Review Article Open Access
Supportive Care and Geriatric Assessment in Older Cancer Patients
Colloca G*, Galindo Navas LM, Ortolani E, Sisto A, Ferrandina C and Landi FDepartment of Geriatrics, Neurosciences and Orthopedics, Catholic University of the Sacred Heart, L.go Francesco Vito 1, Rome 00168, Italy
- *Corresponding Author:
- Giuseppe Colloca MD, PhD
Department of Geriatrics, Neurosciences and Orthopedics
Catholic University of the Sacred Heart
L.go Francesco Vito 1, Rome 00168, Italy
Tel: +39 3388401979
Fax: +39 06 3051911
E-mail: giuseppe.colloca@rm.unicatt.it
Received date: September 25, 2015, Accepted date: October 09, 2015 Published date: October 12, 2015
Citation:Colloca G, Navas LMG, Ortolani E, Sisto A, Ferrandina C, et al. (2015) Supportive Care and Geriatric Assessment in Older Cancer Patients. J Palliat Care Med 5:235. doi:10.4172/2165-7386.1000235
Copyright: © 2015 Colloca G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
In the management of elderly people with cancer under diagnosis, under treatment, or overtreatment, are often recurring problems that can be minimized through the application of Geriatric Assessment. Research studies show that older patients experience more incomplete investigations, toxicity complications, dose reductions and delays and decreased utilization of standard therapy compared to younger patients. The increased incidence of comorbidities in older adults can raise the risk of treatment related toxicities; however the assumption of sarcopenia and/or frailty based on a patient’s age alone may lead to inadequate and inappropriate treatment. The use of Geriatric Assessment, the best practices physicians currently have, can direct supportive care interventions. The Geriatric Assessment assists physicians in determining a patient’s medical decision making capacity, emphasizes the preservation of independent function and minimizes the risk of toxicity, regardless of treatment or treatment intent. The goal of this review is to explain the most relevant aspects of the comprehensive geriatric assessment in elderly cancer patients and provide the basis for supportive care therapies such as pain management, dyspnoea, cachexia and geriatric syndromes like sarcopenia.
Keywords
Geriatric assessment; Cancer; Supportive care; Elderly
Introduction
The most important risk factor in the development of cancer is age. Approximately 50% of newly diagnosed cases occur in people over 65 years and that percentage is expected to increase to 70% by 2030 [1]. The incidence of cancer is between 12 and 36 times higher in adults aged over 65 compared to younger people. This is compounded by the fact that the cancer-related mortality in older populations is higher, close to 70% per year [2]. While these statistics clearly indicate the immediate need for geriatric considerations in caring for most cancer patients, the situation will be magnified by demographic trends that predict an expansion of the elderly population in developed and also developing countries. In the United States alone the 85+ population is projected to triple by 2040 [3].
Based on the anticipated increase in the number of older individuals with cancer the application of the geriatric approach represents a major challenge for health systems. The Geriatric Assessment (GA) considers malnutrition, functionality, polypharmacy, cognitive impairment, depression, social support networks along with a wide variety of comorbidities and geriatric syndromes in evaluating the best choice (treatment, no treatment, palliative care) for the patient. This assessment provides physicians the information necessary to properly estimate the probability of adverse outcomes and allows them to determine the relevance, the intensity and the choice of treatment, consequently improving patient outcomes [4].
Cancer management in the elderly is typically considered suboptimal, mainly due to delays in diagnosis and a tendency to undertreat fit patients or to over treat patients in that may be helpful a palliative care. This because with older patients, physicians often over generalize based on age rather than ascertaining the patient’s true health status in the treatment decision. The National Cancer Center Network (NCCN) addresses the needs of the aging population through an evaluation of mortality risk, treatment toxicity and other issues that may influence the personalized care of the elderly in a framework of guidelines for the management of cancer treatment [5]. Early supportive care is clearly desirable for all patients at low or high risk of treatment complications. There are ongoing efforts by the International Society of Geriatric Oncology (SIOG) to develop validated scales that can help clinicians identify these patients, in order to decide the best therapy by recognizing which patients will benefit from aggressive treatments and which patients are more appropriately treated with supportive therapy at the beginning or at the final stages of the disease [6,7]. In addition to symptom management, the preservation of functional independence and the improvement of quality of life is a major goal in the treatment of elderly.
