Case Report Open Access
Supra Malleolar Osteotomies for Neglected Tibial Deformity Affecting the Ankle and Foot
Pasquale Cancelliere*DPM, MetroWest Medical Center, Framingham, MA, USA
- *Corresponding Author:
- Pasquale Cancelliere
DPM, Attending Surgeon, MetroWest Medical Center
Framingham, MA, USA
Tel: 1-978-810-5425
E-mail: drpc78@gmail.com
Received date:January 30, 2016; Accepted date: March 27, 2016; Published date: March 31, 2016
Citation: Cancelliere P (2016) ��?Supra Malleolar Osteotomies for Neglected Tibial Deformity Affecting the Ankle and Foot�. Clin Res Foot Ankle 4:192. doi:10.4172/2329-910X.1000192
Copyright: © 2016 Cancelliere P. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Clinical Research on Foot & Ankle
Abstract
Ankle arthrosis continues to affect millions of people worldwide. Whereas it is not as common as hip and knee arthrosis in the aging population, it is more and more prevalent in the younger population. Also, it is not uncommon to see total destruction of the ankle joint in the neuropathic population. Whereas arthrosis of the knee and hip is mostly “wear and tear” type, the vast majority of ankle arthrosis is post traumatic. Because of this the likely hood of an underlying post traumatic deformity is high. Post Traumatic Deformity is often disabling particularly in the case of osteomyelitis treatment and open fractures with bone loss. This leads to a painful, non plantigrade, non functional limb. Consequently, the surgeon needs to perform complete and methodic pre-operative planning prior to performing any definitive reconstructive joint surgery.
Ankle arthrodesis continues to be the standard of care for end stage ankle arthrosis. It is a tried and true procedure that provides the surgeon and patient, predictable union rates, low rate of complications and ultimately, gives acceptable AOFAS score, indicating a good post-surgical quality of life to the patient. However, arthrodesis is not without disadvantages. Over the last 10 years, however total ankle replacement (TAR), has become a growing and more widely accepted alternative to arthrodesis. New systems have improved instrumentation, shorter operating room time and fewer complications as well as improved functional outcomes. This procedure is also not without significant possible complications and disadvantages. Also, distraction ankle arthroplasty has shown to provide favorable short term and medium term favorable outcomes.
However, regardless of the procedure selected by the surgeon and patient for the treatment of ankle arthritis, there is one principle that is ubiquitous but unfortunately often overlooked. This iatrogenic negligence leads to increased non-union rates, continued pain and ultimately loss of functionality of the limb. The authors of this paper have encountered several failed ankle arthrodeses and TAR’s because of this which required extensive revisional reconstructive surgery. Also, in the case of bony deformity, conservative measures such as braces, AFO’s will have disappointing results.
Introduction
Whether the surgeon and patient elect to proceed with a TAR or Ankle Arthrodesis, the objectives of the surgery remain grossly identical. The goal of arthrodesis or TAR is to relieve pain and restore a functional, plantigrade limb. Both procedures share the indication of curing painful end stage arthrosis of the ankle, after conservative measures have failed. The advantage of TAR over arthrodesis is that it restores some range of motion of the ankle and that it limits the extent of arthritis which develops in the adjacent joints [1,2]. Often this leads to requiring subsequent arthrodesis in those joints. In a study by Esprarragoza [3], the perceived quality of life of patients who had undergone TAR was superior to patients who underwent Arthrodesis. However, this study was based on preoperative AOFAS scores and post-operative AOFAS scores at an average of 25.2 months. With AOFAS scores taking into account range of motion, this unfairly favors arthroplasty. To date, ankle arthrodesis remains the gold standard for painful end stage arthrosis.
Also, although total ankle arthroplasty effectively relieves pain, it does restrict the patient from high impact activities such as running. Also the patient profile who is a good candidate for ankle replacement is much narrower than the patient profile for ankle arthrodesis. The most common disqualifier for patient seeking replacements in the authors’ practice is the neuropathic ankle.
