Research Article Open Access
Suicide Attempts and the Human Development Index in Brazil, 2000- 2014
Davi Félix Martins Junior1,2, Bezerra-Filho S1, Stella Sarmento1, Ângela Miranda-Scippa11Postgraduate in Medicine and Health (PPgMS), Program of Mood and Anxiety Disorders (CETHA) - Federal University of Bahia (UFBA), Salvador, BA, Brazil, Department of Health - State University of Feira de Santana (UEFS), Feira de Santana, BA, Brazil
2Postgraduate in Medicine and Health (PPgMS), Program of Mood and Anxiety Disorders (CETHA) - Federal University of Bahia (UFBA), Salvador, BA, Brazil
- *Corresponding Author:
- Davi Félix Martins Junior
Postgraduate in Medicine and Health (PPgMS), Program of Mood and Anxiety Disorders (CETHA) - Federal University of Bahia (UFBA)
Salvador, BA, Brazil, Department of Health - State University of Feira de Santana (UEFS)
Feira de Santana, BA, Brazil
E-mail: dmartins@uefs.br
Visit for more related articles at International Journal of Emergency Mental Health and Human Resilience
Abstract
Objective: This study aims to verify whether there is a relationship between the Human Development Index (HDI) of Brazil and suicide attempts (SAs) from 2000 to 2014. Methods: Data on SAs and the Brazilian population were extracted from DATASUS, which is available from the Department of Informatics of the Ministry of Health (www.datasus.gov.br). Standardized rates of hospitalization for SAs were calculated for 100,000 (105) inhabitants in the construction of coefficients. Results: The distribution of hospitalization rates shows distinct patterns, with a reduction in most states but growth in some states located in the Northeast region of Brazil. No correlation was found between the HDI and SAs. States in Brazil's less-developed regions (the Northeast and North) showed lower HDI values and had higher variability in the hospitalization rates due to SAs. The risk of hospitalization was higher for men. Conclusion: No correlation was found between the HDI and SAs, probably because of the great variability of hospital admissions attributable to SAs in low-HDI states. In those states, the stability of hospital admission rates can be affected by a lack of uniformity in registers, among other factors. Further studies should investigate this great variability in hospital admission rates.
Keywords
Suicide attempts, Brazil, Methods of suicide, Hospitalization, Trend, Geographical distribution
Background
Suicide, an intentional, self-inflicted act that results in death, is considered a major public health problem. It is currently the second leading cause of death worldwide among persons aged between 15 and 29 years [1]. In 2012, 803,894 people died by suicide, amounting to one death every 40 seconds (World Health Organization (WHO), 2014). The World Health Organization (WHO) estimates that in 2020 approximately 1.5 million people will die by suicide (Bertolote, Fleischmann, 2002); these data do not include suicide attempts (SAs), which are estimated to occur 20 times more often than completed suicides (World Health Organization (WHO), 2008).
Depending on the method employed, a SA might not require medical attention, and the victim often remains in his or her home environment; such case of SA are not included in official statistics (Alberdi-Sudupe et al., 2011). Sometimes, the person who made the SA is treated on an outpatient basis. Finally, if the gravity of the act results in an increased risk of death or requires intensive treatment for the victim, his or her hospitalization is recorded for technical, administrative and financial reasons.
The Hospital Information System of Brazil’s Unified Health System (SIH/SUS) manages data derived from hospitalizations in public health facilities and/or contracted services. Brazil has a nationwide network of public and/or contracted hospitals that covers approximately 80% of the country’s hospital admissions (HAs), with coverage varying among regions and states depending on population user health plans (Pepe, 2009). Brazil’s distribution of public and private services is uneven because of intraregional inequalities (Paim et al., 2011) and the concentration of income and population in large and medium-sized cities.
One measure used to assess geographic inequalities in living conditions is the United Nation’s Human Development Index (HDI). The HDI is an index consisting of three indicators – income, education and longevity – that are used to characterize the average living conditions of a given population. Both low income and low education levels are related to an increased risk of SA (Avanci, Pedrão & Costa Júnior, 2005; Vidal, Gontijo & Lima, 2013).
Data from Human Development reports released in 2000 and 2010 show that the states with the worst HDI values are located in Northern and Northeastern Brazil, which record the worst socioeconomic indicators. Median values were found in Brazil’s midwestern states, and the best results were exhibited in the more developed southeastern and southern states. The geographic inequality revealed by this indicator reflects the various living conditions of the population, which are closely related to social and economic factors. The HDI strongly influences the quality of both vital statistics (Paes, 2005) and related health events, such as HAs.