Supportive care
Geriatricians consider Supportive Care (SC) in older people to be a discipline of palliative care that provides a more comprehensive approach to patient care aimed at improving the quality of life (QOL), reducing unnecessary hospitalization and increasing patient satisfaction [7,8]. SC guides interventions, providing strategies to prevent and manage treatment toxicity. For example, the routine use of growth factors in older adults undergoing myelosuppressive chemotherapy and the facilitation of the identification and management of multimorbidities and geriatric syndromes is one such supportive care strategy. In elderly cancer patients there are symptoms and conditions that have a strong impact on quality of life that physicians can eliminate or ameliorate. The Geriatric Assessment may reduce or avoids cancer-related domains such as pain, fatigue, nutrition, dyspnea, anemia and bone complications and treatmentrelated domains (adverse drug reaction) such as hematological toxicity, infections, mucositis, neuropathy, heart toxicity and skin diseases [9,10]. In regards to chemotherapy toxicity, its high susceptibility often is due to age-related physiologic changes, polypharmacy and the higher prevalence of comorbidities in older patients [11].
Moreover a key point for the compliance of patients are the psychosocial conditions, the importance of QOL, spiritual attitude and depression in increasing/decreasing patients’ motivation for treatment [9,10,12].
Geriatric Assessment
The elderly cancer patient management is based on the same principles of younger patient populations, but the elderly are at an increased risk of adverse drug reaction due to age-related decreases in organ function, polypharmacy with its increased risk of drug–drug interactions and multimorbidity.
The Geriatric Assessment (GA) is a methodology that includes assessment tools able to predict the functional age of elderly patients with cancer and separates out components that have been associated with different types of cancer treatment and survival. It simultaneously highlights the deficits and problems that may impact morbidity and mortality [13]. A multitude of different tools are available to assess each of these domains and the decision of which to utilize is still not highly standardized, often based on geography, availability, and local regulation [12,14]. The impact of GA on altering treatment choice has varied significantly among recent studies evaluating the efficacy of GA though there is general consensus that the GA serves as a valuable predictor of complications and side effects, functional decline, and overall survival/mortality over the course of treatment [13]. GA is also useful in detecting problems in clinical histories, reducing hospital readmissions, aiding in conventional monitoring and improving selfrated health [15,16]. In a study of elderly with stage I-III primary breast cancer, the general and breast cancer specific death rate after 5 and 10 years was approximately two times higher in women with 3 or more cancer-specific GA deficits, regardless of age and stage of disease [17]. In ELCAPA study using a multivariate analysis, researchers found a lower ADL score and malnutrition were independently associated with cancer treatment changes [18,19]. The results of a GA should be considered along with an understanding of the specific cancer, its stage, pathophysiology, prognosis and the expected effects of available therapeutics in order to ensure a realistic discussion of the probable risks, benefits and rationale for therapeutic strategies with patients, their families and other caregivers [13,18,20].
Important GA domains involved in decision-making are functional status, cognitive impairment, mood, social support/environment, comorbidity and geriatric syndromes, food intake, muscle mass and medications (Table 1).
| Assessment domain | Commonly used instruments | Relevance |
|---|---|---|
| Functional status Activities of Daily Living (ADL) Instrumental Activities of Daily Living (IADL) Mobility |
-KatzIndex -Lawton Brody -Gait Speed -Timed Up and Go (TUG) test |
Decreased treatment tolerance Decreased rates of survival Increased risk of falls |
| Cognitive function Dementia Depression Delirium |
-Mini Mental State Examination -Geriatric Depression Scale -Confusion Assessment Method |
Reduced overall survival Increased risk of toxicity of treatment Increased risk of functional decline Impact treatment adherence and quality of life. Higher utilization of health resources |
| Nutritional status | -Mini Nutritional Assessment | Increased toxicity to chemotherapy and risk of complications of treatment |
| Polypharmacy | -Beers Criteria -STOPP/START Criteria |
Increased risk of drug-drug interactions and other adverse drug events, risk of hospitalizations and toxicity of treatment |
| Comorbidities | -Charlson Comorbidity Index -Cumulative Illness Rating Scale—Geriatrics (CIRS-G) |
Early treatment interruptions Impact in survival and adverse drug reactions |
| Social support | -The Medical Outcomes Study -Social Support Survey |
Impact on ability to afford treatment, compliance Caregiver burden |
Table 1: Geriatric assessment domains.
Functional status
Poor functional status has been identified as a significant impediment to cancer therapy because it is associated with decreased treatment tolerance and decreased rates of survival in older patients with cancer [21]. The item of functional status is subdivided into an assessment of the ability to perform activities of daily living (ADL), an assessment of the instrumental activities of daily living (IADL), an assessment of mobility using the Gait Speed or Timed Up and Go (TUG) test, an assessment of the risk of falls, an assessment of visual and auditory sufficiency [18].
