Commentary Open Access
Surgery for Severe Acute Necrotizing Pancreatitis – Which is the Best Procedure?
Rahul Gupta*Senior Resident, General Surgery, Chandigarh, India
- *Corresponding Author:
- Rahul Gupta
Senior Resident, PGIMER
General Surgery Sector 12
Chandigarh 160012, India
Tel: 919914209649
E-mail: rahul.g.85@gmail.com
Received date: March 17, 2014; Accepted date: May 19, 2014; Published date: May 25, 2014
Citation: Gupta R (2014) Surgery for Severe Acute Necrotizing Pancreatitis – Which is the Best Procedure?. J Gastroint Dig Syst 4:185. doi:10.4172/2161-069X.1000185
Copyright: © 2014 Gupta R. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Surgical management of acute necrotizing pancreatitis is rapidly evolving with newer minimally invasive techniques replacing traditional open necrosectomy as the preferred surgical procedure at various centres worldwide. But one needs to take in to account multiple factors while choosing the most appropriate procedure for a given patient. Also one needs to plan based on the clinical condition of the patient and the timing of intervention that whether patient will benefit from ‘Step up approach’ or primary necrosectomy. These critical issues have been discussed so as to facilitate clinical decision making and importance of multidisciplinary team is highlighted in order to reduce morbidity and mortality associated with severe acute necrotizing pancreatitis.
Keywords
Acute necrotizing pancreatitis; Necrosectomy; Step up approach; Walled off pancreatic necrosis
Commentary
Recently, various minimally invasive techniques [MIT] have been described for acute necrotizing pancreatitis [ANP] which has better outcomes compared to open necrosectomy [OP] [1,2]. But one needs to understand that there is lot of heterogeneity in the current data to make any conclusion favouring any of the techniques. Also none of these MIT can be universally used in all patients unlike open necrosectomy. Hence appropriate patient selection is important. Another important factor to be considered during selection is time of intervention from the onset of pancreatitis. Most of the MIT have been shown to be safe and effective when performed 4-6 weeks after the onset of pancreatitis i.e. after development of walled off pancreatic necrosis [WOPN]. If the patient has worsening of clinical condition despite supportive care before that with large (peri) pancreatic collections, percutaneous catheter drainage [PCD] is considered. This so called ‘Step up approach’ helps in drainage of liquefied pus under tension as well as act as guide for future necrosectomy [3]. Attempt is made to drain all the drainable collections. If the condition of the patient continues to improve, necrosectomy is deferred. If there is no improvement, repeat imaging should be done preferably contrast enhanced computed tomography [CECT] to identify the extent and location of the residual collections. For residual collections in paracolic gutters, minimal access retroperitoneal necrosectomy would be appropriate procedure [2]. Retroperitoneal approach can also be used for debriding (peri) pancreatic collections in communication with paracolic gutters. In situations where (peri) pancreatic collections are not accessible from retroperitoneum, open necrosectomy should be considered.
Endoscopic drainage followed by direct endoscopic necrosectomy can also be considered as an alternative approach. This approach is most suitable for WOPN located abutting the posterior wall of stomach provided there is availability of equipments and expertise. This can also be combined with PCD of collections located in paracolic gutters followed by retroperitoneal necrosectomy in order to achieve faster recovery [4]. In this way, multiple MIT can complement each other to enhance recovery.
Laparoscopic necrosectomy is a feasible option for patients with symptomatic WOPN in absence of organ failure. It has advantage in patients with gallstone disease as cholecystectomy can be simultaneously performed in the same sitting.
An important issue which needs to be considered while deciding on the treatment plan is the type of anaesthesia required to perform the procedure as it has been shown to significant impact on the organ functions of these sick patients [5]. In patients with organ failure, PCD or endoscopic drainage is preferred as they can be done under local anaesthesia or sedation. In otherwise stable patients who can tolerate general anaesthesia without untoward impact, minimal access techniques can provide better drainage with fewer complications.
Patients who fail to respond to MIT or develop complications like bleeding, bowel ischemia, require open necrosectomy. Also where facilities for MIT are not available, open necrosectomy should be performed.
The main determinant of outcome in these patients after any intervention is presence or absence of distant organ failure at the time of intervention as shown in various studies [6]. Hence every effort should be made to improve the organ functions preoperatively by percutaneous or endoscopic drainage and reduce septic load.