Considering that the environment can interfere with a person’s biopsychosocial well-being and that the HDI reflects a given population’s socioeconomic conditions, our first goal was to investigate whether there is an association between the HDI and HAs that is attributable to the SA rate. The second purpose of this study was to verify the spatial and temporal distribution of HAs resulting from SAs in persons 10 years or older for the period from 2000 to 2014. To our knowledge, no other study has investigated this association.
Methods
This study was an ecological analysis of multiple groups (Medronho, 2009). The units of analysis were Brazil’s 26 states plus the Federal District. Brazil’s states are autonomous political administrative units in a federal system, each consisting of a group of municipalities and the capital, which is the seat of the government. The Federal District is an autonomous territory consisting of 30 satellite towns and Brasilia, which is both the federal capital and the Federal District’s seat of government.
The SIH/SUS records hospitalization data in public and/or contract services. A primary source of information in this system is the Hospitalization Authorization Form (AIH), which is required for every HA in the SUS, providing data that allow us to describe not only morbidity and hospital mortality but also associated costs.
Data on HAs resulting from SAs from 2000 to 2014 were collected and coded based on the International Classification of Diseases and Related Health Problems ICD-10, using the X60-X84 codes that correspond to suicide or self-harm. For this study, all SA data included persons aged 10 years and older. The database that we used was MS/SVS/DASIS-SIH/DATASUS 2012 (Ministry of Health: Information health database on the internet).
Three indicators were calculated. First, we calculated the rate of HAs attributable to SAs for three periods - 2000-2004, 2005-2009 and 2010-2014 - along with the percentage of change between each period. Second, we calculated the rate of HAs attributable to SAs stratified by age group: 10-14 years (children), 15-24 years (young), 25-34 years (young adults), 35-44 years and 45-54 (adults), 55-64 (middle-aged), and 65 and older (elderly). The third indicator was the rate of HAs attributable to SAs by sex for the period 2010-2014. The rates were standardized according to the Brazilian demographic census for the year 2000. For the construction of all three indicators, we adopted the mid-term population and the multiplication factor of 100,000 people (105).
Statistical analysis was done using the Spearman correlation test to verify correlation between the HDI and HAs attributable to SAs.
Results
The results were obtained through SUS, with 49,478 HA events attributable to SAs in persons aged 10 years or older from 2000 to 2004, corresponding to an overall rate of 35.2 cases per 105 inhabitants. Of the total HAs, 58.5% occurred in the Southeast region, with an average rate of 47.1 cases per 105 inhabitants, whereas in the Midwest region, 3,740 admissions were recored, with an average rate of 38.6 cases per 105 inhabitants. The risk of hospitalization for a SA in the Southeast was 1.34 times the average rate observed for the rest of the country. During the period studied, the rates ranged from 1.4 cases per 105 inhabitants in the state of Pernambuco to 133.0 cases per 105 inhabitants in the state of Acre. Also noteworthy are the states of Paraíba and Minas Gerais, with 89.3 and 81.2 cases per 105 inhabitants, respectively.
In the second period (2005-2009), there were 44,180 admissions for SAs, with an average rate of 28.4 cases per 105 inhabitants. The Southeast region recorded 24,912 cases, or 56.4% of total admissions, with a rate of 36.8 cases per 105 inhabitants, followed by the North with 6,598 cases, corresponding to a rate of 55.4 cases per 105 inhabitants. The risk of hospitalization in the Northern region was 1.5 times higher than in the Southeast region and 2.0 times higher than the national average. The states of Acre and Pará registered the highest rates: 425.3 and 67.1 cases, respectively, per 105 inhabitants. The state of Pernambuco continued to record the lowest rate, with 1.6 cases per 105 inhabitants, followed by the states of Maranhão, Roraima and Amazonas, with 3.0, 3.8 and 5.2 cases, respectively, per 105 inhabitants.
There were 40,766 HAs due to SAs in the most recent period (2010-2014), corresponding to an overall rate of 24.8 cases per 105 inhabitants. The Southeast region presented the highest rate, with 33.2 cases per 105 inhabitants. In this region, 23,413 people were hospitalized for SAs, accounting for 57.4% of the total, whereas the Midwest region had the fewest admissions, 2,539, with an average rate of 20.9 cases per 105 inhabitants. Rates among the states ranged from 2.4 cases per 105 inhabitants in Roraima to 112.4 cases per 105 inhabitants in Acre; both states are located in the Northern region of Brazil. High rates of 59.5 and 50.3 cases per 105 inhabitants were observed in the states of Espirito Santo in the Southeast and Ceara in the Northeast, respectively.
