Suppurative Tonsillitis Caused by Suspected Community-Acquired Methicillin-Resistant Staphylococcus aureus Infection: A Case Report
Received: 24-Jan-2017 / Accepted Date: 06-Mar-2017 / Published Date: 13-Mar-2017 DOI: 10.4172/2161-1165.1000299
Abstract
Background: Suppurative tonsillitis is mainly caused by β-hemolytic streptococcal infection, staphylococcal infection, and Streptococcus pneumoniae infection. The presentations include general discomfort, shivering, fever, and muscle soreness of limbs. Physical examination shows pharyngeal congestion, tonsil reddening and swelling, and purulent exudate on the surface of tonsils. However, only a few case reports about suppurative tonsillitis caused by community-acquired MRSA infection have been published to date. This was a case report of suppurative tonsillitis caused by suspected MRSA infection, which could provide valuable evidence in guiding the treatment of such diseases.
Case presentation: A 36-year-old male from Heilongjiang Province (China) was admitted to the Respiratory Department in Zhejiang Hospital of Traditional Chinese Medicine for fever and pharyngalgia for 2 days. The patient had a history of tonsil infection, and received irregular penicillin treatment. The response of the patient to cephalosporins, penicillins, and carbapenems was generally suboptimal, and indicators of inflammation, including blood routine examination results, CRP, and PCT, were evidently elevated. Anti-MRSA therapy was continued for 1 week, which effectively alleviated the symptoms. As the risk of repeated tonsil infection could be relatively high, the patient received tonsillectomy in the Department of Otolaryngology.
Conclusions: For patients with suppurative tonsillitis who do not respond to conventional anti-inflammation therapy, the possibility of MRSA infection should be considered if the inflammation indicators increase continuously. Repeated throat swab smear examinations and blood culture can provide evidence to guide diagnosis. Aggressive systemic anti-infective treatments were performed for the present case, which effectively controlled systemic inflammatory reactions and prevented septicopyemia. Moreover, it laid foundations for further radical treatment.
Keywords: Suppurative tonsillitis; Community acquired methicillin resistant; Staphylococcus aureus ; Teicoplanin; Tonsillectomy
165436Case report
A 36-year-old male from Heilongjiang Province (China) was admitted to the Respiratory Department in Zhejiang Hospital of Traditional Chinese Medicine on April 14, 2016, for fever and pharyngalgia for 2 days. The patient was found with pharyngalgia and fever 2 days before, without evident causes; the highest body temperature was 39.8°C. Chill was found; however, no shivering, cough, expectoration, chest distress, polypnea, headache, vomiting, abdominal pain, or diarrhea was observed. The patient received fluid infusion in a local clinic (detailed treatment strategy was unclear), but the symptoms did not improve evidently.
Therefore, the patient was hospitalized in the hospital for further diagnosis and treatment, and the diagnosis on admission was “suppurative tonsillitis.” The patient had a history of tonsil infection, and received irregular penicillin treatment. Recurrence of symptoms was reported. No history of hepatitis, tuberculosis, poisoning, trauma, or surgery was reported. In addition, the patient reported no history of food or drug allergy, drug abuse, and prostitute visiting. However, the patient was a current smoker (about 100 cigarettes/year). Physical examinations on admission showed that the body temperature was 39.6°C, heart rate was 120 beats/min, blood pressure was 104/62 mmHg, and respiration was 20 times/min. The patient was in a state of clear consciousness with weak spiritual condition.
The skin and sclera were not yellow, and no pressing pain in the nasal sinus or cyanosis of lips was found. Pharyngeal hyperemia was noted, and grade II swelling of tonsils was found. Yellow-white pus was found on the pharyngeal wall, and trachea was in the center. Neck lymph nodes could be touched, with pressing pain. The breath sounds in bilateral lungs were clear, and no dry or wet role was found. The cardiac rhythm was regular, and no pathological murmurs in the auscultatory valve areas were observed.
The abdomen was soft and without pressing pain. Liver and spleen could not be touched under the rib. No percussion pain in renal areas or pressing pain in the ureter was found. The bilateral lower limbs were without edema, and neurologic examinations showed negative results. Chest computed tomography scanning was performed after hospitalization, and showed no abnormal changes. The results of electrocardiogram and echocardiography were basically normal. Ultrasound examination of upper abdomen showed cholecystolithiasis, while no other abnormality was found.
