Superior Mesenteric Vein Thrombosis in a Patient with Immune Thrombocytopenia: Case Report and Review of Literature
Received: 26-Sep-2022 / Manuscript No. JGDS-22-75818 / Editor assigned: 28-Sep-2022 / PreQC No. JGDS-22-75818 (PQ) / Reviewed: 12-Oct-2022 / QC No. JGDS-22-75818 / Revised: 17-Oct-2022 / Manuscript No. JGDS-22-75818 (R) / Published Date: 24-Oct-2022
Abstract
Background: Immune Thrombocytopenia (ITP) is an acquired autoimmune disorder that has a combination of suppressed platelet production and immune mediated platelet destruction. Despite the presence of thrombocytopenia, chronic ITP patients have a higher risk of arterial or venous thromboembolism compared to normal people.
Case presentation: A 37 year old female with a history of steroid resistant chronic ITP presented with severe abdominal pain and massive hematochezia. Upper GI bleeding was diagnosed through nasogastric tube aspiration and esophagogastroduodenoscopy. An abdominal CT scan revealed extensive superior mesenteric vein thrombosis, and small bowel and liver ischemia. She had undergone surgical thrombectomy and small bowel resection. During the hospitalization, she was treated with steroid therapy as well as anticoagulants. Eventually, she required a splenectomy because of a consistent low platelet count. Her platelet count is now stable, and she no longer requires any therapeutic interventions for ITP.
Conclusion: This case is one of the few cases that were reported as paradoxical venous thrombosis in ITP patients. Although arterial and venous thrombosis are considered a rare but potentially life threatening complication of ITP, the therapeutic approach is challenging due to the lack of recommendations and guidelines on the treatment of thrombosis in ITP patients.
Keywords: Immune thrombocytopenia; Mesenteric vein thrombosis; Ischemic hepatitis; Intracranial hemorrhage
Background
Chronic immune thrombocytopenia (ITP) is defined as the persistence of thrombocytopenia for at least 12 months following ITP diagnosis [1]. The clinical presentation of ITP may vary; most patients experience either no or mild bleeding, whereas some patients may experience severe bleeding events like intracranial hemorrhage or severe gastrointestinal bleeding [1]. The exact etiology of ITP is unknown, but it is characterized by increased platelet destruction and suppression of production, which eventually leads to isolated thrombocytopenia [2].
However, chronic ITP patients show a higher incidence of arterial or venous thromboembolism compared to normal people despite the presence of thrombocytopenia [3,4]. Some suggestions for this paradox have been proposed based on the use of the higher proportion of large and young platelets, which may be more thrombotically active [5], and the existence of pro-coagulative platelet derived microparticles (PMPs) [6].
This report not only outlines a rare case but also a potentially, life threatening complication of ITP, which presented superior mesenteric vein thrombosis accompanied by ischemic hepatitis. The consent for publication was obtained from the patient and all the personal information was omitted.
Case Presentation
A 37 year old female presented with a complaint of abdominal pain for the past 10 days. The pain had gradually worsened and was identified to be associated with melena and vomiting before she visited the hospital. After she reached the hospital, she had three times of hematochezia, with a total amount of one liter. Her medical background was significant for treatment resistant ITP with positive anti-GPIIb/IIIa treated with prednisolone and methotrexate, and hypertension treated with clinidipine.
She complained of diffuse, squeezing, cramping abdominal pain, and the numeric rating scale was between 7 and 8. On physical examination, her blood pressure was 119 to 92 mmHg, pulse was 123/min, respiratory rate was 24/min, and body temperature was 36.9℃ (98.4°F). Her conjunctivae were pale and anemic. Abdominal examination revealed diffuse abdominal tenderness, but no rebound tenderness. Digital rectal examination revealed hematochezia with fresh blood, and an L-tube aspirate of gastric juice showed fresh blood as well.