The rates increased only in the North region between the first and second period (24.4%). The states located in this region show different trends, with growth of approximately 219.8% in Acre and a reduction of 83.3% in Tocantins. In the Northeast, rates increased 16.9% in the state of Pernambuco, 53.7% in Alagoas, and 75.7% in Piauí, while decreasing in the other states. In the other regions, reductions were observed in all states except Espírito Santo in the Southeast, which increased by 3.2%, and Parana in the South, which increased by 5% increase. Between the second and third period there was a decrease of approximately 9.9% in the Southeast, reaching a maximum of 63% in the North. This reduction pattern contrasts with the Northeast region, which recorded an increase in the average rate of 35.4%. In this region, there were sharp increases in the states of Pernambuco, Ceará and Maranhão of 489.8%, 424.9%, and 173.3%, respectively. Conversely, in the state of Piauí, the rate decreased to 22.4%. The state of Espírito Santo experienced an increase of approximately 79.3%, which is a very different result from the observed reduction in Rio de Janeiro of 44.6%; both states are located in the same region.
Most of the states in the Northeast region presented growth in the rates of HAs attributable to SAs between the first and third period, especially Pernambuco (589.4%, from 1.4 to 9.5 cases per 105 inhabitants) and Maranhão (325.5%, from 3.7 to 15.6 cases per 105 inhabitants). This trend contrasts with the reduction observed in Paraíba (89.6%, from 89.3 to 9.3 cases per 105 inhabitants), and Rio G. do Norte G (63.8%, from 11.7 to 4.2 cases per 105 inhabitants).
There was a decrease of the rates in all of states in the North, Southeast, South and Midwest regions, ranging from 9.5% in São Paulo (39.7 to 36.0 cases per 105 inhabitants) to 85.7% in Tocantins (73.9 to 10.5 cases per 105 inhabitants). Espirito Santo, located in the Southeast region, recorded an increase of 85%, from 32.2 to 59.5 cases per 105 inhabitants.
Of the 134,425 hospital admissions due to suicide attempts 4,932 (3.7%) resulted in death, of which 66.3% occurred in the Southeast region. In the state of Roraima there was no death recorded. The states of São Paulo and Minas Gerais recorded the highest number of deaths, 1636 and 1194, respectively. The HDI was moderately correlated with five years rates of SAs 0.31 (first period 2000-2004) and 0.28 in the last period (2010-2014); however, this correlation was not statistically significant (Table 1). The correlation between complete suicide and hospitalization due suicide attempt was negative -0.932, as well the correlation between complete suicide and hospitalization due suicide attempt for male (-0.881) and female (-0.881), p = 0.000. Only for age group from 45 to 54 years old, the correlation between complete suicide and hospitalizations due suicide attempt was positive (0.072), but was not statistically significant.
| Region/States | 2000/2004 | 2005/2009 | 2010/2014 | Var% | Var% | Var% | HDI ŧ | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (2/1) | (3/2) | (3/1) | - | - | |||||
| n | rate | n | rate | n | rate | 2000 | 2010 | |||||
| N | 4506 | 44.6 | 6598 | 55.4 | 2677 | 20.5 | 24.4 | -63.0 | -54.0 | - | - | |
| RO | 274 | 24.8 | 225 | 17.8 | 265 | 20.1 | -28.3 | 13.1 | -18.9 | 0.537 | 0.690 | |
| AC | 573 | 133.0 | 2254 | 425.3 | 660 | 111.2 | 219.8 | -73.9 | -16.4 | 0.517 | 0.663 | |
| AM | 243 | 11.2 | 135 | 5.2 | 146 | 5.1 | -53.6 | -0.2 | -53.7 | 0.515 | 0.674 | |
