Surgical Treatment of Transplant Renal Artery Aneurysm: Case Report and Review of Literature
Received: 26-Jun-2017 / Accepted Date: 24-Aug-2017 / Published Date: 01-Sep-2016 DOI: 10.4172/2475-7640.1000108
Abstract
Authors report a case of transplant renal artery aneurysm. The aneurysm developed within three months of living unrelated kidney transplantation surgery. The aneurysm involved origin of the transplant renal artery proximally and extended up to its bifurcation. The aneurysm was not amenable to endovascular corrective approach. Surgical resection of the aneurysm was carried out; renal arteries were repaired and re-anastomosed with the right iliac artery. Allograft function recovered after a brief period of acute kidney injury. His kidney function remains stable one year post transplant renal artery repair. A brief review of literature related to the etiology and management of such cases is presented.
Case
A 36-year old male with history of polycystic kidney disease and hypertension underwent living unrelated, commercial, kidney transplantation on 28 November 2014. His post-operative course after the transplant surgery was unremarkable. Patient returned to his hometown and was followed up at a center close to his home. His serum creatinine was between 110-120 μm/L. As is commonly observed with commercial transplant surgeries, there was no available information on donor, immunological and induction immunosuppression nor any surgical details such as vascular trauma during donor nephrectomy or transplantation. His initial ultrasound and Doppler examination of the transplant kidney was reported normal. On a follow up visit, the edge of surgical wound was noted to be erythematous and his serum creatinine was noted to be higher than baseline. The surgical clips at the erythematous area were removed and wound was partly opened at unhealthy site. Empiric antibiotics were started. Due to further increase in serum creatinine a repeat ultrasound and Doppler examination was performed which revealed aneurysmal dilatation of the transplant renal artery. Possibility of fungal infection and the risk of rupture of aneurysm were explained to the patient and transplant nephrectomy was suggested. The patient was referred to our center for another opinion.
Upon arrival to our center, on 02 February 2015, he was afebrile with blood pressure of 172/97 mmHg. He weighed 109 kg with height of 178 cm. His body mass index was 34.4. There was small area of unhealed wound at one end of the scar of surgery and rest of the wound had healed. There was no discharge from the wound. There was no swelling, tenderness or audible bruit over the allograft. Rest of the physical examination was unremarkable. Urine, blood and wound swabs were collected for microbiological examination, including fungal cultures. Empiric treatment with caspofungin was started along with broad spectrum antibiotics. Ultrasound and Doppler examination revealed normal allograft of 12.7 cm with normal echogenicity and good perfusion. Ureteric stent was in place. There was no perinephric collection. A 1.9 cm fusiform aneurysmal dilatation was noted in the transplant renal artery. His immunosuppression included prednisone, mycophenolate mofetil and cyclosporin. He was on norfloxacin and co-trimoxazole for antibiotic prophylaxis. He was taking valganciclovir for antiviral and fluconazole for antibacterial prophylaxis. His blood pressure was controlled on labetalol 300 mg orally three times daily, amlodipine 10 mg orally once daily, hydralazine 100 mg orally three times daily and furosemide 40 mg orally daily.
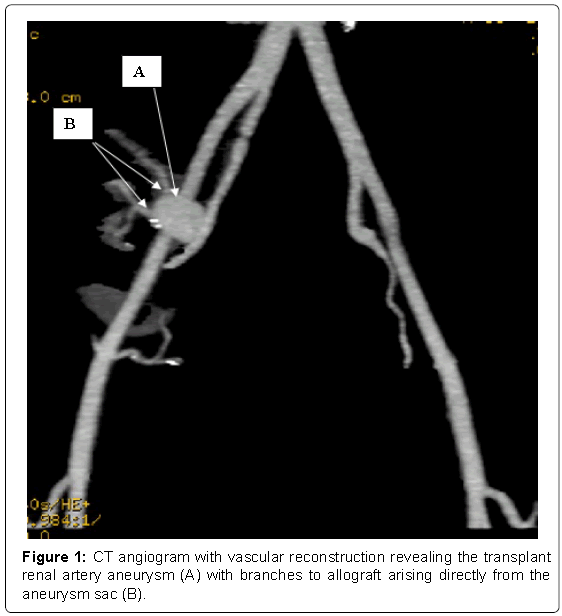
Transplant renal angiogram was performed on 11 February 2015, from left common femoral artery approach crossing over to the right side. Angiogram revealed a 2 × 2.5 cm true aneurysm starting from the anastomosis. At this point right common femoral artery approach was made in a retrograde fashion and aneurysm was entered. Angiogram from the aneurysm revealed that the branches of the renal artery were originating directly from the aneurismal sac. The aneurysm was not amenable to stenting or embolization by endovascular approach. Computerized axial tomogrophic (CT) angiogram was performed with digital vascular reconstruction, which revealed minimal perinephric fluid and fat stranding. The aneurysm was measuring 2.6 cm × 2.1 cm, and as shown on angiographic examination, it spanned the whole length of the vessel with branches emanating from the sac (Figure 1). CT scan also revealed native polycystic kidneys. The rest of the abdominal organs were normal.