Ultrasound examination of the urinary system revealed prostatic hyperplasia and calcification. Ultrasound examination of thyroid and superficial neck lymph nodes showed no abnormal changes. Blood routine examinations showed that the white blood cell count was 20.2 × 109/l, percentage of neutrophils was 82.3%, percentage of lymphocytes was 9.9%, and no other abnormalities were found. Creactive protein (CRP) of the patient was 40 mg/l, and procalcitonin (PCT) was 0.11 ng/ml.
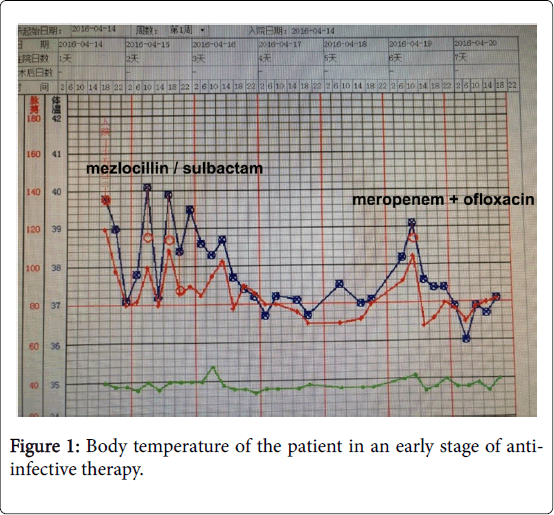
The results of urine routine examinations showed occult blood (±) and ketone bodies (±), while no other abnormalities were found. The results of prothrombin time, erythrocyte sedimentation rate, biochemical examinations, fecal routine examinations, fecal occult blood test, hematological neoplasm tests, and blood Mycoplasma pneumoniae antibody were all normal. After hospitalization, the patient received anti-infective therapy via mezlocillin/sulbactam infusion [3.75 IV glucose tolerance test (ivgtt), q8h] and symptomatic treatments (fluid infusion and anti-fever treatment). However, the body temperature ranged between 38 and 40°C, and pharyngeal swelling and pain were evident (Figures 1 and 2).
The body temperature of the patient decreased after temporary dexamethasone injection (5 mg, IV). Re-examination of blood routine on April 15 showed that the white blood cell count was 15.4 × 109/l, percentage of neutrophils was 72.1%, while no other abnormalities were found. The CRP of the patient was 36 mg/l. As the body temperature of the patient was repeatedly fluctuating, and indicators of inflammation were still very high, mixed bacterial infection was then considered.
Meropenem injection (1.0 IVGTT, q8h) in combination with oral loxacin (0.5 po. qd.) was used for anti-inflammation therapy. In addition, aerosol inhalation for anti-inflammation was also applied as symptomatic therapy. Blood culture was performed three times during the treatment, and the results showed no abnormality.
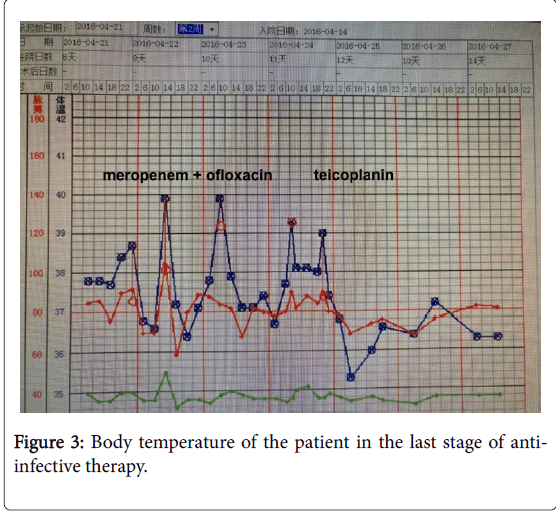
Throat swab smear examination showed no leukocyte phagocytosis, while G +ve cocci and G -ve bacilli were found. After the strategy of anti-infective therapy was changed, the body temperature of the patient still fluctuated. The highest body temperature was 40°C, and the antipyretic effects of temporary dexamethasone injection were very low. Re-examination of blood routine on April 25 showed that the white blood cell count was 15.0 × 109/L, percentage of neutrophils was 75.1%, while no other abnormalities were found. The CRP was 36 mg/L, and PCT was 0.09 ng/ml. Re-examination of throat swab smear showed a large number of G +ve cocci. Although repeated cultures showed no bacterial growth, suppurative tonsillitis caused by community-acquired methicillin-resistant Staphylococcus aureus (MRSA) infection was considered after the clinical presentations were taken into account. The patient and his family were informed of the disease conditions, and the strategy of anti-infective treatment was changed to teicoplanin (0.4 IVGTT, qd) after the consents from the patient was obtained. The body temperature of the patient decreased in the afternoon, and the pharyngeal swelling and pain relieved. Physical examinations showed that tonsil congestion was relieved, and the amount of pus decreased.
