Research Article Open Access
Survival of Teeth Restored with Atraumatic Restorative Treatment in a Pediatric Rural Population
Ana Lucia Seminario1*, Christine Wang1, JoAnna Scott2, Patrick Rooney3 and Penny Leggott11Department of Pediatric Dentistry, University of Washington, Seattle, Washington, USA
2School of Dentistry, University of Missouri, Kansas City, Missouri, USA
3Blaine Harbor Dental, Blaine, Washington, USA
- *Corresponding Author:
- Seminario AL
Assistant Professor
International Visiting Dentist Program, and Director
Department of Pediatric Dentistry University of Washington
Seattle, Washington 98105, USA
Tel: 206-543-4570
E-mail: alsadem@uw.edu
Received Date: July 20, 2017; Accepted Date: August 02, 2017; Published Date: August 10, 2017
Citation: Seminario AL, Wang C, Scott JA, Rooney P, Leggott P (2017) Survival of Teeth Restored with Atraumatic Restorative Treatment in a Pediatric Rural Population. J Oral Hyg Health 5: 224. doi: 10.4172/2332-0702.1000224
Copyright: © 2017 Seminario AL, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Oral Hygiene & Health
Abstract
Objectives: To determine the overall 5-year survival rate of teeth treated by atraumatic restorative treatment (ART) delivered by general practitioners in a rural population in Washington State, USA. Methods: Inclusion/exclusion criteria included children (≤ 12 years and younger) who received ART on asymptomatic carious primary teeth without history of previous restoration (N=178). For this longitudinal study, data collection included demographics, health status, initial date of ART placement, date of ART re-placement, and baseline dmft/DMFT. Variables collected at follow ups included appointment dates, dmft/DMFT, final restorative treatment, pulp therapy, and extraction. Descriptive statistics were calculated for all variables while Kaplan-Meier survival curves were used to summarize overall treatment success. Unadjusted and adjusted hazard ratios (HR) from Cox Proportional Hazard Regression with robust standard error were used to compare survival rates for variables of interest (P<0.05). Results: The overall 5-year survival rate of primary teeth receiving ART restorations was 69.5%. While age, gender, baseline dmft/DMFT, tooth type, and number of ART surfaces were not associated with tooth survival time, child’s health status had a significant association (p=0.02). Conclusion: Among this pediatric rural population, a significant tooth survival rate was observed following treatment with ART. Replenishing ART was successful in extending survival tooth until their natural exfoliation or placement of a definitive restoration.
Keywords
Atraumatic restorative treatment; Children; Tooth survival; Dental caries; General dentistry; Rural community
Introduction
In the 1980s, a pilot study conducted in Tanzania demonstrated a reduction in the need for tooth extraction after removal of soft demineralized dentin from dental cavities that were then filled with polycarboxylate cement [1]. Remarkably, only one of the twentyeight permanent teeth treated in this manner was extracted while the remainder was asymptomatic nine months after treatment [2]. This technique became known as the atraumatic restorative treatment (ART) [3]. Since this initial study, the technique has evolved and been refined to utilize hand instruments to enlarge the orifice of small cavities to be restored with glass ionomer material. ART offers a method to manage and prevent caries progression in challenging environments such as remote areas, field practices, schools, village halls or in community health centers with limited equipment, and has been endorsed by the World Health Organization [4].
Dental caries remains a major public health burden affecting diverse populations, especially children [5]. In children, the effectiveness and survival of ART have been measured by comparing single-surface to multiple-surface restorations. De Amorin et al. showed that after a follow up of over two years, teeth treated using ART have survival rates of 93% and 62% for single- and multiple-surface, respectively [6]. Another study found that the mean and median estimated survival of ART restorations in single-surface primary teeth were 37 months and 38 months respectively, while the survival rates were 94% at 12 months and 20% at 48 months [7]. Evidence supports ART as a successful treatment option for young children unable to cope with definitive dental restorative treatment, patients with special needs, uncooperative patients, and populations with limited access to definitive dental treatment [8-11].