Microbiological tests for bacteria and fungus were negative. The risk of leaving the aneurysm alone and catastrophic event, such as rupture, thrombosis and loss of graft were explained to the patient. Surgery was the only option with possibility of aneurysm resection, vascular reconstruction and re-implantation. Patient was made aware that there may be intra-operative bleeding and if fungus infection is suspected intraoperatively then allograft nephrectomy will be inevitable.
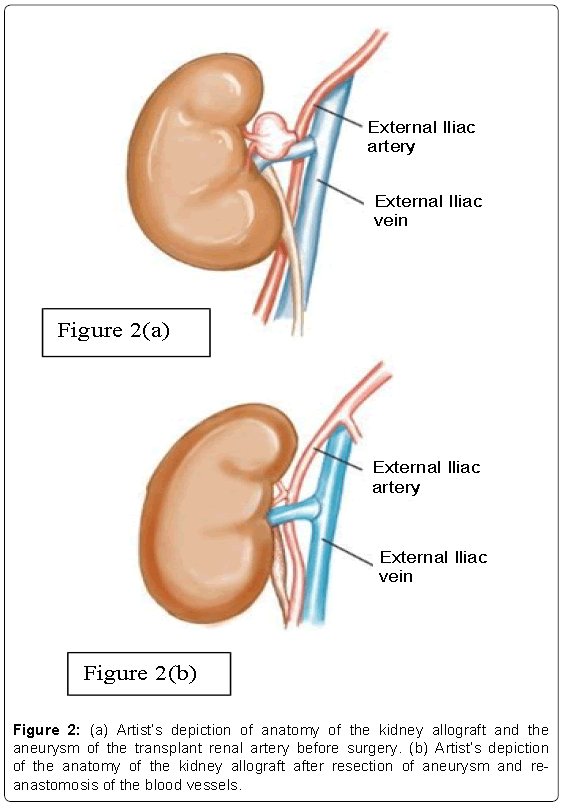
After much hesitation and deliberation, the patient underwent surgery on 8th March 2015 through lower midline incision. The transplanted kidney with its associated structures were identified. The graft was markedly adherent to the retroperitoneum and anterior abdominal wall. Mobilization of the graft was minimized to avoid injury to the graft. A 2 cm aneurysm of renal artery was noted originating from the external iliac artery anastomosis up to the hilum of the kidney (Figure 2a). Graft renal vein was closely adherent to the aneurysm. The proximal and distal external iliac artery and vein were isolated to control graft inflow and outflow. The graft ureter was identified and secured to avoid injury. At this point 1500 units of heparin was given intravenously and then the external iliac artery and vein were clamped proximal and distal to the graft vascular anastomoses. Arteriotomy of the aneurysm was carried out. Graft was heparinized and flushed insitu with cold HTK solution, draining the outflow through a venotomy of the graft renal vein leaving the renal vein anastomosis intact. The wall of the aneurysm did not appear to be infected or inflamed. At the level of the hilum the aneurysm cuff was divided and direct implantation between the hilar cuff and the prior external iliac arteriotomy was done; ensuring a tension free, full thickness arterial anastomosis with 6-0 running vascular stitch (Figure 2b). Graft ischemia time was 20 min. Intra-operative Doppler examination was performed to ensure good perfusion to the kidney allograft. Operative time was 190 min with estimated blood loss of 300 mL. There was no inflammation or fungal elements seen on histology of the resected material. Wound was sutured in layers.
Post-operatively the patient was oliguric for a few hours. Ultrasound and Doppler examination revealed good flow and perfusion to the kidney allograft. There was no perinephric collection. Patient started to produce urine the next day. His serum creatinine peaked to 398 μm/L by post-operative day 4 before it started to improve with out renal replacement therapy.
At his last follow up one-year after the surgical resection of the aneurysm, his serum creatinine has been stable at 120-130 μm/L. His blood pressure is controlled with labetalol 300 mg orally three times daily and hydralazine 100 mg orally three times daily.