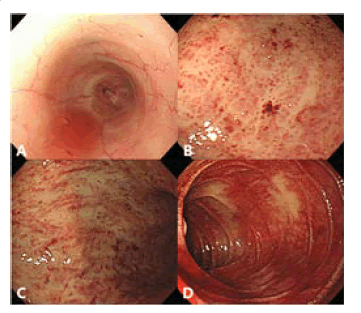
Esophagogastroduodenoscopy showed a large amount of fresh blood in the stomach associated with diffuse erythematous change, suggestive of hemorrhagic gastritis. There was no evidence of focal hemorrhagic lesion. Her esophagus and duodenum were clear (Figure 1).
Figure 1: Esophagogastroduodenoscopy of the patient. (A) No focal lesion was seen in the esophagus. (B, C) Diffuse erythematous change in the stomach wall, suggestive of hemorrhagic gastritis. (D) No focal lesion was seen in the duodenum. The presence of blood is due to hemorrhage of the stomach, and not from the duodenum
Laboratory tests revealed leukocyte count of 47.4 × 103/mL (4-10 × 103/ μL) with 86% of segmented neutrophils, hemoglobin of 14.8 g/dL (12.0- 16.0 g/dL), and platelet count of 12 × 103/mL (150-450 × 103/μL). Initial coagulation studies showed D-dimer value higher than 35.2 mg/L FEU (<0.8 mg/L FEU), fibrinogen degradation product of 31.91 μg/mL (<5 μg/ mL), international normalized ratio (INR) of 1.12 (0.85-1.13), and activated partial thromboplastin time (aPTT) of 26.4 sec (21.0-38.0 sec). Arterial blood gas analysis showed pH of 7.284 (7.35-7.45), bicarbonate ion (HCO3-) of less than 10 mmol/L (21-28 mmol/L), carbon dioxide pressure (PaCO2) of 17.9 mmHg (35.0-48.0 mmHg), and lactic acid of 9.1 mmol/L (0.5-1.6 mmol/L).
Computed tomography (CT) scans of the abdomen and pelvis were done and the results showed extensive portal vein and superior mesenteric vein (SMV) thrombosis that led to infarction and/or ischemic change in the liver segments 6 and 7, and proximal jejunum (Figure 2). There was also mild wall thickening with the mural enhancement of the transverse and ascending colon, consistent with ischemic colitis with mucosal hemorrhage.
Figure 2: CT of abdomen and pelvis, (A, B) axial view, and (C, D) coronal view. (A) Infarction and/or ischemic change in the liver segments 6 and 7 with the subcapsular hepatic fluid collection. (B, C, D) Extensive thrombosis of the portal vein and superior mesenteric vein. Mild wall thickening with the mural enhancement of transverse and ascending colon can be seen along with ischemic colitis with mucosal hemorrhage.
The patient underwent surgical treatment to remove venous thrombus and necrosed bowel. Surgeons checked the location of the thrombus in the portal vein through venography (Figure 3) and performed a thrombectomy of SMV to restore venous blood flow and small bowel resection with an ileostomy for nonviable small bowel. For post-operative care, the patient was admitted to the intensive care unit. Single-donor platelet (SDP) transfusion along with the IVIG and intravenous prednisolone were applied for the treatment of thrombocytopenia. An inferior vena cava (IVC) filter was placed and antithrombin III and lower molecular weight heparin (LMWH) were applied for the treatment of thrombosis.
Despite the continuous transfusion of platelets and application of steroids, there was no enhancement in the platelet count. Therefore, splenic artery embolization was performed to manage the uncontrolled coagulopathy on day 4. Additional workup to rule out the conversion to prothrombotic disorders from ITP was performed and the results were significant for ANA positive at >1:200 with cytoplasmic type and low C3, C4. However, all other results were negative including anti-ADAMTS13, rheumatoid factor, anti- CCP, ANCA, anti-Sm, SS-A, SS-B, Scl-70, Jo-1, Centromere B, dsDNA, RNPs, and anti-cardiolipin.
Despite splenic artery embolization, no improvement in the patients’ clinical status was observed. Moreover, she started to show neurological abnormalities such as altered mental status and seizure like activity on day 14. Electroencephalogram revealed partial seizure, while non-enhanced brain CT showed bilateral subarachnoid hemorrhage and frontal hemorrhage. The patients’ seizure-like activity was treated with the administration of lorazepam and levetiracetam, and further anticoagulation was held because of intracranial hemorrhage.