General and family dentists are often those in the forefront of managing routine pediatric oral health. Because of the characteristics of ART, this technique has become an option among these practitioners. A cross-sectional survey of general dentists conducted in Hong Kong reported that ART was the preferred treatment option for a hypothetical 4-year-old healthy and cooperative boy, whereas pediatric dentists favored conventional restorative treatment for the same patient [12]. A second cross-sectional survey conducted in England reported similar results where ART was the preferred method among the general dental practitioners to restore a primary molar with a proximal lesion in a six-year-old boy [13]. Because general dental practitioners have demonstrated a preference for the use of the ART technique, it is important to evaluate the outcome and survival of teeth treated with ART in a general practice.
Most of the current atraumatic restorative treatment literature focuses on the survival of the restorations. This paper aims to describe the 5-year survival rate of primary and young permanent teeth treated with ART and to identify demographic dental variables associated with the success rate of teeth that received ART. The study population came from a rural area of Washington State and received care in a general dental practice.
Methods
Study population
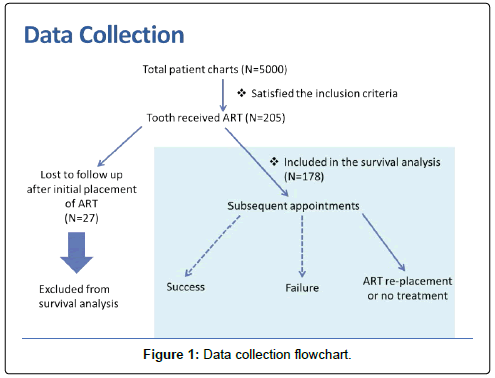
This project was approved by the University of Washington Human Subjects Review Board (#44883). Children between 2 and 12 years old who received dental care in a general practice in the rural northwest area of Washington State, USA between 2000-2009 were included in this longitudinal study. The initial database consisted of approximately 5,000 paper charts of inactivated patients (adults and children) donated from a general practice to the University Of Washington Department Of Pediatric Dentistry for assessment of effectiveness of the ART technique. Eligibility for this study included children: a) with behavioral challenges that did not allow definitive restorative treatment, b) with at least one initial ART placement on a primary tooth that was asymptomatic and had no previous restoration, c) with at least one follow up appointment, and d) who were not candidates for dental treatment under sedation and/or general anesthesia. One hundred seventy-eight subjects satisfied the inclusion and exclusion criteria (Figure 1).
Intervention
Two general dentists trained using the Atlas of Pediatric Dentistry guidelines on ART placement written by University of Washington pediatric dentistry faculty members performed the restorative treatment [14]. Specifically, ART restorations were performed by removing affected dentin using hand instruments. Cotton rolls were used for isolation. Vitrebond™ light-cure glass ionomer liquid and powder (3M ESPE) was hand-mixed, applied to the cavity preparation and halogen light-cured for 20 seconds, according to the manufacturers’ instructions.
Data collection
For this study, initial ART placement was defined as the first instance of ART placement recorded in the patient chart. We followed up only the first documented tooth receiving ART for each child as recorded in the chart notes. Bitewings or periapical radiographs taken at the recall appointments were only utilized to estimate the date of natural exfoliation of the primary tooth of interest when this information was not available in the dental chart. One hundred seventy-eight subjects with at least one follow up appointment were included in this study. All data was abstracted from the charts by one of the authors (CW) who was calibrated with two senior faculty members (PL & ALS) for accuracy.
Demographic variables
The following demographic variables were extracted from the patient charts: child’s date of birth, gender; and health status. Age was calculated as date of initial ART placement minus the child’s date of birth and then categorized as follows: 1) 0-2 years (prior to full set of primary dentitions), 2) 3-6 years (full primary dentition), and 3) 7-12 years (mixed dentition). Health status was categorized as ASA I (healthy) versus ASA II or more (not healthy), based on the medical history form.
