Mini Review Open Access
Survival Prediction of End Stage Cancer Patients: A Quick Review
Vincent Thai*, Gary Wolch and Yoko Tarumi
University of Alberta Hospital, Edmonton, AB Canada
- *Corresponding Author:
- Vincent Thai
University of Alberta Hospital
Edmonton, AB Canada
E-mail: vincent.thai@albertahealthservices.ca
Received date: September 13, 2013; Accepted date: October 29, 2013; f Published date: November 4, 2013
Citation: Thai V, Wolch G, Tarumi Y (2013) Survival Prediction of End Stage Cancer Patients: A Quick Review. J Palliat Care Med 3:164. doi: 10.4172/2165-7386.1000164
Copyright: © 2013 Thai V, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Survival prediction for end stage cancer patientsremains an important task in Palliative Medicine. Previously more of an art form, survival prediction has now become increasingly objective, utilizing statistical estimates of survival. Both clinician prediction survival and actuarial estimation of survival have their uses and drawbacks. This article examines the pros and cons of each and how both can be utilized at the bedside.
Keywords
Survival prediction; Palliative cancer patients; Prognosis; Review; Prognostic tools
Introduction
Patrick Young [1] was quoted as saying, “the trouble with weather forecasting is that it is right too often for us to ignore it and wrong too often for us to rely on it “. As with weather forecasting, survival prediction of terminally ill cancer patients is an attempt to apply objective actuarial data to a circumstance with an infinite number of variables. For many physicians, nurses and other allied health care professionals, formulating and conveying survival predictions can be a daunting task [2]. However, survival prediction for end stage cancer patients remains an important task in Palliative Medicine [3]. Previously more of an art form, survival prediction has now become increasingly objective, utilizing statistical estimates of survival [4], with the use of actuarial estimation of survival (AES), presented as scores or indexes. Clinician prediction of survival (CPS), on the other hand, depending on the clinician’s experience and clinical context, formulates a survival prediction, usually in the form of a temporal prediction. To be able to use both CPS and AES tools for survival prediction require understanding of the pros and cons of each.
Survival prediction is helpful for the following reasons:
• Helps to determine goals of care and decision making by patients and families; medical decision-making by the health care team e.g. to proceed or not proceed with life sustaining treatments such as intravenous anti-biotics and transfusions.
• Patients and families want to know.
• Helps to determine the most appropriate care in the best possible setting e.g. hospice eligibility criteria.
• Resource allocation and future policy planning e.g. subsidized palliative drug plan coverage.
• Potential common language for health care practitioners who are involved in end of life planning.
Factors Influencing Survival in Advanced Cancer
Around 150 variables have been studied to predict survival [5,6]. When formulating survival prediction in the early stages of cancer, tumor pathology, co-morbidities and response to oncologic therapy are of greater importance. However, during the latter stages of cancer (e.g. stage IV metastatic small cell lung cancer), performance status, anorexia, systemic inflammation, lymphopenia, edema, symptoms like delirium, dyspnea and dysphagia become more important predictors. Many actuarial prognostic tools are based on these prognostic factors that occur during the later stages of the cancer e.g. delirium, dyspnea, poor performance status etc). A more detailed look at the variables that have either a definite or possible impact on survival prediction can be found in Table 2 of Dr Paul Glare’s paper [3] and being familiar with these factors can be very helpful.
| Factor | Partial score |
|---|---|
| PPS 10-20 | 4 |
| 30-50 | 2.5 |
| > 50 | 0 |
| Delirium | 4 |
| Dyspnea at rest | 3.5 |
| Oral intake: mouthfuls or less | 2.5 |
| Reduced, but more than mouthfuls | 1 |
| Edema | 1 |
the overall score. The final PPI score stratifies the patients in 1 of these 3 groups:
PPI >=6 : survival time of less than 3 weeks
PPI >=4 but less than 6 : survival time shorter than 6 weeks
PPI <4 : survival time more than 6 weeks
Table 2: Palliative Prognostic Index (PPI)
Clinician Predicted Survival (Cps) Versus Actuarial Estimation of Survival (Aes)
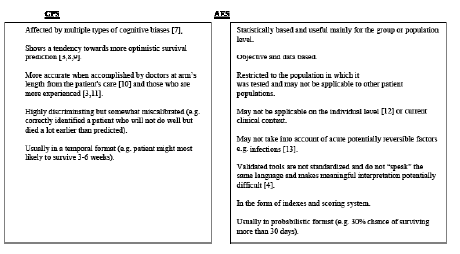
Some of the features, including advantages and disadvantages of CPS and AES are summarized as follows:
Statistical Methods Employed in Aes
There are a myriad of statistical methods employed in these AES [14]. Common methods include survival curves, with potential problems of censoring and patients lost to follow up. Receiver operator characteristics curve is also often used to assess discrimination for binary responses e.g. alive or dead. Multi-variate analysis is often used but not all patients have the same set of factors due to the heterogeneity of end stage cancer patients. A more detailed description of the statistical methods can be found in the paper by Bartfay [14].