At this moment, the level of total bilirubin and direct bilirubin were 25.04 mg/dL (0.47-1.58 mg/dL) and 18.51 mg/dL (0.13-0.47 mg/dL), respectively. However, the patients’ abdominal CT did not show any significant dilatation of intrahepatic bile ducts. Therefore, hyperbilirubinemia was considered a complication arising from ischemic injury of the liver parenchyma, and her neurological abnormalities were attributed to the clinical aspect of hyperbilirubinemia. Thus, phenobarbital was applied to improve the metabolism of bilirubin. With improvement in the bilirubin levels, the patient demonstrated alertness. Since she still showed high levels of D-dimer and fibrinogen degradation products, which were consistent with chronic disseminated intravascular coagulation (DIC) with predominant thrombosis, a low dose of enoxaparin administration was restarted followed by warfarin management.
As a result, she showed gradual improvement and was discharged on day 129. Her discharge medications included prednisolone and warfarin. However, there was no improvement in her platelet level and she had multiple episodes of GI bleeding and hypermenorrhea. In addition, she developed deep vein thrombosis (DVT) of the lower extremity vein after holding anticoagulants. Since her thrombocytopenia did not resolve and the patient could not afford rituximab due to its high cost, she eventually underwent laparoscopic splenectomy.
Following splenectomy, her platelet counts gradually increased and remained stable (last count 364 × 103/mL). She is being followed up continuously and on rivaroxaban for thrombosis without any medications on ITP. Since then, she did not experience any further thrombotic episodes.
Conclusion
This case report presents mesenteric vein thrombosis in a patient with ITP, which is paradoxical considering the low platelet count. Since this rare complication can be potentially fatal as well as lead to hemorrhage, the choice between therapeutic approaches to increase platelet counts and anticoagulation to prevent further thrombosis can be of dilemma.
Ethics Approval and Consent to Participate
Institutional Review Board (The Catholic University of Korea School of Medicine) approved the review of medical record.
Consent for Publication
Consent for publication was obtained from the patient according to our institutional consent form.
Availability of Data and Materials
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Competing Interests
The authors declare that they have no competing interests.
Funding
No funding sources.
Authors’ Contributions
YJW, reviewed the medical records and literature and wrote the paper. JYK, treated the patient, collected the data, and carried out critical interpretations. Both authors read and approved the final manuscript.
Acknowledgements
Not applicable.
References
- Fogarty PF (2009) Chronic immune thrombocytopenia in adults: Epidemiology and clinical presentation. Hematol Oncol Clin North Am 23(6):1213-21.
- Johnsen J (2012) Pathogenesis in immune thrombocytopenia: New insights. Hematology Am Soc Hematol Educ Program 306-12.
- Severinsen MT, Engebjerg MC, Farkas DK, Jensen AØ, Nørgaard M, et al. (2011) Risk of venous thromboembolism in patients with primary chronic immune thrombocytopenia: A Danish population-based cohort study. Br J Haematol. 152(3):360-2.
- Nørgaard M, Cetin K, Maegbaek ML, Kristensen NR, Ghanima W, et al. (2016) Risk of arterial thrombotic and venous thromboembolic events in patients with primary chronic immune thrombocytopenia: A Scandinavian population-based cohort study. Br J Haematol 174(4):639-42.
- Cohen YC, Djulbegovic B, Shamai-Lubovitz O, Mozes B (2000) The bleeding risk and natural history of idiopathic thrombocytopenic purpura in patients with persistent low platelet counts. Arch Intern Med 160(11):1630-8.
- Sewify EM, Sayed D, Abdel Aal RF, Ahmad HM, Abdou MA (2013) Increased circulating red cell microparticles (RMP) and platelet microparticles (PMP) in immune thrombocytopenic purpura. Thromb Res 131(2):e59-63.