Dental variables
The following dental variables were extracted from the patient charts: number of decayed, missing, or filled teeth for primary and permanent dentition (dmft or DMFT, respectively) at initial ART placement; date of initial ART placement and date of ART re-placement(s); location of the ART placement (anterior versus posterior); and number of surfaces restored with ART within the selected tooth. DMFT and dmft were categorized into 3 groups: 1) 2 or less, 2) 3-4, and 3) 5 or more. When both permanent teeth and primary teeth were present, DMFT and dmft were combined. The number of surfaces restored with ART was categorized as 1) 1 surface, 2) 2 surfaces, and 3) 3 or more surfaces.
Definition of dental procedures at follow up
The type and date of ART treatment outcomes were recorded at each recall appointment. Related variables were categorized as follows:
Extraction: The dental record indicated that the ART tooth was extracted, due to either abscess or clinical symptoms of necrotic pulp or irreversible pulpitis. Date of the extraction was recorded as indicated in the patient chart.
ART remains without treatment: Tooth receiving ART restoration had no symptoms, had no re-placement recorded.
ART re-placement: The dental record indicated ART re-placement. Date of the ART re-placement was recorded as indicated in the patient chart.
ART replaced by a definitive restoration at a later date: Record indicated that a definitive restoration (composite, amalgam or stainless steel crown) was placed. Date of the definitive restoration was recorded as indicated in the patient chart.
Pulp therapy and stainless steel crown (SSC): Date of the pulp therapy and SSC was recorded as indicated in the patient chart.
Definition of ART treatment success
In order to assess effectiveness of this technique delivered by general practitioners in a real-setting environment we defined success as: Natural exfoliation, ART replaced by composite or SSC at a later date, ART without treatment, and ART re-placement were considered as successes because these are compatible with caries lesions not progressing into irreversible damage of pulpal tissue of the tooth.
Definition of ART treatment failure
Because prevention of caries progression into the pulpal tissue of the tooth is one of the therapeutic goals of ART, we defined failure as: Extraction, pulp therapy, abscess, and spontaneous pain were designated as failures because these treatments were performed in response to caries progression into the pulpal tissue of the tooth, which does not meet the primary therapeutic goal of ART [15].
Data analysis
Data were captured using REDCap Software Version 5.7.3 (Vanderbilt University) and then imported into Stata 12.0 (College Station, TX) for analysis. Descriptive statistics were calculated for all variables. Kaplan Meier curves were calculated for overall treatment success and to demonstrate survival rate for each variable. Unadjusted and adjusted Hazard Ratios (HR) from Cox Proportional Hazard Regression with robust standard errors was used to compare survival rates for variables of interest. The significance level was established at 5%.
Results
Descriptive statistics
A total of 178 patients were included in this analysis. The majority of the sample was 3-6 years old (63.5%) and considered healthy (84.3%). Half of the children (51.7%) were male and 37.6% had a dmft/DMFT of five or more. Teeth treated with ART restorations were primarily posterior teeth (75.8%) and had 2 carious surfaces (50%). Of the 178 patients included, 31 patients had teeth that failed to survive after receiving ART (17.4%). Impact of missing data (11.2%) on the association between dmft/DMFT and ART failure was not statistically significant (p=0.737 data not shown) (Table 1).