| RR | 12 | 4.7 | 12 | 3.8 | 9 | 2.4 | -18.5 | -36.3 | -48.1 | 0.598 | 0.707 | |
| PA | 2596 | 53.6 | 3787 | 67.1 | 1422 | 22.7 | 25.2 | -66.1 | -57.5 | 0.518 | 0.646 | |
| AP | 123 | 32.6 | 52 | 11.0 | 53 | 9.6 | -66.3 | -12.5 | -70.5 | 0.577 | 0.708 | |
| TO | 685 | 73.9 | 133 | 12.3 | 122 | 10.5 | -83.3 | -14.6 | -85.7 | 0.525 | 0.699 | |
| NE | 6935 | 18.1 | 5919 | 14.1 | 8588 | 19.1 | -21.7 | 35.4 | 5.9 | - | - | |
| MA | 161 | 3.7 | 144 | 3.0 | 838 | 15.6 | -19.0 | 424.9 | 325.5 | 0.476 | 0.639 | |
| PI | 158 | 6.9 | 297 | 12.2 | 392 | 14.9 | 75.7 | 22.4 | 115.0 | 0.484 | 0.646 | |
| CE | 1237 | 20.7 | 1235 | 18.4 | 3643 | 50.3 | -11.0 | 173.3 | 143.2 | 0.541 | 0.682 | |
| RN | 265 | 11.7 | 203 | 8.1 | 115 | 4.2 | -30.7 | -47.8 | -63.8 | 0.552 | 0.684 | |
| PB | 2493 | 89.3 | 1948 | 65.2 | 297 | 9.3 | -27.0 | -85.8 | -89.6 | 0.506 | 0.658 | |
| PE | 89 | 1.4 | 113 | 1.6 | 712 | 9.5 | 16.9 | 489.8 | 589.4 | 0.544 | 0.673 | |
| AL | 119 | 5.4 | 197 | 8.3 | 122 | 4.7 | 53.7 | -42.9 | -12.2 | 0.471 | 0.631 | |
| SE | 313 | 21.7 | 295 | 18.3 | 214 | 12.2 | -15.9 | -33.2 | -43.9 | 0.518 | 0.665 | |
| BA | 2100 | 19.8 | 1487 | 13.1 | 2255 | 19.0 | -34.2 | 45.1 | -4.5 | 0.512 | 0.660 | |
| SE | 28937 | 47.1 | 24912 | 36.8 | 23413 | 33.2 | -21.8 | -9.9 | -29.6 | - | - | |
| MG | 12150 | 81.2 | 8616 | 52.4 | 7124 | 41.6 | -35.5 | -20.5 | -48.7 | 0.624 | 0.731 | |
| ES | 839 | 32.2 | 969 | 33.2 | 1820 | 59.5 | 3.2 | 79.3 | 85.0 | 0.640 | 0.740 | |
| RJ | 3384 | 27.6 | 2400 | 18.1 | 1416 | 10.0 | -34.4 | -44.6 | -63.7 | 0.664 | 0.761 | |
| SP | 12564 | 39.7 | 12927 | 36.9 | 13053 | 36.0 | -7.1 | -2.6 | -9.5 | 0.702 | 0.783 | |
| S | 5360 | 25.4 | 4053 | 17.4 | 3541 | 14.8 | -31.6 | -15.1 | -41.9 | - | - | |
| PR | 1384 | 17.4 | 1607 | 18.3 | 1396 | 15.4 | 5.0 | -15.9 | -11.7 | 0.650 | 0.749 | |
| SC | 1527 | 33.8 | 980 | 19.2 | 1187 | 21.5 | -43.2 | 11.9 | -36.5 | 0.674 | 0.774 | |
| RS | 2449 | 28.4 | 1466 | 15.6 | 958 | 10.2 | -45.2 | -34.4 | -64.1 | 0.664 | 0.746 | |
| C-O | 3740 | 38.6 | 2698 | 24.3 | 2547 | 20.9 | -36.9 | -14.0 | -45.7 | - | - | |
| MS | 590 | 34.5 | 393 | 20.5 | 324 | 15.4 | -40.5 | -25.1 | -55.5 | 0.613 | 0.729 | |
| MT | 726 | 35.2 | 344 | 14.6 | 387 | 14.9 | -58.7 | 2.1 | -57.8 | 0.601 | 0.725 | |
| GO | 1506 | 35.9 | 1426 | 29.7 | 1160 | 22.2 | -17.4 | -25.1 | -38.1 | 0.615 | 0.735 | |
| DF | 918 | 52.9 | 535 | 26.7 | 676 | 30.1 | -49.5 | 12.7 | -43.1 | 0.725 | 0.824 | |
| Brasil | 49478 | 35.2 | 44180 | 28.4 | 40766 | 24.8 | -19.3 | -12.7 | -29.6 | 0.612 | 0.727 | |
Source: Ministry of Health - System SUS Hospital Information (SIH/SUS).
*People aged 10 years or older.
State of national database on 09/29/2015. August 2014.
Data through August 2015, subject to rectification.
Where: N-North region (AC - Acre, AM - Amazonas, AP - Amapá, PA – Pará, RO – Rondônia, RR – Roraima, TO - Tocantins); NE-Northeast region (AL - Alagoas, BA – Bahia, CE - Ceará, MA - Maranhão, PB - Paraíba, PE - Pernambuco, PI – Piauí, RN - Rio Grande do Norte, SE - Sergipe); C-O-Midwest region (DF - District Federalŧ-Brasilia, GO - Goiás, MS - Mato Grosso do Sul, MT - Mato Grosso); SE-Southeast region (ES - Holy Ghost, MG - Minas Gerais, Rio de Janeiro - Rio de Janeiro, São Paulo - São Paulo); S-South region (PR – Paraná, RS - Rio Grande do Sul, SC - Santa Catarina). These codes were adopted by the IBGE - Brazilian Institute of Geography and Statistics.
ŦHDI - Human Development Index.
Five-year rate set by the Brazilian Population Demographic Census of 2000.