Cognitive function
Patients with cancer in conjunction with cognitive impairment are at risk for noncompliance and nonadherence to therapeutic regimens as well as for delirium and early death [22]. The Mini Mental State (MMS) is a widespread screening instrument used to evaluate cognitive difficulties in orientation, registration, attention, calculation, recall and language. Regarding affective symptoms, estimates of the prevalence of depression among the elderly with cancer vary widely from 3% and 25%. The presence of this complication is associated with an increased risk of functional decline and a higher utilization of health resources [23]. The Geriatric Depression Scale (GDS) is a multiquestion, elderly validated, self-rating instrument that is capable of distinguishing the mild and severely depressed from normal individuals [24].
Multimorbidity and geriatric syndromes
It is more likely for elderly cancer patients to have an inappropriate drug prescription or to be more susceptible to early treatment interruptions compare younger if there are more than 2 comorbidities [25]. Comorbidity represents a combination of additional diseases beyond an index disorder. Currently, in geriatrics, multimorbidity is the most used term, able to identify any co-occurrence of two or more chronic or acute diseases and medical conditions within one patient, indicating a shift of interest from a given index condition to individuals who suffer from multiple disorders.
The list of geriatric syndromes includes incontinence, delirium, falls, pressure ulcers, sleep disorders, problems with eating or feeding, pain, and depressed mood. Dementia and physical disability are also sometimes considered to be geriatric syndromes. Thus the term syndrome that is normally used to describe a pattern of symptoms and signs that have a single underlying cause is not able to cover the Geriatric Syndromes, indeed this terminology in Geriatric reflects the complex interactions between an individual's vulnerabilities and exposure to stressors, the multifactorial pathophysiology that occur when the accumulated effects of impairments in multiple systems, (often involving systems unrelated to the apparent chief complaint) that render an older person vulnerable to situational challenges. These syndromes are important to identify because of their deleterious effects on function and quality of life, in older cancer patients and because they often may be remediable with therapeutic intervention, in this scenario is really important to differentiate between condition very similar as anorexia, sarcopenia and cachexia [26].
Polypharmacy
Polypharmacy is defined as the concurrent use of five or more drugs. Not age but the number of drugs used, increased the risk of experiencing an Adverse Drug Reaction [27]. Tools and tests describing the level of polypharmacy in different patients are the Beers Criteria (Beers Criteria for Potentially Inappropriate Medication Use in Older Adults or Beers List) [28], STOPP [Screening Tool of Older Person’s Prescriptions] and START [Screening Tool to Alert Doctors to Right Treatment] criteria [29].
Nutritional status
The weight reduction and/or low body mass index have a negative impact on overall health, increasing mortality and toxicity to chemotherapy [30]. The Mini Nutritional Assessment (MNA) is a validated approach to gauge nutritional deficiency and/or malnutrition, both of which are a common problem occurring in 15– 60% of elderly patients as a result of disease, poor eating habits or inadequate social support systems [31].
Social support and environment
Social isolation and the perception of loneliness increases the risk for mortality, especially in the elderly [32]. The Medical Outcomes Study (MOS) Social Support Survey provides a multidimensional tool to evaluate emotional/informational, tangible, effective and positive social interactions [33].
Anorexia, cachexia and sarcopenia
Aging is characterized by the loss of homeostatic mechanisms together with the occurrence of multiple changes in body composition and loss of organ function (frailty syndrome). One of the most remarkable changes exposed by the aging process is skeletal muscle degeneration or sarcopenia.
Sarcopenia can be considered the biological substrate for the development of physical frailty [34]. Both conditions deal with several features that constitute major causes of physical function impairment, disability and mortality in the elderly [34]
When a geriatric patient develops cancer the systemic effect induced by cancer alone and geriatric profile may compromise the prognosis. Several adaptations associated with cancer burden share mechanisms that are involved in the aging process itself like the activation of the inflammatory response or increased muscle protein breakdown [35]. Cancer cachexia, anorexia and sarcopenia crosstalk through different metabolic and immunologic pathways resulting in muscle degeneration and atrophy [36].
The main clinical feature in adults is weight loss (Table 2). Sarcopenia, is defined by the presence of both low muscle mass and low muscle function (strength and performance) [37]. Lean body mass is always lost while fat mass may be reduced, preserved or even increase leading to an ambiguous change in final body weight [38].
| Anorexia | Sarcopenia | Cachexia |
|---|---|---|
| “loss of appetite and/or lower food intake” |
“ presence of both low muscle mass and low muscle function (strength or performance)” | “complex metabolic syndrome associated with underlying illness and characterized by loss of muscle with or without loss of fat mass” |
| �lean body mass �fat mass �body weight |
�lean body mass �/ = /fat mass �/ = /body weight |
�lean body mass �/ = fat mass �body weight |
Table 2: Clinical feature in adults weight loss.