Anti-MRSA therapy was continued for 1 week, which effectively alleviated the symptoms. The body temperature of the patient returned to the normal level (Figure 3). Re-examination of blood routine on April 30 showed that the white blood cell count was 6.7 × 109/l, percentage of neutrophils was 49.3%, while no other abnormalities were found. The CRP was 3 mg/L, and PCT was 0.03 ng/ml. The general conditions of the patient were normal. No obvious pharyngeal swelling or pain was found, and pus on the pharyngeal wall disappeared (Figure 4), and the disease condition was stable. Therefore, the patient was discharged. As the risk of repeated tonsil infection could be relatively high in this patient, elective surgery was suggested. Therefore, the patient received tonsillectomy in the Department of Otolaryngology. The patient was followed up for eight months after the surgery, and no infection of Suppurative tonsillitis again. The life of the patient was basically normal.
Discussion
Suppurative tonsillitis is mainly caused by β-hemolytic streptococcal infection, staphylococcal infection, and Streptococcus pneumoniae infection. In addition, adenovirus infection could also induce suppurative tonsillitis. These pathogens can invade from outside or already exist in tonsillar crypts. The proliferation of these bacteria can increase when resistance to illness decreases in fatigue, constitutional weakness, excessive drinking and smoking, and irritation from noxious gases, and thus cause suppurative tonsillitis. The presentations include general discomfort, shivering, fever, and muscle soreness of limbs. Physical examination shows pharyngeal congestion, tonsil reddening and swelling, and purulent exudate on the surface of tonsils. In addition, lymphoid follicle enlargement, purulence, and multiple follicular abscesses can be found in patients with severe form of the disease.
The percentage of hospital-acquired S. aureus infection has increased evidently in recent years, most of which are MRS infections [1]. However, only a few case reports about suppurative tonsillitis caused by community-acquired MRSA infection have been published to date [2]. The response of the patient to cephalosporins, penicillins, and carbapenems was generally suboptimal, and indicators of inflammation, including blood routine examination results, CRP, and PCT, were evidently elevated. Although positive results of bacterial culture were obtained, multiple throat swab smear examinations and efficacies of clinical treatments suggested suppurative tonsillitis caused by suspected community-acquired MRSA infection. The disease improved after treatment with teicoplanin injection (0.4 ivgtt, qd), and the patient was discharged 1 week later. Currently, whether the treatment for community-acquired upper respiratory infection and soft tissue infection should also cover MRSA infection is still a point of discussion [3]. Horseman et al. have suggested that only betalactamases are needed for patients with community-acquired nonsuppurative cellulitis. Thus, MRSA coverage is not needed. However, for patients with suppurative cellulitis having underlying diseases (such as diabetes), anti-MRSA infective therapy is needed [4]. Xu et al. have investigated the etiologies and drug sensitivity in suppurative tonsillitis, and found that the most common pathogenic bacteria for suppurative tonsillitis in children included S. pyogenes , Haemophilus influenzae , S. aureus , and S. pneumoniae . These pathogens have elevated drug resistance to first-generation cephalosporins and penicillin, and sensitive antibiotics should be selected according to the results of drug sensitivity test and features of drug resistance in the corresponding region [5].