Table 1. Hospitalization in SUS attributable to suicide attempts * (number, rate per 105 inhabitants, variation %) in Brazil, states, Federal District and the HDI
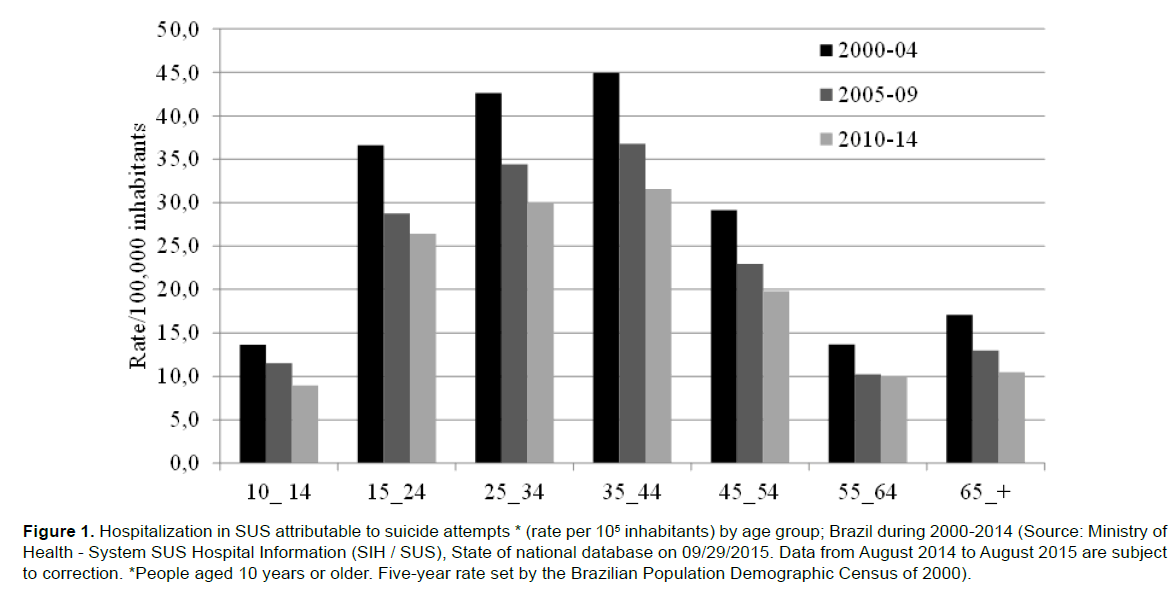
In the 15-34 age groups, there were 65,042 HAs attributable to SAs, corresponding to 48.4%, with the lowest number found in children aged 10-14 years of age, accounting for 5,926 admissions (4.4%). The 35-44 age group presented the highest rates of 44.9, 36.8 and 31.6 cases per 105 inhabitants in the first, second and third periods, respectively. These rates decreased between the first and second periods, varying from 15.3% in children to 25% in middleaged (55-64 years of age) individuals; between the second and third period, rates fell 3.1% in middle-aged people (55-64 years of age) and 19.5% in the elderly (65 years of age). Reductions of greater magnitude occurred between the first and third period, ranging from 27.8% in young adults (15-24 years of age) to 38.7% in the elderly.
The rates increased from the group of children (10-14 years of age) to adults (35-44 years of age) and then decreased with the elderly. The risk of hospitalization in the group of persons 35-44 years of age was 3.3 times higher than in the group of children and 2.8 times higher than in the elderly (Figure 1).
Figure 1. Hospitalization in SUS attributable to suicide attempts * (rate per 105 inhabitants) by age group; Brazil during 2000-2014 (Source: Ministry of Health - System SUS Hospital Information (SIH / SUS), State of national database on 09/29/2015. Data from August 2014 to August 2015 are subject to correction. *People aged 10 years or older. Five-year rate set by the Brazilian Population Demographic Census of 2000).
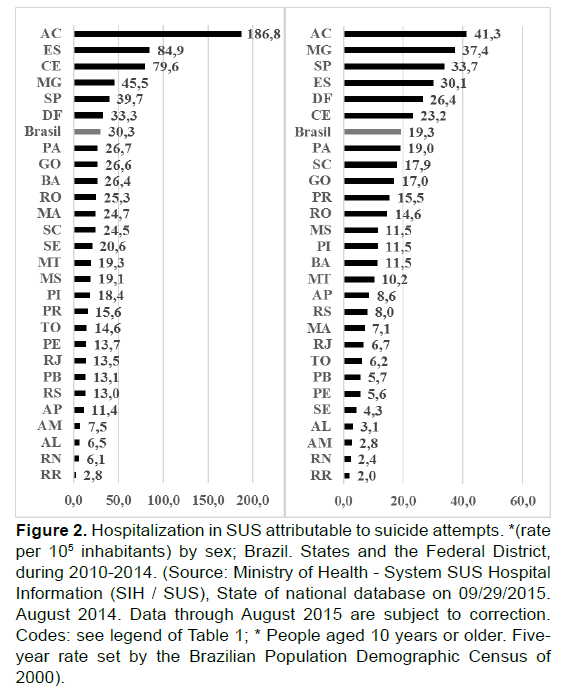
In the period 2010-2014, HAs attributable to SAs rate was 30.3 cases per 105 inhabitants for men and 19.3 cases per 105 inhabitants for women, yielding a male/female ratio of 1.6. Acre presented the highest rate in men, with 186.8 cases per 105 inhabitants, followed by Espirito Santo, with 84.9 cases per 105, and Ceará, with 79.6 cases per 105 inhabitants. Roraima, located in the North region, presented the lowest rate of 2.8 cases per 105 inhabitants, followed by Rio G do Norte with 6.1 cases per 105 inhabitants and Alagoas with 6.5 cases per 105 inhabitants. Both, Rio G do Norte and Alagoas are located in the Northeast region.