| ART Failure | |||
|---|---|---|---|
| No (N = 147) |
Yes (N = 31) |
Total (N = 178) |
|
| Age at ART Placement | |||
| 0-2 | 15 (10.2%) | 4 (12.9%) | 19 (10.7%) |
| 3-6 | 95 (64.6%) | 18 (58.1%) | 113 (63.5%) |
| 7-12 | 37 (25.2%) | 9 (29%) | 46 (25.8%) |
| Gender | |||
| Male | 73 (49.7%) | 19 (61.3%) | 92 (51.7%) |
| Female | 74 (50.3%) | 11 (35.5%) | 85 (47.8%) |
| Missing | 0 (0%) | 1 (3.2%) | 1 (0.6%) |
| Health Status | |||
| Not Healthy | 18 (12.2%) | 10 (32.3%) | 28 (15.7%) |
| Healthy | 129 (87.8%) | 21 (67.7%) | 150 (84.3%) |
| DMFT at ART Placement | |||
| ≤ 2 | 34 (23.1%) | 8 (25.8%) | 42 (23.6%) |
| 3-4 | 43 (29.3%) | 6 (19.4%) | 49 (27.5%) |
| 5+ | 54 (36.7%) | 13 (41.9%) | 67 (37.6%) |
| Missing | 16 (10.9%) | 4 (12.9%) | 20 (11.2%) |
| Tooth location of ART | |||
| Anterior | 38 (25.9%) | 4 (12.9%) | 42 (23.6%) |
| Posterior | 108 (73.5%) | 27 (87.1%) | 135 (75.8%) |
| Missing | 1 (0.7%) | 0 (0%) | 1 (0.6%) |
| Number of Surfaces with ART | |||
| 1 | 60 (40.8%) | 9 (29%) | 69 (38.8%) |
| 2 | 69 (46.9%) | 20 (64.5%) | 89 (50%) |
| 3+ | 18 (12.2%) | 2 (6.5%) | 20 (11.2%) |
Table 1: Demographic and dental variables of study population who were treated with atraumatic restorative treatment (ART).
The earliest recording of an ART placement was in February 2000 and the final placement was recorded in 2009. For the study population, time between initial ART placement and the final visit ranged from 16 days to 8.34 years with an average time span of 2.6 years (SD=1.7). The number of recall appointments after initial ART placement ranged from one to 11 with an average of 3.5 appointments (SD=2.5). Time from initial ART placement to first subsequent recall ranged from 16 days to 4.4 years with an average of 0.8 years (SD=0.8) (Data not shown).
Survival analysis
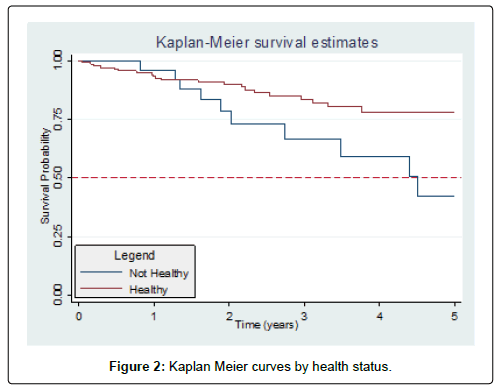
The overall 5-year survival rate of teeth receiving ART was 69.5% and the median survival time was 8.3 years. (Figure 1) Associations between the demographic and dental variables are presented in Table 2. Age, gender, baseline DMFT/dmft, tooth location, and number of ART surfaces were not associated with ART failure. The only variable found to have a significant association with tooth survival was health status of the child (p=0.027) (Table 2 and Figure 2). After adjusting for age, there is a 131% increase in the risk of ART failure among not healthy children (ASA II or higher) as compared to healthy children with (ASA I) (HR=2.31, 95% CI: 1.10, 4.84) (Table 2).
| Unadjusted Model | Adjusted Model* | |||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p-value | HR | 95% CI | p-value | |
| Age at ART Placement | 0.337 | 0.437 | ||||
| 0-2 | reference | reference | ||||
| 3-6 | 0.70 | (0.24, 2.04) | 0.512 | 0.66 | (0.22, 2.03) | 0.474 |
| 7-12 | 1.25 | (0.39, 4.04) | 0.706 | 1.08 | (0.32, 3.67) | 0.905 |
| Gender | 0.351 | 0.665 | ||||
| Male | reference | reference | ||||
| Female | 0.70 | (0.33, 1.47) | 0.351 | 0.85 | (0.40, 1.78) | 0.665 |
| Health Status | 0.015 | 0.027 | ||||
| Healthy | reference | reference | ||||
| Not Healthy | 2.40 | (1.19, 4.86) | 0.015 | 2.31 | (1.10, 4.84) | 0.027 |
| DMFT at ART Placement | 0.576 | 0.749 | ||||
| ≤ 2 | reference | reference | ||||
| 3-4 | 0.58 | (0.20, 1.66) | 0.308 | 0.66 | (0.21, 1.99) | 0.455 |
| 5+ | 0.87 | (0.36, 2.10) | 0.757 | 0.88 | (0.34, 2.30) | 0.800 |
| Tooth location of ART | 0.163 | 0.059 | ||||
| Anterior | reference | reference | ||||
| Posterior | 2.14 | (0.73, 6.24) | 0.163 | 2.85 | (0.96, 8.45) | 0.059 |
| Number of Surfaces with ART | 0.132 | 0.213 | ||||
| 1 | reference | reference | ||||
| 2 | 2.00 | (0.94, 4.27) | 0.073 | 1.86 | (0.80, 4.36) | 0.151 |
| 3+ | 0.78 | (0.16, 3.76) | 0.754 | 0.72 | (0.14, 3.69) | 0.693 |
Table 2: Unadjusted and adjusted hazard ratios (HR) from cox proportional hazard regression with robust standard errors.