Cachexia is widely observed in older adults with cancer. It affects around 50-80% of cancer patients and may account for up to 20% of cancer deaths. The cachectic syndrome is defined as a complex metabolic syndrome associated with underlying illness and is characterized by loss of muscle along with an ambiguous change in fat mass [39]. Cancer cachexia is an energy-wasting syndrome invariably associated with muscle wasting. Loss of myofibrillar protein in muscle cells results in muscle weakness and fatigue [40]. Bidirectional sarcoplasmic reticulum (SR)-mitochondrial communication is compromised leading to skeletal muscle dysfunction [41]. During cachexia an increase in the activity of SR Ca pumps (SERCA) occurs promoting energy inefficiency; overexpression of PGC1alfa causes expression of genes linked to mitochondrial uncoupling and energy expenditure [42]. Other molecular mechanisms that contribute to energy imbalance include insulin resistance, increased futile cycle activity, TNF alfa and IL1 and other pro-inflammatory, pro-cachectic cytokines [43]. Persons with cachexia due to cancer may deplete up to 80% of their muscle mass and skeletal muscle loss is a very powerful prognostic factor independent of the actual body weight loss [44].
Evans elaborated CASCO score to diagnose and stage cachexia [45]. Body weight loss and composition accounts for up 40% of CASCO. It represents risk of impaired physical performance and loss of quality of life. The second relevant component of the score is inflammation/ metabolic disturbances/immunosuppression; several studies suggest the role of that response in pathological conditions other than cancer [46]. Anorexia is the fourth element of CASCO. Anorexia is defined as the presence of loss of appetite and/or lower food intake. Anorexia, coupled with a decrease in exercise leads to a decline in muscle mass and strength [47]. It could also be hypothesized that selective malnutrition anorexia is directly correlated with the onset of sarcopenia [48]. This contributes to an increasing rate of institutionalization and poorer quality of life [47]. Sarcopenia can be considered the link between several multifactorial syndromes affecting oncologic patients like anorexia malnutrition and cachexia.
Pain
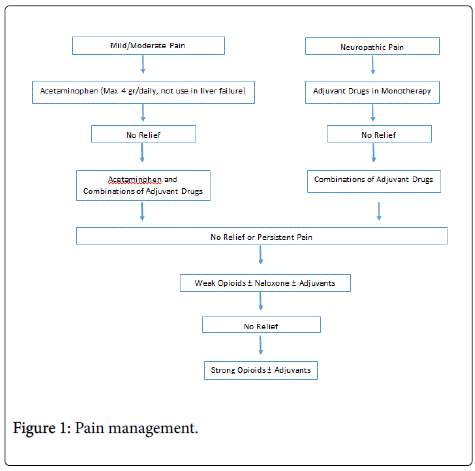
The approach to pain management in older persons differs from that for younger people (Figure 1); clinical manifestations of persistent pain are often complex and multifaceted in the frail population. In addition, older people may underreport pain. For instance, there are inherent difficulties in recognizing pain experienced when a cognitive impairment co-exists [49]. Persistent pain is among the most important symptoms in terms of prevalence and potential consequences in cancer care, depending on the type and extent of the disease. The overall prevalence of persistent pain ranges between 15% and 80% in populations with no hematological disease, but an average of 45% of cancer patients receive inappropriate or no care for pain [49,50]. Cancer subsumes many diseases and rapidly changes the therapeutic landscape. The analgesic plan of care is often ineffective in the presence of pain caused through direct tissue injury or a related process such as inflammation. Therefore, persistent cancer pain represents syndromes that are directly related to cancer itself (neuropathic, visceral, somatic and paraneoplastic syndromes) or to the treatment of cancer (chemotherapy, radiation, and surgery) [49]. Syndrome recognition can guide additional clinical assessment and treatment, clarify prognosis, allow for proper care and offer reassurance to patients that often interpret pain as an indication of cancer progression [9,49] The potential effects of cancer treatment should be considered in the development of a strategy for cancer pain in the elderly, for example, if pain is focal and related to cancer mass effect, radiotherapy can be effective, or if the cancer has spread, chemotherapy may be helpful [49,51].