Among women, the highest HA rates attributable to SAs were recorded in Acre, Minas Gerais and São Paulo with 41.3, 37.4 and 33.7 cases per 105 inhabitants, respectively, and the lowest rates were recorded in Roraima, Rio G do Norte and Amazonas with rates of 2.0, 2.4 and 2.8 cases per 105 inhabitants, respectively.
In all states, men were hospitalized more often than women, with the highest ratio observed in the state of Sergipe, with 4.8 (20.6 versus 4.3 cases per 105 inhabitants), followed by Acre with 4.5 (186.8 versus 41.3 per 105 inhabitants), Maranhão with 3.5 (24.7 versus 7.1 per 105 inhabitants), and Ceará States with 3.4 (79.6 versus 23.2 per 105 inhabitants). In Paraná, the ratio was 1.0, indicating that the risk of hospitalization (whether in public health units and/or contracted facilities) for injuries resulting from a SA was the same for both sexes (Figure 2).
Figure 2. Hospitalization in SUS attributable to suicide attempts. *(rate per 105 inhabitants) by sex; Brazil. States and the Federal District, during 2010-2014. (Source: Ministry of Health - System SUS Hospital Information (SIH / SUS), State of national database on 09/29/2015. August 2014. Data through August 2015 are subject to correction. Codes: see legend of Table 1; * People aged 10 years or older. Fiveyear rate set by the Brazilian Population Demographic Census of 2000).
Discussion
This study aimed to examine the association between the HDI and HAs attributable to SAs and to verify the spatial and temporal distribution of HAs attributable SAs in persons 10 years or older by investigating data collected by public health services from 2000 to 2014.
No correlation between the HDI and HAs attributable to SAs was found. However, the states with the lowest HDI showed greater variability in rates of hospitalization for SAs. In less-developed areas, health services are less organized, which could explain why we find this great variability of rates in states located in the less-developed regions. We did not observe correlation between complete suicide and suicide attempts as well as this correlation according to gender and age group.
In a study analyzing suicide trends in various countries (Levi et al., 2003), the authors concluded that finding a common cause was impossible. The conditions implicated in SAs are diverse and include mental disorder, easy access to the means to commit suicide, religion, socioeconomic instability, poverty and unemployment. On average, three out of four suicides in 2012 occurred in low-income, low-HDI countries (World Health Organization, 2016). However, our data show that the Brazilian states with lower HDI rates showed low HAs rates for SAs in relation to the national average, but more variability in rates for the periods studied. However, developed areas, such as the Federal District and São Paulo, which have the highest HDI rates in the federation, recorded high rates of HAs attributable to SAs. In the states located in the most developed regions of the country (the South and Southeast regions), the rates appeared stable, which might be related to more reliable data.
Another aspect that could influence the differences is the availability of beds for hospitalization in emergency services, which can vary both among and within states. Large and mediumsized cities in Brazil that are more concentrated in the regions with higher HDI values historically have increased both the availability of emergency-unit hospital beds and human and technological resources to perform health services. In less-developed regions, such as the North and Northeast, the spatial distribution of health services, especially those of medium and high complexity, is geographically more scarce and concentrated. However, this concentrated pattern has been changing in recent years given the ongoing policy of spatial deconcentration of services and, consequently, of health professionals in the territory.
Geographical barriers, such as distance between the city in which a SA occurred and the city that offers urgent care also can explain the temporal variability in rates in that the places where attempts occur do not always correspond to the places where the person receives care.
Furthermore, suicide is a stigmatized social event that favors the omission of cases. Suicide is a complex phenomenon in relation to religious, cultural and social norms. For that reason, there is a decreased likelihood that a death will be classified as suicide when there is no explicit expression of suicidal intent; this practice varies by culture and epoch (Björkenstam et al., 2014). Death by suicide might be recorded as death from undetermined causes, leading to underreporting (Pavia et al., 2005), and we believe that this problem applies to SAs.