Discussion
CPS is a complex, dynamic process, taking into consideration patient and disease related factors, performance status, symptom burden, and disease trajectory and laboratory markers. It does not do so in a vacuum without observation and data, thus some actuarial information is incorporated in the CPS, with the potential to acquire more new information as patients develop more medical problems. However, miscalibration remains a problem where patients may potentially be over treated or have a late palliative referral if the actual survival is shorter than predicted. On the contrary, potential undertreatment or a premature palliative referral, if the actual survival is longer than predicted.
Additionally, the actuarial survival data is not independent of bias, an example being the varied interpretation of functional status scales and symptoms. Still, like weather forecasting, survival prediction, despite its fallibility, can help us avoid certain “hazards”. In the case of end stage cancer patients, these “hazards” may mean overly aggressive treatment or transfer to an inappropriate location of care. The need for accurate prognostication in determining goals of care and care planning necessitates our pursuit to further define and validate clinical factors e.g. delirium, anorexia etc.
Various AES palliative prognostic tools (see appendix A on some examples of AES tools) have been developed to improve the prognostic inaccuracy of the clinician prediction survival. The evidence of the predictive value of the Palliative Performance (PaP) score is among the best. However, each palliative prognostic tool has its own drawbacks [3]. For example, being constrained to the 30 day limit and needing blood work in the PaP tool may not practical in certain settings (e.g. hospice or near death) and not ideally applicable to Onco-hematological patients. The other disadvantage is that it does not include delirium which is an important prognostic factor. Definitions of symptom based prognostic factors in the Palliative Prognostic Index (PPI) and PaP are difficult to dichotomize as symptoms including dyspnea, appetite and delirium are always on a continuum, with subjective interpretation (Table 1). The Palliative Performance Scale (PPS) may not be sufficiently discriminatory for prediction survival and mid range PPS levels may be harder to interpret [3]. Even biological parameters, (e.g. inflammatory markers), may not be readily accessible and potentially confounded by acute medical events e.g. superimposed infections.
| Criterion | Assessment | Partial score |
|---|---|---|
| Dyspnea | No Yes |
0 1 |
| Anorexia | No Yes |
0 1.5 |
| Kamofsky Performance Scale |
>30 10 – 20 |
0 2.5 |
| Clinical prediction of survival (weeks) | >12 11 – 12 7 – 10 5 – 6 3 – 4 1 – 2 |
0 2 2.5 4.5 6 8.5 |
| Total WBC (x10 9/ L) | <8.5 8.6 – 11 >11 |
0 0.5 1.5 |
| Lymphocyte percentage | 20 – 40 % 12 – 19.9 % < 12 % |
0 1 2.5 |
| Risk group A B C |
30 day survival >70 % 30 – 70 % < 30 % |
Total score 0 – 5.5 5.6 – 11 11.1 – 17.5 |
Table 1: The Palliative Prognostic Score (PaP)
Other prognostic tools may have the problem of irrelevant time frames e.g. 2 week time frame for the Cancer Prognostic score. The short term prediction and complex formula to calculate survival for the Intra-hospital Cancer Mortality Risk Model (ICMRM) may discourage use. Survival normograms do have their advantages but may not take into account of acute potentially reversible factors e.g. infections [13] and advent of new targeted palliative oncological treatments which may prolong life.