A pain history, a physical examination and pain scales are useful tools in the systematic assessment of symptoms, but they need to be tailored according to the needs of specific populations (i.e. patients with cognitive impairment, or with more than one type of pain) and should never be used as substitutes for a complete and deep pain assessment [9,49]. The World Health Organization advocates a threestep ladder of pain management and illustrates that the process of selecting analgesic drugs should be dependent on an assessment of the intensity of pain experienced by the patient, rather than the etiology of pain [9,49,52]. In the elderly as in younger patients the right dose of an analgesic is the dose that relieves pain without causing unmanageable side effects and the least-invasive method of drug administration should be used for this purpose [49].
Older patients are generally at higher risk of adverse drug reactions and age-adjusted dosing is not available for most analgesics. Pain killer drugs can be safe and effective when comorbidities, age-associated differences, and pharmacokinetic and pharmacodynamic drug properties are carefully considered [11,49]. Dosing for the elderly needs to start low, followed by careful upward titration [9]. In older patients, the intramuscular route should be avoided because of issues with painful injections, cachexia/sarcopenia and reduced muscle mass. The subcutaneous route is appropriate for those elderly who are unwilling or unable to take oral medications [49]. Transdermal, rectal, and trans mucosal routes may be essential for people with swallowing difficulties [49]. Doses and timing of drug administration is essential due to the rapid-onset of persistent pain; analgesics should be taken at regular time intervals and not “as needed”, adjuvant drugs should be prescribed when required; and each patient should be regularly reassessed in order to determine the response to treatment and to ensure that he/she experiences maximum benefit [49,53]. In some patients in which no single agent can produce pain relief without doselimiting adverse effects, more than a single drug may be required to obtain a specific therapeutic endpoint [49]. Moreover, a combination of two or more drugs with complementary mechanisms of action may work synergistically to afford greater relief with less toxicity than higher doses of a single agent (rational polypharmacy) [49,54]. Patients who experience poor analgesia or significant side effects may benefit from an opioid switching that involves discontinuation of the previously used opioid and initiation of the new one at the equianalgesic dose [49]. In elderly regarding an appropriate choice, a number of factors influence it, such as preference, compliance or adherence, organ function, co-morbidities, outpatient vs. inpatient, drug metabolism, and routes of administration, analgesic effects and availability [49,55]. Moreover non pharmacologic measures can also be used and have to be considered in the elderly, such as massage, topical agents, and physical modalities, cognitive strategies meditation, prayer, social gatherings, and humor, can also be effective in some cases [9,56].
Geriatric screening tools
The Geriatric Assessment guides the management of elderly cancer patients in a way that distinguishes fit patients, who can receive standard cancer treatment, from those in whom comorbidities, geriatric syndromes and disabilities are a contraindication of full treatment but not of interventions in supportive care that will improve their quality of life [7,57]. However, Geriatric Assessments are not always used because of the significant time constraints needed to administer them, and so attempts have been made to develop screening tools, or abbreviated instruments, to identify patients that need a full GA [58]. The domains most often assessed by screening tools are self-rated health, cognitive function, nutritional status, comorbidity and functional status [18].
G8: The G8 is an eight-item screening tool, developed for older cancer patients. The tool covers multiple domains usually assessed by the geriatrician when performing the GA and takes about 5 minutes. A score of ≤14 is considered abnormal [59].
Vulnerable elders survey 13: Is a 13-item self-administered tool, developed for identifying older people at increased risk of health deterioration within the community. A score of ≥3 identifies individuals as vulnerable, defined as an increased risk of functional decline or death over the next 2 years [60]. The time necessary to complete the VES-13 is 5 minutes. In older persons in the community, an abnormal VES-13 was associated with a reduction function, survival and health outcomes [59].
Triage risk screening tool (TRST): The tool is composed of five yes/no questions and those obtaining a score of ≥2 are considered as at risk. This tool takes two minutes to complete [61]. The Flemish version of the Triage Risk Screening Tool fTRST(1) and fTRST(2) were predictive of functional decline with fTRST(1) demonstrating the highest sensitivity [14].
Groningen frailty indicator: The Groningen Frailty Indicator (GFI) is composed of 15 questions addressing various domains and was developed for people aged 65 years and over, including hospital inpatients, nursing home residents and community dwelling elderly. A score of ≥4 indicates a risk of physical, social and/or psychological impairment [58].
Barber questionnaire: The Barber Questionnaire was developed to identify older persons at risk for dependence in the community [62]. It consists of nine yes/no questions and patients with a score of ≥1 are considered candidates for further evaluation through GA.
Abbreviated comprehensive geriatric assessment: The abbreviated comprehensive geriatric assessment (aCGA) [58,63] consists of the 15 items from the full CGA that most correlated with the findings of the CGA. The time to complete aCGA was 5 min, with an observed overall sensitivity of 51% and specificity of 97% [64].