However, both procedures, require one universal pre requisite in order for a good outcome. There must be no inherent deformity to the lower extremity. Both an ankle arthrodesis and TAR will not be successful if placed in a lower limb with a deviated mechanical axis, especially if the deformity exceeds the compensation available at the adjacent joints.
Preoperative Planning
In the authors’ practice, when evaluating a patient who might be a candidate for a hind foot arthrodesis or joint replacement, a specific protocol is followed every time in order to achieve an accurate diagnosis and appropriately treat the patient.
This has allowed for consistently favourable clinical outcomes.
A thorough and complete medical history exam is obtained. Factors that are of particular relevance are congenital versus acquired etiologies, comorbidities, lifestyle habits, and risk factors for postoperative complications and/or poor healing.
The second step involves static physical exam and gait analysis. Gait analysis should be methodic. It begins from observing overall symmetry in shoulder level, hip level, knee, and ankles.
Asymmetric circumduction of the hips and excessive unilateral arm swing should be noted.
Genu Valgum/Varum which exceeds anatomic limits, as well as knee hyperextension/flexion, equinus and calcaneal stance positions are all important.
During static exam, subtalar joint position, spherion height, knee level and hip level as well as limb torsion all need to be identified.
The next part of the exam is the radiographic exam. Full limb radiographs including the pelvis and foot are necessary to discern wither there is a femoral, tibial or combined deformity or limb length discrepancy.
Secondarily, weight bearing, full tibia radiographs including the tibial plateau and foot are paramount.
Both Frontal and Sagittal plane views are obtained. For the purposes of this chapter/article, we will outline the measurements taken and their clinical significance, along with treatment algorithm by the plane of the radiographs.
Anterior Posterior views will identify Varum/Valgum, whereas Sagittal view will identify and procurvatum, recurvatum deformities. We also obtain ankle AP, LAT and Long Leg Calcaneal Axial Views are obtained.
Frontal Plane View Radiographs
Commonly called the Anterior Posterior View, this radiographs primarily identify frontal plane deformity such as tibial Varum and Valgus.
In post-traumatic deformity, the most common will be Varum of the tibia. This is in the author’s experience due to two reasons primarily.
The first one being a consequence of Wolf ’s law where because of the imbalance between the posterior and medial muscle groups over powering the lateral group musculature, there is Varus pull at the fracture site during the healing process.
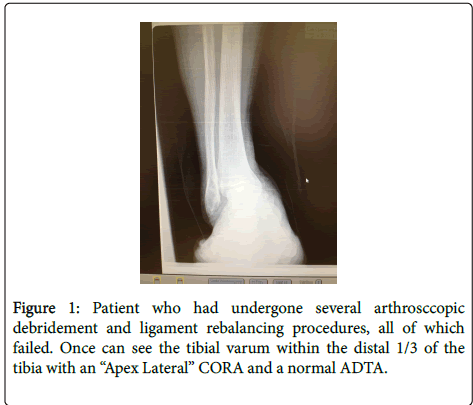
This will result in a seemingly apparent ankle varus deformity. In reality, if the surgeon takes the time to accurately measure the mechanical or anatomic axis of the tibia and ankle, it becomes apparent that many times the ankle joint will have a ADTA which is within normal limits and a CORA which is much more proximal (Figure 1).
Consequently surgeries such as ligament rebalancing techniques, ankle distraction, arthroscopy, will have limited and short lived success.
In the case of arthrodesis of the ankle and/or subtalar joint, the results will be disastrous, leaving the patients with a non plantigrade foot and worsening of pain and disability.
In the case of total ankle arthroplasty, it will result in accelerated and ultimately failure of the implant.