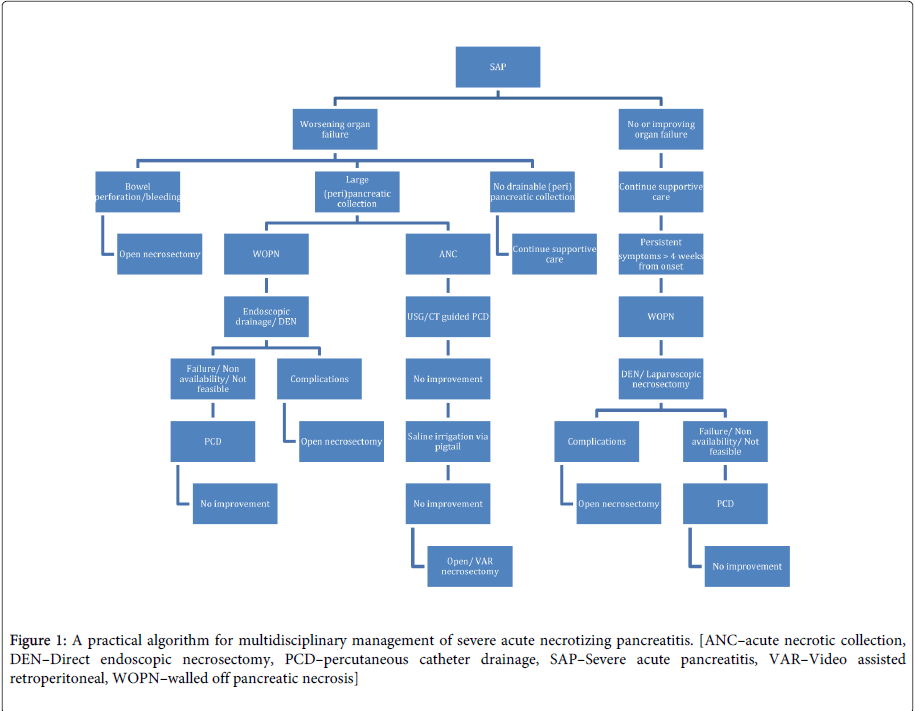
To conclude, a multidisciplinary team of surgeon, interventional radiologist and gastroenterologist is required to provide individualised treatment to each patient of SAP based on the clinical condition, radiology findings and availability of equipments and expertise. A practical algorithm depicted in Figure 1 can be useful in constructing the treatment plan.
Figure 1: A practical algorithm for multidisciplinary management of severe acute necrotizing pancreatitis. [ANC–acute necrotic collection, DEN–Direct endoscopic necrosectomy, PCD–percutaneous catheter drainage, SAP–Severe acute pancreatitis, VAR–Video assisted retroperitoneal, WOPN–walled off pancreatic necrosis]
References
- Babu BI, Siriwardena AK (2009) Current status of minimally invasive necrosectomy for post-inflammatory pancreatic necrosis. HPB (Oxford) 11: 96-102.
- Raraty MG, Halloran CM, Dodd S, Ghaneh P, Connor S, et al. (2010) Minimal access retroperitoneal pancreatic necrosectomy: improvement in morbidity and mortality with a less invasive approach. Ann Surg 251: 787-793.
- van Santvoort HC, Besselink MG, Bakker OJ, Hofker HS, Boermeester MA, et al. (2010) A step-up approach or open necrosectomy for necrotizing pancreatitis. N Engl J Med 362: 1491-1502.
- Gluck M, Ross A, Irani S, Lin O, Ian Gan S, et al. (2012) Dual modality drainage for symptomatic walled-off pancreatic necrosis reduces length of hospitalization, radiological procedures, and number of endoscopies compared to standard percutaneous drainage. J GastrointestSurg 16:248–257.
- Golubovska I, Vanags I. (2008) Anaesthesia and stress response to surgery. Proceedings of the Latvian academy of sciences 62:141–147.
- Connor S, Ghaneh P, Raraty M, Rosso E, Hartley MN, et al. (2003) Increasing age and APACHE II scores are the main determinants of outcome from pancreatic necrosectomy. Br J Surg 90: 1542-1548.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 15645
- [From(publication date):
June-2014 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 11089
- PDF downloads : 4556