The performance of different screening tools may depend on the setting and the preferred screening tool may depend on the clinical situation. [18,58,59]. None of the screening tools were successful in identifying impairments across all the domains included in GA. Given this lack of data supporting the efficacy of any one screening tool in predicting the outcome of a GA, it would be advised to assess all older patients with a GA to have a personalized choice [18,58]. However, in a “real world” clinical practice, this approach is often not possible because time consuming, thus the use of a screening tools is recommended to identify patients in need of further evaluation by GA if there is not available a geriatric center to send the patient or a geriatrician in multidisciplinary assessment team.
Conclusion
Supportive Care in elderly is considered a discipline of palliative care that provides a more comprehensive approach to the complex patient, it is aimed at improving the quality of life (QOL), reducing unnecessary hospitalization and increasing patient satisfaction. Thus in a field as geriatric oncology were the cancer management in the elderly is usually considered suboptimal, for the delays in diagnosis and a tendency to undertreat fit patients or to over treat frail and vulnerable patients, supportive care should be taken into greater consideration. With elderly, physicians often generalize based on age rather than patient’s true health status in the treatment choice. Our suggestion, for those who approach or begin to assess elderly patients, is to consider several factors that can to truly favor the best choice to the patient, in accordance his/her wishes and that allow to maintain it self-sufficient and good quality of life. The geriatric assessment is an easy way to allows, really, a tailor made management focuses on needs of patients.
References
- Yancik R (2005) Population aging and cancer: a cross-national concern. Cancer J 11: 437-441.
- de la Cruz M, Bruera E (2013) Approach to the older patient with cancer.BMC Med 11: 218.
- Siegel R, Naishadham D, Jemal A (2013) Cancer statistics, 2013.CA Cancer J Clin 63: 11-30.
- Yee KWL, Pater JL, Pho L, Zee B, Siu LL (2003) Enrollment of older patients in cancer treatment trials in Canada: why is age a barrier? J ClinOncol 21: 1618-1623.
- Hoffe S, Balducci L (2012) Cancer and age: general considerations.ClinGeriatr Med 28: 1-18.
- Kapo J, Morrison LJ, Liao S (2007) Palliative care for the older adult.J Palliat Med 10: 185-209.
- Brighi N, Balducci L, Biasco G (2014) Cancer in the elderly: is it time for palliative care in geriatric oncology?J GeriatrOncol 5: 197-203.
- Lee RT, Ramchandran K, Sanft T, Von Roenn J (2015) Implementation of supportive care and best supportive care interventions in clinical trials enrolling patients with cancerâ€. Ann Oncol 26: 1838-1845.
- Balducci L (2003) New paradigms for treating elderly patients with cancer: the comprehensive geriatric assessment and guidelines for supportive care. J Support Oncol 1: 30-37.
- Wagland R, Richardson A, Armes J, Hankins M, Lennan E, et al. (2014) Treatment-related problems experienced by cancer patients undergoing chemotherapy: a scoping review. Eur J Cancer Care 24: 605-617.
- Colloca G, Santoro M, Gambassi G (2010) Age-related physiologic changes and perioperative management of elderly patients. SurgOncol 19: 124-130.
- Davis MP (2011) The MASCC Textbook of Cancer Supportive Care and Survivorship Support. Care Cancer 11-22.
- Wildiers H, Heeren P, Puts M, Topinkova E, Janssen-Heijnen MLG, et al. (2014) International Society of Geriatric Oncology Consensus on Geriatric Assessment in Older Patients With Cancer. J ClinOncol 54: 8347.
- Kenis C, Decoster L, Van Puyvelde K, De Grève J, Conings G, et al. (2014) Performance of two geriatric screening tools in older patients with cancer.J ClinOncol 32: 19-26.
- Extermann M, Boler I, Reich RR, Lyman GH, Brown RH, et al. (2012) Predicting the risk of chemotherapy toxicity in older patients: the Chemotherapy Risk Assessment Scale for High-Age Patients (CRASH) score Cancer 118: 3377-3386.
- Hamaker ME, Prins MC, Stauder R (2014) The relevance of a geriatric assessment for elderly patients with a haematological malignancy--a systematic review.Leuk Res 38: 275-283.
- Clough-Gorr KM, Thwin SS, Stuck AE, Silliman RA (2012) Examining five- and ten-year survival in older women with breast cancer using cancer-specific geriatric assessment.Eur J Cancer 48: 805-812.
- Hurria A, Wildes T, Blair SL, Browner IS, Cohen HJ, et al. (2014) Senior adult oncology, version 2.2014: clinical practice guidelines in oncology. J NatlComprCancNetw 12: 82-126.