Discussion
The strength of this study relies on its primary outcome: rather than targeting the survival time of ART restorations, we aimed to investigate the 5-year survival rate of primary teeth and young permanent teeth receiving this therapy. We found a long median survival time of 8.3 years that is substantially different when compared with previous studies [2,7]. There are several factors that could affect the results that are worthy of discussion. Since the 1990s, high viscosity glass ionomer cements have traditionally been the material of choice for ART restorations due to their superior physical properties [16-18]. In this study, Vitrebond™, a low viscosity resin modified glass ionomer cement, was used for ART restorations. Although this material is marketed as a liner, properties include the ability to adapt to the cavity preparation, release fluoride, adhere to the dentin and enamel, and provide effective sealing of dentinal tubules. These factors and its biocompatibility may have attributed to the significant long survival for the restorations [19-22]. Another factor to consider is continuity of care in this lowincome community who had limited access to dental care during this study period. Children were followed up by the same two providers increasing treatment effectiveness by allowing regular assessment and as needed replenishment of the ART restoration material.
Similarly to previous studies, we did not find significant difference in survival rates between age, position of the tooth (anterior vs. posterior teeth), or gender [7]. Our results differ when assessing the association of ART success and multi-surface restorations: we did not find significant difference in survival rates of primary teeth receiving a single versus multi-surface ART restorations [23-25]. We believe this is explained by the fact that our study population received replenishment of the ART restoration as needed at their follow up appointments, therefore teeth were resealed and recharged, resulting in release of fluoride into adjacent tooth structure, factors known to increase the success rate of ART restorations [10].
In the 1999-2004 National Health and Nutrition Examination Survey (NHANES), children aged two to 11 had a caries prevalence of 42% and an average decayed or filled primary teeth (dft) score of 1.6 [26]. In the present study, children were seen from 2000 to 2009, ranged from 10 months to 12 years old, and had an average dmft/DMFT of 4.5 (SD=2.7). While dmft/DMFT is nearly three times higher than the national average at that time, it was not associated with the survival rate of the ART restoration. This is similar to the findings from Farag et al. where DMFT did not have any effect on the cumulative survival percentages of all ART restorations over five years of evaluation among adolescents [27].
We also found a significant difference in survival rates between healthy children (ASA I) and not healthy children (ASA II or more) with the former having longer survival time than the latter (Table 2 and Figure 2). One plausible explanation might be that families with children who have compromised health and development face more challenges in adhering to the recommended preventative regimes, including oral hygiene, dietary control, and regular dental appointments.
There are several limitations in the current study. First, because the database originated from a general dental practice, no specific clinical criteria for reliability of treatable lesion characteristics were described before the initial ART placement. Second, the dental charts did not include a description of the ART restoration regarding its marginal integrity, degree of wear and the reason for ART re-placement. Additionally, it was unclear whether there was recurrent caries, advancement of caries, new caries on different surfaces after the initial ART placement, or whether the re-placement was due to wear or loss of retention. Furthermore, because of the inconsistency in the availability of radiographs, we were unable to have a systematic radiographic evaluation. For that reason, radiographs were only used to estimate the date of exfoliation when it was not clearly registered in the dental chart. Finally, the present study shows that more than two-thirds of teeth treated with ART survived more than 5 years. We believe the long median survival time is related to the low overall ART failure rate. All these factors likely influenced the longer survival time of ART in these children.