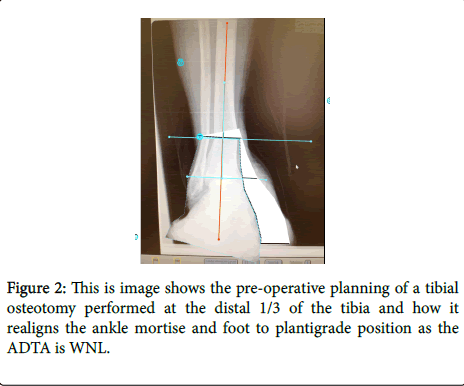
In this case, a low energy tibial osteotomy at the right level, depending on the quality of bone and soft tissue, thus following the principles of osteotomies, combined with external fixation will result in accurate correction of the deformity, restoring a plantigrade position and functional limb (Figure 2). We recommend a multiple drill hole and corticotomy technique in order to preserve endosteal blood flow and minimal peristomal damage. This will lead to accelerated healing and increased inherent stability to the osteotomy by leaving irregular edges to the bone regardless of whether the surgeon prefers and wedge type osteotomy or focal dome osteotomy. In the case of the wedge type osteotomy we recommend an opening type wedge as it will preserve or restore limb length.
Sagittal Plane View Radiographs
Recurvatum deformities are less tolerated and will accelerate wear and tear of an ankle implant rapidly due to increased shear forces versus procurvatum which lead to impingement/impaction type forces and will negate any benefits of soft tissue lengthening procedure to treat equinus.
At the ankle, Anterior Distal Tibial Angle and Lateral Distal Tibial Angles are measured. As both mechanical and anatomic axis in the tibia are parallel, it is up the surgeon which one of these is to be used as reference.
The measurements off the Calcaneal Axial view are primarily Calcaneal Translational or Varus/Valgus Angulation.
Only after all these angles have been accurately measured can preoperative planning take place and the exact osteotomy indicated for each single deformity is beyond the scope of this article/chapter.
Case Report
JM is a 13 year Male patient who presented to the author’s office for severe and debilitating pain of approximately 1 year duration. Patient has sustained a fall injury while playing on his grandparents’ trampoline. Since then he became less and less active and was complaining of severe pain to the Left leg, ankle and foot. His grandparents took him to see other specialists who had diagnosed him with ankle sprain and prescribed PT and splinting. After several trials, he did not improve satisfactorily and at the time of presentation he had completely withdrawn from physical activity and was severely demoralized. The patient had a history of psychiatric disease but was other otherwise healthy.On gait analysis, patient walked with a notable limb, pelvic and shoulder tilt and externally rotated tibia. Also, his Left foot remained in a pronated position the entire gait cycle, although it was reducible manually on non-weight bearing clinical exam with no clinical evidence of tarsal coalition. On radiograph evaluation a crush injury of the lateral aspect of the tibial episphysis was identified (Salter Harris V), which correlated with the clinical picture. The limb length discrepancy was measured clinically and with CT scan and measured at just above 2 cm.
I recommended to the patient and grandparents that he undergo corrective surgery and they could choose to undergo surgery immediately or after his growth plates had fused. However, it was explained to them that he would probably be suffering more and more pain to wait until then since his deformity would grow more severe and significant adaptive changes and arthrosis could set in. It was also explained to them however, that operating at this time could not guarantee that further surgery be required lateral on in life as his tibia and foot would continue to grow until 15-16 years of age. The patient and grandparents decided to undergo corrective surgery consisting of realignment calcaneal osteotomy, and tibial derotational osteotomy and lengthening. The tibial osteostomy was made through a small medial tibia incision at the level of the distal diaphysis-distal metaphyseal junction as this is typically the area where blood flow is the best. The fixator at this point had already been applied and wires tensioned. The osteotomy was made using a multiple drill hole corticotomy technique after carefully dissecting the periosteum. The derotation was made acutely on the operating room table.
Surgery was performed as stated with an external fixator and patient was allowed to weight bear immediately after surgery and limb lengthening was started at 1 week postoperatively, at a rate of 0.25mm four times a day for a total of 1 mm a day. Limb length equalization took 20 days and the external fixator was kept on for another 60 days to allow the regenerate bone to consolidate.