Moreover, survival prediction scores from these validated tools do not “speak” the same language and is subjected to interpretation [4]. They are not interchangeable and may not be appropriate with the clinical scenario at hand. It is also unclear which tools should be used and at what time points of the disease trajectory and in which clinical context. How valid are these tools will depend on future validation studies. Though mathematically more accurate in calculating survival on a population basis [12], what limits the application of AES is due to the fact that these tools only account for a small part of the variance in patients’ observed survival, and the lack of consistency amongst prognostic factors between cancer patients individually. The actual clinical impact of these tools remains to be seen. Ultimately, the ideal AES prognostic tool will need to be user friendly to allow its uptake and be presentable to patients for it to be useful. Unfortunately, no single prognostic index or scoring system has been universally successful in predicting outcomes across populations, especially on individual patients [11,12].
As part of a bigger picture, one can hypothesize if an expert opinion in the form of a palliative consult may help with survival prediction of patients with intermediate prognosis. This is assuming that the expert opinion may have a better understanding of the prognostic markers.
Conclusions and Recommendations
AES estimation of survival is generally superior to clinical judgment mathematically; and that is because the accuracy of probabilistic survival prediction is inherent in AES. However, CPS is often retained as independent survival predictor on multivariate analysis [11]. Hence, current literature recommends the use of both clinician prediction survival and use of objective validated AES tools together [8,15]. Though certain AES do contain the CPS, e.g. PaP, it will be interesting if the initial CPS in the PaP is the same as the final CPS from the same clinician i.e. how stable the CPS is? A clinician may use a prognostic score or index as a starting point and refine the prognosis to the clinical scenario [3].
For example, a probabilistic survival prediction score may not harmonize well with guidelines for admission to hospices or qualify for subsidized palliative drug plans (e.g. hard to apply a survival of 30%- 70% chance by 30 days compared to hospice criteria of < 3 months). However, on going through the mental exercise of using an AES, it can be very educational in seeing the presence/ absence of various prognostic factors when applied to the patient. With this understanding, a CPS can then be formulated. The clinician at the bedside will take the overall clinical situation into consideration with a validated AES tool (e.g. PaP, PPS) and formulate the survival prediction (e.g. 3 to 6 weeks) relevant to the individual patient, clinical context and hospice criteria. However, future studies will need to be done to validate this approach.
References
- http://patricklyoung.net/about-patrick/
- Christakis NA, Iwashyna TJ (1998) Attitude and self-reported practice regarding prognostication in a national sample of internists. Arch Intern Med 158: 2389-2395.
- Glare P, Sinclair C, Downing M, Stone P, Maltoni M, et al. (2008) Predicting survival in patients with advanced disease. Eur J Cancer 44: 1146-1156.
- Lau F, Cloutier-Fisher D, Kuziemsky C, Black F, Downing M, et al. (2007) A systematic review of prognostic tools for estimating survival time in palliative care. J Palliat Care 23: 93-112.
- Viganò A, Dorgan M, Buckingham J, Bruera E, Suarez-Almazor ME (2000) Survival prediction in terminal cancer patients: a systematic review of the medical literature. Palliat Med 14: 363-374.
- Justice AC, Covinsky KE, Berlin JA (1999) Assessing the generalizability of prognostic information. Ann Intern Med 130: 515-524.
- Goodman J (2007) How doctors think. Houghton Mifflin, Boston.
- Glare PA, Sinclair CT (2008) Palliative medicine review: prognostication. J Palliat Med 11: 84-103.
- Evans C, McCarthy M (1985) Prognostic uncertainty in terminal care: can the Karnofsky index help? Lancet 1: 1204-1206.
- Christakis NA, Lamont EB (2000) Extent and determinants of error in doctors' prognoses in terminally ill patients: prospective cohort study. BMJ 320: 469-472.
- Glare P, Virik K, Jones M, Hudson M, Eychmuller S, et al. (2003) A systematic review of physicians' survival predictions in terminally ill cancer patients. BMJ 327: 195-198.
- Henderson R, Keiding N (2005) Individual survival time prediction using statistical models. J Med Ethics 31: 703-706.
- Thai V, Lau F, Wolch G, Yang J, Quan H, et al. (2012) Impact of infections on the survival of hospitalized advanced cancer patients. J Pain Symptom Manage 43: 549-557.
- Bartfay E, Bartfay WJ (2008) Accuracy assessment of prediction in patient outcomes. J Eval Clin Pract 14: 1-10.
- Parkes CM (2000) Commentary: prognoses should be based on proved indices not intuition. BMJ 320: 473.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 15268
- [From(publication date):
December-2013 - Nov 21, 2024] - Breakdown by view type
- HTML page views : 10857
- PDF downloads : 4411
