and when considering the two hospitalizations, morbidity and hospital stay were lower in the simultaneous group [4,32,36]. Data from one large multicentric retrospective study involving 1004 patients showed that for patients undergoing a major hepatectomy, there was no difference in overall complications between groups. Although the SLCR group had a higher incidence of mortality (8% vs. 2.8%) it was not statistically significant [6].
Simultaneous laparoscopic resection of colon and liver is feasible and many case series have shown good results. Lesions located in the antero-lateral segments are more prone to laparoscopic resection, but even major resections have been performed by specializes centers. Despite the lack of high quality evidence and survival data, it can be considered in a small subset of well-selected cases [37].
As demonstrated by retrospective studies and meta-analysis, longterm outcomes of overall and recurrence-free survival are similar when SCLM is compared to the classical approach [38-40]. When comparing the three approaches (classical, simultaneous and reversal) some studies have shown that the operative strategy had no impact on long-term outcomes, showing the importance of tumor behavior over the technical assessment [5,6]. Reversal approach may be a particularly beneficial in patients with a large amount of liver disease (but potentially resectable) and advanced rectal tumors, in order to not delay systemic treatment. Despite rational and widely discussed, until now only few studies (three observational and one retrospective cohort) have been published regarding reversal approach involving at all 91 patients [41].
Summarizing, simultaneous resection of colorectal liver metastasis is safe and feasible and should be considered in the treatment of selected patients with metastatic colorectal cancer in specialized centers.
References
- Manfredi S, Lepage C, Hatem C, Coatmeur O, Faivre J, et al. (2006) Epidemiology and management of liver metastases from colorectal cancer. Ann Surg 244: 254-259.
- Viganò L, Langella S, Ferrero A, Russolillo N, Sperti E, et al. (2013) Colorectal cancer with synchronous resectable liver metastases: monocentric management in a hepatobiliary referral center improves survival outcomes. Ann SurgOncol 20: 938-945.
- Tanaka K, Shimada H, Matsuo K, Nagano Y, Endo I, et al. (2004) Outcome after simultaneous colorectal and hepatic resection for colorectal cancer with synchronous metastases. Surgery 136: 650-659.
- Martin RC 2nd, Augenstein V, Reuter NP, Scoggins CR, McMasters KM (2009) Simultaneous versus staged resection for synchronous colorectal cancer liver metastases. J Am CollSurg 208: 842-850.
- Brouquet A, Mortenson MM, Vauthey JN, Rodriguez-Bigas MA, Overman MJ, et al. (2010) Surgical strategies for synchronous colorectal liver metastases in 156 consecutive patients: classic, combined or reverse strategy? J Am CollSurg 210: 934-941.
- Mayo SC, Pulitano C, Marques H, Lamelas J, Wolfgang CL, et al. (2013) Surgical management of patients with synchronous colorectal liver metastasis: a multicenter international analysis. J Am CollSurg 216: 707-716.
- Mentha G, Majno PE, Allal AS, Roth AD(2006) Neoadjuvant chemotherapy and resection of advanced synchronous liver metastases before treatment of the colorectal primary. Br J Surg 93: 872-878.
- Benoist S, Pautrat K, Mitry E, Rougier P, Penna C, et al. (2005) Treatment strategy for patients with colorectal cancer and synchronous irresectable liver metastases. Br J Surg 92: 1155-1160.
- Dexiang Z, Li R, Ye W, Haifu W, Yunshi Z, et al. (2012) Outcome of patients with colorectal liver metastasis: analysis of 1,613 consecutive cases. Ann SurgOncol 19: 2860-2868.
- Lam VW, Spiro C, Laurence JM, Johnston E, Hollands MJ, et al. (2012). A systematic review of clinical response and survival outcomes of downsizing systemic chemotherapy and rescue liver surgery in patients with initially unresectable colorectal liver metastases. Ann SurgOncol 19: 1292-1301.
- Viganò L, Karoui M, Ferrero A, Tayar C, Cherqui D, et al. (2011) Locally advanced mid/low rectal cancer with synchronous liver metastases. World J Surg 35: 2788-2795.
- Bosset JF, Collette L, Calais G, Mineur L, Maingon P, et al. (2006) Chemotherapy with preoperative radiotherapy in rectal cancer. N Engl J Med 355: 1114-1123.
- Gérard JP, Conroy T, Bonnetain F, Bouché O, Chapet O, et al. (2006) Preoperative radiotherapy with or without concurrent fluorouracil and leucovorin in T3-4 rectal cancers: results of FFCD 9203. J ClinOncol 24: 4620-4625.
- Kapiteijn E, Marijnen CA, Nagtegaal ID, Putter H, Steup WH, et al. (2001) Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med 345: 638-646.
- Nordlinger B, Sorbye H, Glimelius B, Poston GJ, Schlag PM, et al. (2008). Perioperative chemotherapy with FOLFOX4 and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC Intergroup trial 40983): a randomised controlled trial. Lancet 371: 1007-1016
- Karoui M, Penna C, Amin-Hashem M, Mitry E, Benoist S, et al. (2006) Influence of preoperative chemotherapy on the risk of major hepatectomy for colorectal liver metastases. Ann Surg 243: 1-7.
- Narita M, Oussoultzoglou E, Chenard MP, Rosso E, Casnedi S, et al. (2011) Sinusoidal obstruction syndrome compromises liver regeneration in patients undergoing two-stage hepatectomy with portal vein embolization. Surg Today 41: 7-17.
- Jaeck D, Oussoultzoglou E, Rosso E, Greget M, Weber JC, et al. (2004) A two-stage hepatectomy procedure combined with portal vein embolization to achieve curative resection for initially unresectable multiple and bilobar colorectal liver metastases. Ann Surg 240: 1037-1049.