The external fixator used was the SEAL (System for External Alignment of Limbs, Allentown, PA) this system is a non-constrained external fixator system with corrective struts that allow for distraction/ compression. Also, the struts are attached to the rings via universal ball joints which allow for correction in all planes and axis. PT was maintained throughout the lengthening period to allow mobilization of the knee. The fixator was removed at that time and more PT was initiated to mobilize the ankle joint. At 3 month follow up, the patient was walking pain free with no insert required and no limitation in activity other than slight fatigue. This was attributable to the lengthy process wearing the external fixator. Both the patient and grandparents and the patient were extremely happy with their outcome. This is a good example of how once deformity has been accurately diagnosed, it can be corrected and thus restoring quality of life for patients. The deformity correction was joint sparing and because it was made prior to arthrosis and other adaptive changes, this patient will likely not require joint destructive surgeries in the future.
Discussion
Haskell [4] and Kim [5], in two independent studies showed that 33-44% of patients presenting for ankle replacement have greater than 10 degrees of coronal plane deformity. This is has mirrored the experience of the authors of this paper as well, in patients presenting for either replacement or arthrodesis. The ankle mortise is not an inherently congruent joint, and its stability is based on alignment of the mortise.
Even if there total compensation, particularly, in the case of the TAR, it will lead to accelerated degeneration of the implant, accelerated development of DJD in adjacent joints and decreased life span of the implant. In a mal united ankle arthrodesis, there is an even greater loss of compensatory motion and therefore, degeneration of adjacent joints will be accelerated.
Restoration of alignment in the coronal and sagittal planes to neutral is paramount. Kim [5] has postulated that ankle arthroplasty outcomes have been acceptable with as much as 10 to 15 degrees of coronal plane deformity. However, this is not acceptable in patients undergoing ankle arthrodesis. Varus (or apex lateral) deformity, will be particularly devastating as subtalar joint eversion does not afford the same degrees of compensation and will thus deteriorate rapidly. Coetzee [6] reported up to 50% failure of ankle replacement with greater than 20 degrees varus deformity. This will also lead to pathological compensation of the foot via supination further changing the ground reacting forces. Also the closer the deformity to the ankle joint, the greater of an effect it will have on the joint. Typically, procurvatum is more easily tolerated that recurvatum, as shear forces on the joint are increased in the case of ankle replacement. Also procurvatum is more easily compensated at the level of the knee joint.
Some surgeons recommend ligament augmentation or rebalancing procedures in the ankle replacement population. Whereas it has been ineffective in patients who have isolated ligament laxity or insufficiency, long term it is not a viable solution in the case of concomitant bone deformity.
Both TAR and Ankle Arthrodesis, and Ankle Distraction Arthroplasty have shown to have been effective procedures in alleviating pain from ankle arthritis. However, it is still incumbent on the surgeon to accurately examine the patient and correct any prior existing lower limb deformity. Complete tibia plain films, to include knee, tibia ankle and foot in sagittal and coronal views, and following the Ilizarov principles of deformity correction will identify underlying deformities. This will allow the surgeon to realize when a corrective osteotomy is required, either as a staged procedure or at the time of primary surgery. This will correct deforming forces in the ankle joint and allow for a functional, plantigrade foot long term.
References
- Keating JF, Blachut PA, O'Brien PJ, Court-Brown CM (2000) Reamed nailing of Gustilo grade-IIIB tibial fractures. J Bone Joint Surg 82:1113��?1116.
- Gopal S, Majumder S, Batchelor AG, Knight SL, De Boer P, et al. (2000) Fix and flap: the radical orthopaedic and plastic treatment of severe open fractures of the tibia. J Bone Joint Surg Br 82: 959-66.
- Esparragoza L, Vidal C, Vaquero J (2011) Comparative study of the quality of life between Arthrodesis and total ankle arthroplasty substitution of the ankle.J Foot Ankle Surg50: 383-387.
- Haskell A, Mann RA (2004) Ankle arthroplasty with preoperative coronal plane deformity.ClinOrthopRelat Res 424:98-103.
- Kim BS, Choi WJ, KIM YS, LEE JW(2009) Total ankle replacement in moderate to severe varus deformity of the ankle. J Bone Joint Surg 91:1183-1190.
- Coetzee JC (2008) Management ofvarus or valgus deformity in ankle replacement. Foot Ankle Clin13 :509-520
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 12598
- [From(publication date):
July-2016 - Apr 06, 2025] - Breakdown by view type
- HTML page views : 11643
- PDF downloads : 955