Interestingly, these limitations may also support the success of this technique when used in a real-world setting. Specifically, this study defines hard outcomes (tooth survival) that are of interest to general dentists and proposes that by replenishing the lesion with ART material, success of the technique can be positively impacted. To our knowledge, this paper is the first study utilizing a database of a general dental practice in a rural geographical area demonstrating a long median survival time of teeth that were treated with ART. The ART technique provides general practitioners and pediatric dentists with a successful method for managing dental caries when conventional treatment is not possible.
Conclusion
A long median survival time of teeth treated with ART was observed in this study. Specifically, healthy children had significantly longer survival rates for primary teeth treated with ART than those who were medically compromised. Finally, replenishing ART is an effective method to treat primary teeth with caries until their natural exfoliation or until a permanent restoration can be placed.
Conflict of Interest
The authors have no conflicts of interest.
Acknowledgment
We would like to express our gratitude to the University Of Washington Department Of Paediatric Dentistry for supporting this project by funding transportation and delivery of the paper database.
References
- Frencken JE, Truin GJ, van't Hof MA, Konig KG, Mabelya L, et al (1990) Prevalence of dental caries in 7-13 year-old children in Morogoro District, Tanzania, in 1984, 1986, and 1988. Community Dent Oral Epidemiol 18: 2-8.
- Frencken JE, Leal SC, Navarro MF (2012) Twenty-five-year atraumatic restorative treatment (ART) approach: a comprehensive overview. Clin Oral Investig 16: 1337-1346.
- Taifour D, Frencken JE, Beiruti N, van 't Hof MA, Truin GJ (2002) Effectiveness of glass-ionomer (ART) and amalgam restorations in the deciduous dentition: results after 3 years. Caries Res 36: 437-444.
- Frencken JE, Pilot T, Songpaisan Y, Phantumvanit P (1996) Atraumatic restorative treatment (ART): rationale, technique, and development. J Public Health Dent. 56:135-140.
- Petersen PE, Bourgeois D, Ogawa H, Estupinan-Day S, Ndiaye C (2005) The global burden of oral diseases and risks to oral health. Bull World Health Organ 83: 661-669.
- de Amorim RG, Leal SC, Frencken JE (2012) Survival of atraumatic restorative treatment (ART) sealants and restorations: a meta-analysis. Clin Oral Investig 16: 429-441.
- Faccin ES, Ferreira SH, Kramer PF, Ardenghi TM, Feldens CA (2009) Clinical performance of ART restorations in primary teeth: A survival analysis. J Clin Pediatr Dent 33: 295-298.
- Schriks MC, van Amerongen WE (2003) Atraumatic perspectives of ART: Psychological and physiological aspects of treatment with and without rotary instruments. Community Dent Oral Epidemiol 31: 15-20.
- de Menezes Abreu DM, Leal SC, Frencken JE (2009) Self-report of pain in children treated according to the atraumatic restorative treatment and the conventional restorative treatment--a pilot study. J Clin Pediatr Dent 34: 151-555.
- Mickenautsch S, Grossman E (2006) Atraumatic restorative treatment (ART): Factors affecting success. J Appl Oral Sci 14: 34-36.
- No Autors Listed (2016) Policy on Interim Therapeutic Restorations (ITR). Pediatr Dent 38: 50-51.
- Lee GH, McGrath C, Yiu CK (2013) The care of the primary dentition by general dental practitioners and paediatric dentists. Int Dent J 63: 273-280.
- Tickle M, Threlfall AG, Pilkington L, Milsom KM, Duggal MS, et al (2007) Approaches taken to the treatment of young children with carious primary teeth: A national cross-sectional survey of general dental practitioners and paediatric specialists in England. Br Dent J 203: 102-103.