- Narita M, Oussoultzoglou E, Jaeck D, Fuchschuber P, Rosso E, et al. (2011) Two-stage hepatectomy for multiple bilobar colorectal liver metastases. Br J Surg 98: 1463-1475.
- Allen PJ, Kemeny N, Jarnagin W, DeMatteo R, Blumgart L, et al. (2003) Importance of response to neoadjuvant chemotherapy in patients undergoing resection of synchronous colorectal liver metastases. J GastrointestSurg 7: 109-115.
- Reddy SK, Zorzi D, Lum YW, Barbas AS, Pawlik TM, et al. (2009) Timing of multimodality therapy for resectable synchronous colorectal liver metastases: a retrospective multi-institutional analysis. Ann SurgOncol 16: 1809-1819.
- Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH (1999) Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg 230: 309-318.
- Minagawa M, Makuuchi M, Torzilli G, Takayama T, Kawasaki S, et al. (2000) Extension of the frontiers of surgical indications in the treatment of liver metastases from colorectal cancer: long-term results. Ann Surg 231: 487-499.
- Capussotti L, Vigano' L, Ferrero A, Lo Tesoriere R, Ribero D, et al. (2007) Timing of resection of liver metastases synchronous to colorectal tumor: proposal of prognosis-based decisional model. Ann SurgOncol 14: 1143-1150.
- Chau I, Brown G, Cunningham D, Tait D, Wotherspoon A, et al. (2006) Neoadjuvantcapecitabine and oxaliplatin followed by synchronous chemoradiation and total mesorectal excision in magnetic resonance imaging-defined poor-risk rectal cancer. J ClinOncol 24: 668-674.
- Karoui M, Koubaa W, Delbaldo C, Charachon A, Laurent A, et al. (2008) Chemotherapy has also an effect on primary tumor in colon carcinoma. Ann SurgOncol 15: 3440-3446.
- Weber JC, Bachellier P, Oussoultzoglou E, Jaeck D (2003) Simultaneous resection of colorectal primary tumour and synchronous liver metastases. Br J Surg 90: 956-962.
- de Santibañes E, Fernandez D, Vaccaro C, Quintana GO, Bonadeo F, et al. (2010) Short-term and long-term outcomes after simultaneous resection of colorectal malignancies and synchronous liver metastases. World J Surg 34: 2133-2140.
- Martin R, Paty P, Fong Y, Grace A, Cohen A, et al. (2003) Simultaneous liver and colorectal resections are safe for synchronous colorectal liver metastasis. J Am CollSurg 197: 233-241.
- de Haas RJ, Adam R, Wicherts DA, Azoulay D, Bismuth H, et al. (2010) Comparison of simultaneous or delayed liver surgery for limited synchronous colorectal metastases. Br J Surg 97: 1279-1289.
- Chua HK, Sondenaa K, Tsiotos GG, Larson DR, Wolff BG, et al. (2004) Concurrent vs. staged colectomy and hepatectomy for primary colorectal cancer with synchronous hepatic metastases. Dis Colon Rectum 47: 1310-1316.
- Luo Y, Wang L, Chen C, Chen D, Huang M, et al. (2010) Simultaneous liver and colorectal resections are safe for synchronous colorectal liver metastases. J GastrointestSurg 14: 1974-1980.
- Reddy SK, Pawlik TM, Zorzi D, Gleisner AL, Ribero D, et al. (2007) Simultaneous resections of colorectal cancer and synchronous liver metastases: a multi-institutional analysis. Ann SurgOncol 14: 3481-91.
- Thelen A, Jonas S, Benckert C, Spinelli A, Lopez-Hänninen E, et al. (2007) Simultaneous versus staged liver resection of synchronous liver metastases from colorectal cancer. Int J Colorectal Dis 22: 1269-1276.
- Yoshidome H, Kimura F, Shimizu H, Ohtsuka M, Kato A, et al. (2008) Interval period tumor progression: does delayed hepatectomy detect occult metastases in synchronous colorectal liver metastases? J GastrointestSurg 12: 1391-1398.
- Capussotti L, Ferrero A, Viganò L, Ribero D, Lo Tesoriere R, et al. (2007) Major liver resections synchronous with colorectal surgery. Ann SurgOncol 14: 195-201.
- Lupinacci RM, Andraus W, De Paiva Haddad LB, Carneiro D Albuquerque LA, Herman P (2014) Simultaneous laparoscopic resection of primary colorectal cancer and associated liver metastases: a systematic review. Tech Coloproctol 18: 129-135.
- Yin Z, Liu C, Chen Y, Bai Y, Shang C, et al. (2013) Timing of hepatectomy in resectable synchronous colorectal liver metastases (SCRLM): Simultaneous or delayed? Hepatology 57: 2346-2357.
- Slesser AA, Simillis C, Goldin R, Brown G, Mudan S, et al. (2013) A meta-analysis comparing simultaneous versus delayed resections in patients with synchronous colorectal liver metastases. SurgOncol 22: 36-47.
- Li ZQ, Liu K, Duan JC, Li Z, Su CQ, et al. (2013) Meta-analysis of simultaneous versus staged resection for synchronous colorectal liver metastases. Hepatol Res 43: 72-83.
- Lam VW, Laurence JM, Pang T, Johnston E, Hollands MJ, et al. (2014) A systematic review of a liver-first approach in patients with colorectal cancer and synchro nous colorectal liver metastases. HPB (Oxford) 16: 101-108.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 15502
- [From(publication date):
April-2014 - Apr 26, 2025] - Breakdown by view type
- HTML page views : 10847
- PDF downloads : 4655