- Riva N, Donadini MP, Dentali F, Squizzato A, Ageno W (2012) Clinical approach to splanchnic vein thrombosis: Risk factors and treatment. Thromb Rest 130 Suppl 1:S1-3.
- Acosta S, Ogren M, Sternby NH, Bergqvist D, Björck M (2005) Mesenteric venous thrombosis with transmural intestinal infarction: A population-based study. J Vasc Surg 41(1):59-63.
- Hmoud B, Singal AK, Kamath PS (2014) Mesenteric venous thrombosis. J Clin Exp Hepatol 4(3):257-63. Epub 2014 Apr 13.
- Pabinger I, Schneider B (1996) Thrombotic risk in hereditary antithrombin III, protein C, or protein S deficiency. A cooperative, retrospective study. Gesellschaft fur Thrombose- und Hamostaseforschung (GTH) Study Group on Natural Inhibitors. Arterioscler Thromb Vasc Biol 16(6):742-8.
- Morasch MD, Ebaugh JL, Chiou AC, Matsumura JS, Pearce WH, et al. (2001) Mesenteric venous thrombosis: A changing clinical entity. J Vasc Surg 34(4):680-4.
- Thatipelli MR, McBane RD, Hodge DO, Wysokinski WE (2010) Survival and recurrence in patients with splanchnic vein thromboses. Clin Gastroenterol Hepatol 8(2):200-5.
- Kumar S, Kamath PS (2003) Acute superior mesenteric venous thrombosis: One disease or two? Am J Gastroenterol 98(6):1299-304.
- Acosta S, Alhadad A, Svensson P, Ekberg O (2008) Epidemiology, risk and prognostic factors in mesenteric venous thrombosis. Br J Surg 95(10):1245-51.
- Boulware R, Refaai MA (2020) Why do patients with immune thrombocytopenia (ITP) experience lower bleeding events despite thrombocytopenia? Thromb Res 187:154-158.
- Psaila B, Bussel JB, Frelinger AL, Babula B, Linden MD, et al. (2011) Differences in platelet function in patients with acute myeloid leukemia and myelodysplasia compared to equally thrombocytopenic patients with immune thrombocytopenia. J Thromb Haemost 9(11):2302-10.
- Thomsen RW, Schoonen WM, Farkas DK, Riis A, Fryzek JP, et al. (2010) Risk of venous thromboembolism in splenectomized patients compared with the general population and appendectomized patients: A 10-year nationwide cohort study. J Thromb Haemost 8:1413-6.
- Fontana V, Jy W, Ahn ER, Dudkiewicz P, Horstman LL, et al. (2008) Increased procoagulant cell-derived microparticles (C-MP) in splenectomized patients with ITP. Thromb Res 122(5):599-603.
- Swan D, Newland A, Rodeghiero F, Thachil J (2021) Thrombosis in immune thrombocytopenia - current status and future perspectives. Br J Haematol 194(5):822-834.
- Rasheed MA, Alsaud AE, Razzaq S, Fadul A, Yassin MA (2020) Cerebral Venous Thrombosis in a Patient with Immune Thrombocytopenia, an Apparent Paradox. Case Rep Oncol 13(2):588-594.
- Matzdorff A, Beer JH. (2013) Immune thrombocytopenia patients requiring anticoagulation-maneuvering between Scylla and Charybdis. Semin Hematol 50 Suppl 1:S83-8.
- Napolitano M, Saccullo G, Marietta M, Carpenedo M, Castaman G, et al. (2019) Platelet cut-off for anticoagulant therapy in thrombocytopenic patients with blood cancer and venous thromboembolism: An expert consensus. Blood Transfus 17(3):171–80.
Citation: Woo Y, Kim JY (2022) Superior Mesenteric Vein Thrombosis in a Patient with Immune Thrombocytopenia: Case Report and Review of Literature. J Gastrointest Dig Syst 12: 708.
Copyright: © 2022 Kim JY. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 2932
- [From(publication date): 0-2022 - Nov 20, 2025]
- Breakdown by view type
- HTML page views: 2507
- PDF downloads: 425