- Peterson D, Kaakko T, Smart E, Jorgenson M, Herzog C (2007) Dental students attitudes regarding online education in pediatric dentistry. J Dent Child (Chic) 74: 10-20.
- Tinanoff N, Coll JA, Dhar V, Maas WR, Chhibber S, et al. (2015) Evidence-based update of pediatric dental restorative procedures: Preventive strategies. J Clin Pediatr Dent Spring 39: 193-197.
- Luengas-Quintero E, Frencken JE, Munuzuri-Hernandez JA, Mulder J (2013) The atraumatic restorative treatment (ART) strategy in Mexico: two-years follow up of ART sealants and restorations. BMC Oral Health 13: 42.
- Bonifacio CC, Kleverlaan CJ, Raggio DP, Werner A, de Carvalho RC, et al. (2009) Physical- mechanical properties of glass ionomer cements indicated for atraumatic restorative treatment. Aust Dent J 54: 233-237.
- Frencken JE, Holmgren CJ (2013) Caries management through the Atraumatic Restorative Treatment (ART) approach and glass-ionomers: Update 2013. Braz Oral Res 28: 5-8.
- Chadwick RG, Woolford MJ (1993) A comparison of the shear bond strengths to a resin composite of two conventional and two resin-modified glass polyalkenoate (ionomer) cements. J Dent 21: 111-116.
- Prabhakar AR, Subhadra HN, Kurthukoti AJ, Shubha AB (2008) Sealing ability and thermal diffusivity of cavity lining materials: an in vitro study. J Indian Soc Pedod Prev Dent 2: S62-S67.
- Hse KM, Leung SK, Wei SH (1999) Resin-ionomer restorative materials for children: A review. Aust Dent J 44 (1): 1-11.
- Croll TP (1990) Glass ionomers for infants, children, and adolescents. J Am Dent Assoc 120: 65-68.
- Lo EC, Luo Y, Fan MW, Wei SH (2001) Clinical investigation of two glass-ionomer restoratives used with the atraumatic restorative treatment approach in China: Two-years results. Caries Res 35: 458-463.
- van't Hof MA, Frencken JE, van Palenstein Helderman WH, Holmgren CJ (2006) The atraumatic restorative treatment (ART) approach for managing dental caries: A meta-analysis. Int Dent J 56: 345-351.
- Yu C, Gao XJ, Deng DM, Yip HK, Smales RJ (2004) Survival of glass ionomer restorations placed in primary molars using atraumatic restorative treatment (ART) and conventional cavity preparations: 2-year results. Int Dent J 54: 42-46.
- No Authors Listed (2014) Dental caries (tooth decay) in children (age 2 to 11). NIDCR.
- Farag A, van der Sanden WJ, Abdelwahab H, Mulder J, Frencken JE (2009) 5-year survival of ART restorations with and without cavity disinfection. J Dent 37: 468-474.
Relevant Topics
- Advanced Bleeding Gums
- Advanced Receeding Gums
- Bleeding Gums
- Children’s Oral Health
- Coronal Fracture
- Dental Anestheia and Sedation
- Dental Plaque
- Dental Radiology
- Dentistry and Diabetes
- Fluoride Treatments
- Gum Cancer
- Gum Infection
- Occlusal Splint
- Oral and Maxillofacial Pathology
- Oral Hygiene
- Oral Hygiene Blogs
- Oral Hygiene Case Reports
- Oral Hygiene Practice
- Oral Leukoplakia
- Oral Microbiome
- Oral Rehydration
- Oral Surgery Special Issue
- Orthodontistry
- Periodontal Disease Management
- Periodontistry
- Root Canal Treatment
- Tele-Dentistry
Recommended Journals
Article Tools
Article Usage
- Total views: 4587
- [From(publication date):
September-2017 - Apr 24, 2025] - Breakdown by view type
- HTML page views : 3574
- PDF downloads : 1013