- Caillet P, Canoui-Poitrine F, Vouriot J, Berle M, Reinald N, et al. (2011) Comprehensive geriatric assessment in the decision-making process in elderly patients with cancer: ELCAPA study. J ClinOncol 29: 3636-3642.
- Owusu C, Berger NA (2014) Comprehensive geriatric assessment in the older cancer patient: coming of age in clinical cancer care ClinPract (Lond) 11: 749-762.
- Maione P, Perrone F, Gallo C, Manzione L, Piantedosi F, et al. (2005) Pretreatment quality of life and functional status assessment significantly predict survival of elderly patients with advanced non-small-cell lung cancer receiving chemotherapy: a prognostic analysis of the multicenter Italian lung cancer in the elderly. J ClinOncol 23: 6865-6872.
- Stilley CS, Bender CM, Dunbar-Jacob J, Sereika S, Ryan CM (2010) The impact of cognitive function on medication management: three studies. Health Psychol 29: 50-55
- Kua J (2005) The prevalence of psychological and psychiatric sequelae of cancer in the elderly - how much do we know?Ann Acad Med Singapore 34: 250-256.
- Yesavage JA, Sheikh JI (1986) 9/Geriatric Depression Scale (GDS). ClinGerontol 5: 165-173.
- Frasci G, Lorusso V, Panza N, Comella P, Nicolella G, et al. (2000) Gemcitabine plus vinorelbine versus vinorelbine alone in elderly patients with advanced non-small-cell lung cancer.J ClinOncol 18: 2529-2536.
- Winters-Stone KM, Lyons KS, Nail LM, Beer TM (2012) The Exercising Together project: design and recruitment for a randomized, controlled trial to determine the benefits of partnered strength training for couples coping with prostate cancer. Contemp. Clin Trials 33: 342-350.
- Carbonin P, Pahor M, Bernabei R, Sgadari A (1991) Is age an independent risk factor of adverse drug reactions in hospitalized medical patients?J Am GeriatrSoc 39: 1093-1099.
- American Geriatrics Society 2012 Beers Criteria Update Expert Panel (2012) American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults.J Am GeriatrSoc 60: 616-631.
- Gallagher P, Ryan C, Byrne S, Kennedy J, Mahony DO (2008) STOPP (Screening Tool of Older Person’s Prescriptions) and START (Screening Tool to Alert doctors to Right Treatment). Consensus validation. Int J ClinPharmacol. Ther 46: 72-83.
- Newman AB, Yanez D, Harris T, Duxbury A, Enright PL, et al. (2001) Weight change in old age and its association with mortality.J Am GeriatrSoc 49: 1309-1318.
- Vellas B, Guigoz Y, Garry PJ, Nourhashemi F, Bennahum D, et al. (1999) The Mini Nutritional Assessment (MNA) and its use in grading the nutritional state of elderly patients.Nutrition 15: 116-122.
- Shankar A, McMunn A, Banks J, Steptoe A (2011) Loneliness, social isolation, and behavioral and biological health indicators in older adults. Health Psychol 30: 377-385.
- Sherbourne CD, Stewart AL (1991) The MOS social support survey.SocSci Med 32: 705-714.
- Landi F, Calvani R, Cesari M, Tosato M, Martone AM, et al. (2015) Sarcopenia as the Biological Substrate of Physical Frailty. ClinGeriatr Med 31: 367-374.
- Scheede-Bergdahl C, Watt HL, Trutschnigg B, Kilgour RD, Haggarty A, et al. (2012) Is IL-6 the best pro-inflammatory biomarker of clinical outcomes of cancer cachexia?ClinNutr 31: 85-88.
- Argilés JM, Busquets S, Stemmler B, López-Soriano FJ (2014) Cancer cachexia: understanding the molecular basis.Nat Rev Cancer 14: 754-762.
- Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, et al. (2010) Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 39: 412-423.
- Prado CMM, Lieffers JR, McCargar LJ, Reiman T, Sawyer MB, et al. (2008) Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study.Lancet Oncol. 9: 629-635.
- Blum D, Omlin A, Fearon K, Baracos V, Radbruch L, et al. (2010) Evolving classification systems for cancer cachexia: ready for clinical practice?Support Care Cancer 18: 273-279.
- Martin L, Birdsell L, Macdonald N, Reiman T, Clandinin MT, et al. (2013) Cancer cachexia in the age of obesity: skeletal muscle depletion is a powerful prognostic factor, independent of body mass index. J ClinOncol 31: 1539-1547.