Discussion
Transplant renal artery aneurysm (TRA) is a rare complication with a reported incidence of 0.3% [1,2]. This complication is rare but, if untreated, may lead to potentially catastrophic consequences, such as rupture, thrombosis, renal infarction and loss of graft and death. Atherosclerosis, vascular trauma during angioplasty or stenting and injury related to kidney biopsy and vasculitis are common causes of renal artery aneurysms in non-transplant subjects. Infections, particularly fungal infections, trauma to the renal artery during harvesting are known causes of such aneurysms in patients with transplant kidneys [3-5]. Shortage of organs has pressurized clinicians to accept organs from deceased donors with longer stays in the intensive care units on antibiotic therapy. Such donors may have undetected fungal infection at the time of harvesting and later may manifest as mycotic aneurysm. More importantly, tighter control on organ trade in many countries has led to unauthorized transplant activity. Most such activity takes place in poor environment not suitable for surgical procedures, hence increasing the risk of bacterial and fungal infections. Additionally, organ shortage has also lead to use of surgically challenging organs such as kidney with renal artery aneurysm. The aneurysm can be repaired on the back table before the kidney is transplanted [6]. Patients with autosomal dominant polycystic kidney disease (ADPKD) are known to have vascular aneurysms more frequently than what is observed in the general population. Our case, and a previously reported case by Al-Wahaibi et al. where the recipient suffered from ADPKD [7]. It is possibly a coincidence, as the aneurysm developed in the donor vessel. Patients susceptible to develop vascular aneurysms, such as Ehlers- Danlos syndrome, Marfan syndrome or Klinefelter syndrome are not considered to have contraindications for kidney donation as long as they have no evidence of kidney disease. There is limited available information in the literature, in the form of case reports, on surgical outcomes of kidney donors with these disorders [8,9]. In our case donor information related to these syndromes was not available.
Clinical presentation of transplant renal artery aneurysm varies from no symptoms to increasing blood pressure, rise in serum creatinine, and development of pain at the allograft site, fever and shock due to infection or bleeding from the aneurysm.
Those kidney allograft recipients who develop this complication have options of endovascular or open surgical procedure. These aneurysms often pose difficulty in management due to early division of the artery, being close to the hilum of the allograft and adhesions related to primary transplant surgery. Allograft nephrectomy is avoidable in a limited number of cases when there is no active infection, surgery is technically feasible and experienced transplant surgical team with support services are in place. Non surgical or interventional radiological approach is less invasive. The draw back of such approach is that it may overlook a fungal infection, as opposed to open surgery where a close inspection and even per-operative biopsy may be performed for confirmation. Deployment of a stent or filler in an infected vessel may only prolong the inevitable and may give false sense of security to the treating team. In cases where the renal artery’s main divisions appear to arise from the aneurismal sac, two stents may be deployed in each division of the renal artery. This however, requires adequate landing space proximally and is technically difficult if the origin of the aneurysm is too narrow or wide. Risk of rupture of the aneurysm and need for embolization and emergency surgery remains a possibility.
Open surgical approach has the advantage of better identification of the anatomical structures, assessment of the possibility of infection of the surrounding tissue and involved vessels, control of the vessels and perfusion of the kidney allograft during the procedure to minimize risk of acute kidney injury post operatively. In case where aneurysmectomy may result in shortened artery, venous graft may be used for vascular re-anastomosis.
References
- Dimitroulis D,Bokos J, Zavos G, Nikiteas N, Karidis NP, et al. (2009) Vascular Complications in Renal Transplantation: A Single-Center Experience in 1367 Renal Transplantations and Review of the Literature.Transplantation Proc41: 1609-1614.
- Parada B, Figueiredo A, Mota A, Furtado A (2003) Surgical complications in 1000 renal transplants. Transplant Proc 35: 1085-1086.
- Laouad I, Buchler M, Noel C, Sadek T, Maazouz H, et al. (2005) Renal artery aneurysm seconday to candida albicans in four kidney allograft recipients. Transplant Proc 37: 2834-2836.
- Henderson A, Pall AA, Chakarverty S (2007) Unsuspected mycotic aneurysm of renal transplant artery. Kidney International 72: 775-776.
- Meybodi NT, Amouian S, Mohammadian-Roashan N (2005)Renal allograft mucormycosis: Report of two cases. Urol J 2: 54-56.
- Gravante G, Pisani F,D’Angelo M, Iaria G, Orlando G (2008)Renal artery aneurysms in kidney grafts. Am J Surg 196: e46-e47.
- Al-Wahaibi KN, Aquil S, Al-Sukaiti R, Al-Riyami D, Al-Busaidi Q (2010) Transplant renal artery false aneurysm: Case report and literature review. Oman Med J 5: 306-310.
- Farese S, Vogt B, Frey FJ, Huynh-Do U (2006) Successful kidney transplantation from Donor with Marfan’s Syndrome. Am J Transplant 6: 1972-1974.
- Thomson SD, Chmura AM, Slapak M (1995)Renalautotransplantation for aortic dissection in Marfan’s Syndrome. J R Soc Med 88: 532-533
Citation: Farooqui MA, O’Hali WA, Muaikeel M, Akhtar MN, Qurashi S, et al. (2016) Surgical Treatment of Transplant Renal Artery Aneurysm: Case Report and Review of Literature. J Clin Exp Transplant 1: 108. DOI: 10.4172/2475-7640.1000108
Copyright: © 2016 Farooqui MA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 13391
- [From(publication date): 11-2016 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 12490
- PDF downloads: 901