The analysis of geographical and temporal trends in SAs requiring hospitalization showed wide variation among states and regions. The South, Southeast and Midwest regions presented the highest HDI values, with rates varying less among the states in those regions and a reduced temporal pattern, except in Espirito Santo, located in the Southeast, which had a rate that increased by 85% in the period studied (32.2 cases per 105 inhabitants to 59.5 cases per 105 inhabitants).
We found significant variations among the states with the lowest HDI values located in the North and Northeast regions. In the North region, rates varied widely among the states, with the most significant differences in the second period. The reduction of rates in every state defines the temporal pattern. Acre, located in the North region, recorded the highest rates in the three periods. When compared with the rates in other states, Acre’s rate of HAs attributable to SAs was exceptionally high, indicating a need for detailed studies to explain the high risk of hospitalization.
The states located in the Northeast region showed a significant change in rates, especially in Pernambuco, Maranhão and Ceará, where the temporal pattern was expressed by strong growth movements in some states, in contrast to the variable reduction observed in others. Significant variability undermines the reliability of the data and may be attributable to an underreporting of the secondary instability of health information records that is typical of underdeveloped regions, such as the North and Northeast regions, which comprise the temporal trend analysis.
Among age groups, the distribution of rates shows growth with advancing age, reaching its peak in the adult group of 35-44 years of age and decreasing with the elderly. Our findings are consistent with other studies (Chau, Kabuth & Chau, 2017; Swahn et al., 2012). Decreases in all age groups defined the temporal patterns, which were higher both in the elderly and in children. The rates in the elderly were higher than in middle-aged people. The trend of attempting suicide varies among age groups; affective factors are predominant among the young, socioeconomic problems are predominant among adults and middle-aged people, and the difficulty of dealing with aging, loss and health problems are predominant among the elderly.
Except in Paraná, the highest rates of HA were found among men. Although men are hospitalized more often than women, the differences were not very great, except in Sergipe and Acre, where the admission rates for men were 4.8 and 4.5 times higher than for women, respectively. These findings contradict the literature, which reports a higher risk of SA in women than in men (Tsirigotis, Gruszczynski & Tsirigotis, 2011; Callanan & Davis, 2012). We must note that data from this study refer to serious attempts that required hospitalization, perhaps explaining why hospitalization risk was higher for men. The average risk of HA for men was 3.0 when violent methods were used, whereas it was only 1.3 when nonviolent methods were used. By contrast, women tend to opt for less violent methods in their attempts, with a lower risk of death. In this study, women have made greater use of medical substances, whereas men have made greater use of non-medical substances, such as alcohol, solvents, gases and vapors, pesticides and other chemicals, and unspecified harmful substances.
The choice of method used—violent methods for men versus non-violent methods for women—explains not only the differences in the risk of suicide but also the sex risk of HAs attributable to SAs (Värnik et al., 2011; Pommereau, 2012).
Regardless of the method employed—violent or non-violent— men have higher rates of HAs attributable to SAs. This result might be because regardless of the method used, the intensity of the technique applied is greater among men.
What This Study Adds
To the best of our knowledge, this study is the first to connect HA rates for SAs (disaggregated by states and the Federal District) with the HDI. In addition, an analysis of the geographical and temporal distribution was conducted of HA rates for injuries resulting from SAs in Brazil.
Limitations
One limitation is the use of a macro analysis unit, i.e., the states. A smaller unit would provide space closer to local reality. The data’s One limitation is the use of a macro analysis unit, i.e., the states. A smaller unit would provide space closer to local reality. The data’s focus on a single method related to public and/or contracted services is another limitation that could exclude other sources of inpatient admissions; for this reason, the results should be analyzed with caution. The main limitation of this approach is that the data could be underestimating reality, although the public subsector responds by providing the absolute majority of Brazil’s HAs.
Conclusions
No correlation was found between the HDI and the HAs attributable to SAs, as well between complete suicide ans SAs. However, the states with lower HDI values are those with greater variability in the HA rates for SA. This finding suggests that low socioeconomic conditions could interfere with the quality of hospital data, which points to the need for targeted actions to improve the quality of registration data in those states.
The results of this study have identified the states with the highest risk of hospitalization for injuries resulting from SAs, public, and contracted services and the geographical distribution by sex, age and method used.
The rates varied among the states, especially in the less-developed regions, while remaining stable in other regions. The temporal pattern was characterized by a reduction of HAs attributable to SAs in the absolute majority of the states. The risk of hospitalization was higher in men. This finding may be because only cases with an increased risk of death lead to hospitalization. Hospitalization results from the use of more lethal methods or milder methods committed with greater intensity.