- Fontes-Oliveira CC, Busquets S, Toledo M, Penna F, Paz Aylwin M, et al. (2013) Mitochondrial and sarcoplasmic reticulum abnormalities in cancer cachexia: altered energetic efficiency? BiochimBiophysActa 1830: 2770-2778.
- Miura S, Tomitsuka E, Kamei Y, Yamazaki T, Kai Y, et al. (2006) Overexpression of peroxisome proliferator-activated receptor gamma co-activator-1alpha leads to muscle atrophy with depletion of ATP. Am J Pathol 169: 1129-1139.
- Glass DJ (2010) Signaling pathways perturbing muscle mass.CurrOpinClinNutrMetab Care 13: 225-229.
- Baracos VE (2001) Management of muscle wasting in cancer-associated cachexia: understanding gained from experimental studies. Cancer 92: 1669-1677.
- Evans WJ, Morley JE, Argilés J, Bales C, Baracos V, et al. (2008) Cachexia: a new definition. ClinNutr 27: 793-799.
- Delano MJ, Moldawer LL (2006) The origins of cachexia in acute and chronic inflammatory diseases.NutrClinPract 21: 68-81.
- Kalantar-Zadeh K, Kuwae N, Wu DY, Shantouf RS, Fouque D, et al.(2006) Associations of body fat and its changes over time with quality of life and prospective mortality in hemodialysis patients. Am J ClinNutr 83: 202-210.
- Nakanishi K (2001) Innate and acquired activation pathways in T cells.Nat Immunol 2: 140-142.
- Colloca G, Lattanzio F, Balducci L, Onder G, Ronconi G, et al. (2015) Treating cancer and no-cancer pain in older and oldest old patients.Curr Pharm Des 21: 1706-1714.
- Deandrea S, Montanari M, Moja L, Apolone G (2008) Prevalence of undertreatment in cancer pain. A review of published literature.Ann Oncol 19: 1985-1991.
- Hillegonds DJ, Franklin S, Shelton DK, Vijayakumar S, Vijayakumar V (2007) The management of painful bone metastases with an emphasis on radionuclide therapy.J Natl Med Assoc 99: 785-794.
- WHO | WHO’s cancer pain ladder for adults.
- Zech DF, Grond S, Lynch J, Hertel D, Lehmann KA (1995) Validation of World Health Organization Guidelines for cancer pain relief: a 10-year prospective study.Pain 63: 65-76.
- Gallagher RM (2005) Pain science and rational polypharmacy: an historical perspective.Am J Phys Med Rehabil 84: S1-3.
- Nalamachu SR (2012) Opioid rotation in clinical practice.AdvTher 29: 849-863.
- Lansbury G (2000) Chronic pain management: a qualitative study of elderly people's preferred coping strategies and barriers to management.DisabilRehabil 22: 2-14.
- Balducci L, Colloca G, Cesari M, Gambassi G (2010) Assessment and treatment of elderly patients with cancer.SurgOncol 19: 117-123.
- Decoster L, Van Puyvelde K, Mohile S, Wedding U, Basso U, et al. (2014) Screening tools for multidimensional health problems warranting a geriatric assessment in older cancer patients: an update on SIOG recommendations. Ann Oncol.
- Soubeyran P, Bellera C, Goyard J, Heitz D, Curé H, et al. (2014) Screening for Vulnerability in Older Cancer Patients: The ONCODAGE Prospective Multicenter Cohort Study. PLoS One 9: e115060.
- Saliba D, Elliott M, Rubenstein LZ, Solomon DH, Young RT, et al. (2001) The Vulnerable Elders Survey: a tool for identifying vulnerable older people in the community.J Am GeriatrSoc 49: 1691-1699.
- Meldon SW, Mion LC, Palmer RM, Drew BL, Connor JT, et al. (2003) A brief risk-stratification tool to predict repeat emergency department visits and hospitalizations in older patients discharged from the emergency department.AcadEmerg Med 10: 224-232.
- Barber JH, Wallis JB, McKeating E (1980) A postal screening questionnaire in preventive geriatric care.J R Coll Gen Pract 30: 49-51.
- Overcash JA, Beckstead J, Moody L, Extermann M, Cobb S (2006) The abbreviated comprehensive geriatric assessment (aCGA) for use in the older cancer patient as a prescreen: scoring and interpretation. Crit Rev OncolHematol 59: 205-210.
- Kellen E, Bulens P, Deckx L, Schouten H, Van Dijk M, et al. (2010) Identifying an accurate pre-screening tool in geriatric oncology.Crit Rev OncolHematol 75: 243-248.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 15008
- [From(publication date):
November-2015 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 10357
- PDF downloads : 4651