Teicoplanin is a new nonintestinal glycopeptide antibiotic with high bactericidal activity. Teicoplanin can bind to aminoacyl-D-alanyl-Dalanine in the peptidoglycan subunit, thus destructing the bacterial cell wall and inducing bacterial death. The antibacterial activity of teicoplanin is very high for Gram-positive aerobic bacteria and anaerobic bacteria, especially for MRSA infection. Teicoplanin is one of the few drugs that have antibacterial activities against multi-drug resistant S. aureus and Enterococcus [6]. Compared with vancomycin, the universally acknowledged antibiotic against resistant bacteria, teicoplanin has similar antibacterial activity, same action mechanism, and comparable or even better clinical efficacy; it could be applied via intravenous or muscular injection. In addition, the in vivo antibacterial activity of teicoplanin is very high. The half-life is relatively long, and it has relatively long-lasting postantibiotic effects. The loading dose of teicoplanin is generally 400 mg/dl, and the consequent maintenance dose is 200 mg for treatment. In the present case of suppurative tonsillitis caused by MRSA infection, body temperature and inflammation indicators remained at high levels. Therefore, a loading dose of teicoplanin was continuously used. Re-examination of inflammation indicators 1 week later showed that the body temperature returned to the normal level. The patient recovered and was discharged from the hospital. This was the first case report of suppurative tonsillitis caused by MRSA infection, which could provide valuable evidence in guiding the treatment of such diseases.
Current opinions mainly suggest that the long-term irregular application of antibiotics is one of the high risks of MRSA infection [7]. The patient in the present case report had a history of long-term irregular use of penicillin in a local hospital, and the treatment durations were not standard, which could be the major factor inducing MRSA infection. For patients with suppurative tonsillitis who do not respond to conventional anti-inflammation therapy, the possibility of MRSA infection should be considered if the inflammation indicators increase continuously. Repeated throat swab smear examinations and blood culture can provide evidence to guide diagnosis, while effective MRSA coverage is one of the most effective treatments that should be prescribed by physicians. However, radical treatment method is still tonsillectomy. Aggressive systemic anti-infective treatments were performed for the present case, which effectively controlled systemic inflammatory reactions and prevented septicopyemia. Moreover, it laid foundations for further radical treatment. Currently, the physician– patient relationship is very tense in China. Hence, curing patients as possible and reducing medical disputes are the aims of every health care worker.
Declarations
Consent to publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
Competing interests
The authors declare that they have no competing interests.
Authors contributions
Ruihai Ye interviewed the patient in the hospital setting, performed the literature review,draft writing and editing. Zhen Wang contributed to the idea conception and execution. Junchao Yang supervised the patient treatment in hospital and Zhonghai Wang reviewed the case presentation and discussion.Shaohua Lin provided the diagnosis for laboratory. Both authors read and approved the final manuscript.
References
- Ji F, Li Y, Hu Z (2015) Clinical distribution and drug-resistance surveillance of methicillin-resistant Staphylococcus aureus in Chengdu from 2013 to 2014. Xi Bu Yi Xue 27:607-613.
- Wang JT, Wu HS, Weng CM (2013) Prognosis of patients with methicillin-resistant Staphylococcus aureus bloodstream infection treated with teicoplanin: a retrospective cohort study investigating effect of teicoplanin minimum inhibitory concentrations. BMC Infect Dis 13:182-189.
- Brook I, Foote PA (2006) Isolation of methicillin resistant Staphylococcus aureus from the surface and core of tonsils in children. Int J Pediatr Otorhinolaryngol 70:2099-2102.
- Horseman M, Bowman JD (2013) Is community-acquired methicillin-resistant staphylococcus aureus coverage needed for cellulitis? Infect Dis Ther 2:175-185.
- Xu HX, Zhong Q (2014) Comparative study of etiologies and drug-sensitivity of suppurative tonsillitis in children. You Jiang Min Zu Yi Xue Yuan Xue Bao 53:418-420.
- Sachithanandam ST (2014) Rising methicillin-resistant staphylococcus aureus Infections in ear, nose, and throat diseases. Case Rep Otolaryngol 2014:253945.
- van der Vorm ER, Groenendijk EH (2003) Two hospital staff with throat carriage of methicillin-resistant Staphylococcus aureus, which had to be treated with systemic antibiotics. Ned Tijdschr Geneeskd 147:1079-1081.
Citation: Ye R, Yang J, Wang Z, Lin S, Wang Z (2017) Suppurative Tonsillitis Caused by Suspected Community-Acquired Methicillin-Resistant Staphylococcus aureus Infection: A Case Report. Epidemiology (Sunnyvale) 7:299. DOI: 10.4172/2161-1165.1000299
Copyright: © 2017 Ye R. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 9417
- [From(publication date): 0-2017 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 8542
- PDF downloads: 875