This type of study leaves room for future investigations that focus on smaller units as municipalities and thus can identify the exact county in which the SA occurred. This research could help local health agencies develop strategies to prevent and respond to SAs that require more effective and appropriate HA.
Funding
This study did not receive any funding. The data are in the public domain.
Authors’ Contributions
DFMJ participated in developing the study conception and design, data analysis and interpretation, drafting the article. SS - performed a relevant critical review of the intellectual content. SB-F and AM-S participated in the drafting the article, revising it critically for important intellectual content and final approval of the version to be published. All authors read and approved the final manuscript.
Competing Interests
The authors declare that they have no competing interests.
Acknowledgement
Nature Publishing Group Language Editing by revision of English.
References
- World Health Organization (WHO). (2014). Preventing suicide: A global imperative. Luxembourg: WHO
- Bertolote, J.M. & Fleischmann, A. (2002). A global perspective in the epidemiology of suicide. Suicidologi, 7(2), 6-8
- World Health Organization. (2008). World report on violence and health. Geneva: World Health Organization
- Alberdi-Sudupe, J., Pita-Fernández, S., Gómez-Pardiñas, S.M., Gil-de-Bernabé, F.I., García-Fernández, J., Martínez-Sande, G., et al., (2011). Suicide attempts and related factors in patients admitted to a general hospital: a ten-year cross-sectional study (1997-2007). BMC Psychiatry, 11, 51
- Pepe, V.E. (2009). System of hospital information of the Unified Health System (SIH-SUS). In: Brazil. Ministry of Health (MS). The Brazilian experience in health information systems. Brasilia: MS, 65-86
- Paim, J, Travassos, C., Almeida, C., Bahia, L. & Macinko, J. (2011). The Brazilian health system: history, advances, and challenges. The Lancet, 377(9779), 1778–1797, 21
- Avanci, R.C., Pedrão, L.J. & Costa Júnior, M.L. (2005). Perfil do adolescente que tenta suicídio em uma unidade de emergência. Rev Bras Enferm, 58, 535-539
- Vidal, C.E.L., Gontijo, E.C.D.M. & Lima, L.A. (2013). Attempted suicide: prognostic factors and estimated excess mortality] [Article in Portuguese] Cad. Public Health, Rio de Janeiro, 29(1), 175-187
- Paes, N.A. (2005). Evaluation of the coverage of death registries of the Brazilian states in 2000. Rev Public Health, 39(6), 882-890
- Medronho, R.A. (2009). Ecological Studies in: Epidemiology Roberto de Andrade Medronho ... São Paulo: Editora Athneu, 265-269
- Ministry of Health: Information health database on the internet. Brasilia: MS
- Levi, F., La Vecchia, C., Lucchini, F., Negri, E., Saxena, S., Maulik, P.K., et al., (2003). Trends in mortality from suicide, 1965–99. Acta Psychiatr Scand, 108, 341-349
- World Health Organization. (2016). Mental Health
- Björkenstam, C., Johansson, L.A., Nordström, P., Thiblin, I., Fugelstad, A., Hallqvist, J., et al., (2014). Suicide or undetermined intent? A register-based study of signs of misclassification. Population Health Metrics, 12, 11
- Pavia, M., Nicotera, G., Scaramuzza, G., Angelillo, I.F. & The Collaborative Group. (2005). Suicide mortality in Southern Italy: 1998–2002 Psychiatry Res, 134, 275– 279
- Chau, K., Kabuth, B. & Chau, N. (2014). Gender and Family Disparities in Suicide Attempt and Role of Socioeconomic, School, and Health-Related Difficulties in Early Adolescence. BioMed Research International, 2014, 314521.
- Swahn, M.H., Bossarte, R.M., Choquet, M., Hassler, C., Falissard, B. & Chau, N. (2012). Early substance use initiation and suicide ideation and attempts among students in France and the United States, Int J Public Health, 57(1), 95-105
- Tsirigotis, K., Gruszczynski, W. &Tsirigotis, M. (2011). Gender differentiation in methods of suicide attempts. Med Sci Monit, 17, H65–70
- Callanan, V.J. & Davis, M.S. (2012). Gender differences in suicide methods. Soc Psychiatry Psychiatr Epidemiol, 47(6), 857-869
- Värnik, A., Sisask, M., Värnik, P., Wu, J., Kõlves, K., Arensman, E., et al., (2011). Drug suicide: a sex-equal cause of death in 16 European countries. BMC Public Health, 11, 61
- Pommereau, X. (2012). Life-threatening behaviors, suicide, attempted suicide and self-inflicted injury. Bull Acad Natl Med, 196(2), 357-369.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 3799
- [From(publication date):
March-2017 - Jul 04, 2025] - Breakdown by view type
- HTML page views : 2877
- PDF downloads : 922