Successful Treatment of a Symptomatic Unicameral Calcaneus Bone Cyst by Cement Injection Using a Double Needle Technique under CT Guidance: A Case Report
Received: 07-Jan-2022 / Manuscript No. CRFA-21-49068 / Editor assigned: 10-Jan-2022 / PreQC No. CRFA-21-49068 (PQ) / Reviewed: 24-Jan-2022 / QC No. CRFA-21-49068 / Revised: 31-Jan-2022 / Manuscript No. CRFA-21-49068 (R) / Accepted Date: 02-Feb-2022 / Published Date: 04-Feb-2022 DOI: 10.4172/2329-910X.1000327
Abstract
Simple bone cysts (SBCs) are benign cavitary lesions which most commonly affect adolescent males in the first two decades of life. They are mainly asymptomatic, but can manifest with pain or pathological fractures. A 16-year old girl presented with an 8-day history of pain and swelling over the right calcaneal region. On local examination, tenderness was the only noteworthy sign and all routine laboratory tests conducted revealed normal results. Routine lab evaluations were all within normal limits. No history of trauma to the calcaneal region and no family history of other pathological conditions were reported. Despite numerous proposed methods for the management of calcaneus SBCs, the optimal approach towards these lesions remains controversial. Here, a novel method utilizing a minimally invasive technique is proposed to successfully manage these lesions. In an outpatient setting, under conscious sedation and local anestethics, two interosseous needles were simultaneously inserted percutaneously into the cyst under the guidance of CT fluoroscopy. Unlike previous techniques, aspiration was only performed to reveal serosanguineous fluid content. Then a radiopaque bone cement mixture was injected into the cyst from one needle until the cessation of serosanguineous fluid efflux from the second needle. The procedure was performed under fluoroscopy control to warrant complete replacement of cyst content with cement material. The duration of the procedure was estimated to be 15 minutes and the total dose length product (DLP) and smartview DLP were 577.9 mGy*cm and 13 mGy*cm, respectively. The patient experienced itching and warmth at the site of the procedure immediately after the intervention. 3 weeks after the procedure, the injection site healed smoothly and the patient reported pain with weight bearing activities and limping after prolonged standing. Over a one-year follow-up period, the patient recovered without any complications. Bone cement injection using a double needle technique under CT fluoroscopy guidance is a feasible and safe method to treat symptomatic unicameral calcaneal bone cysts.
Keywords
Simple bone cyst, percutaneous cement injection, minimally invasive treatment, unicameral bone cyst of the calcaneus, case report, double needle technique, CT fluoroscopy guidance
Abbreviations: SBC - Simple bone cyst; UBC - Unicameral bone cyst ; CT - Computed tomography; MRI - Magnetic resonance imaging; CBC - Complete blood counts; ESR - Erythrocyte sedimentation rate; BUN - Blood urea nitrogen; HA – Hydroxyapatite; DLP - Dose length product
Introduction
Simple bone cysts (SBCs) are benign cavitary lesions within the metaphysical region of bones [1]. They can be unicameral (single chamber) or with partial septations [2]. Unicameral bone cysts are well-defined cystic cavities filled with serious or serosanguineous fluid, which is lined by a fibrovascular connective tissue membrane [2,3]. The precise etiology of UBCs has not been determined, but some researchers have suggested that venous outflow obstruction may be responsible for cystic cavitation filled with fluid [4,5]. These lesions most commonly affect children and adolescent males (with a 2-3:1 male to female ratio) in the first two decades of life, are most often observed in the proximal regions of the humerus and femur (accounting for up to 80% of cases) and are relatively uncommon in the calcaneus [5-7]. UBCs of the calcaneus mostly arise from the anterolateral aspect of the bone, far away from the area in which most of the body weight is transmitted [8]. Although these lesions are mainly asymptomatic, they can present with pain or pathological fractures due to structural weakness [3]. The patient’s age has been shown to have the greatest impact on disease presentation [9]. Plain radiography yields high diagnostic accuracy and is considered the imaging modality of choice [10]. Despite the fact that CT and MRI add little to the diagnosis, they can be helpful in excluding other entities that can mimic a simple bone cyst [5,11]. Moreover, magnetic resonance imaging (MRI) can be combined with plain radiography to confirm the presence of fluid within a cyst and demonstrate its aggressive features [5]. Hitherto, various methods have been proposed to manage UBCs, including observation, intralesional steroid injection, percutaneous or open curettage with or without bone grafting, percutaneous injection of allogenic demineralized bone matrix and cannulated pin/screw insertion [12-19]. However, minimally invasive techniques are far more desirable due to the higher healing rate, a lack of recurrence and the preservation of the periosteum, muscles, blood supply and shorter recovery time.
In this case presentation, we discuss the successful management of a calcaneal UBC with a new minimally invasive technique utilizing 2 interosseous needles with the injection of cement into the cyst without aspiration.
Case Presentation
A 16- year old girl presented with chief complaints of pain and swelling over the right hind foot and calcaneal region and difficulty bearing weight over a period of 8 days. She had suffered from mild pain in the right calcaneus intermittently since the age of 3, which had been relieved with rest and cold compression, but approximately 3 weeks prior to her coming to our center, the pain had become constant. The pain had increased over an 8-day period during which the patient had been playing volleyball most of the day. She did not report a history of trauma to the calcaneal region and there was no family history of other pathological conditions.
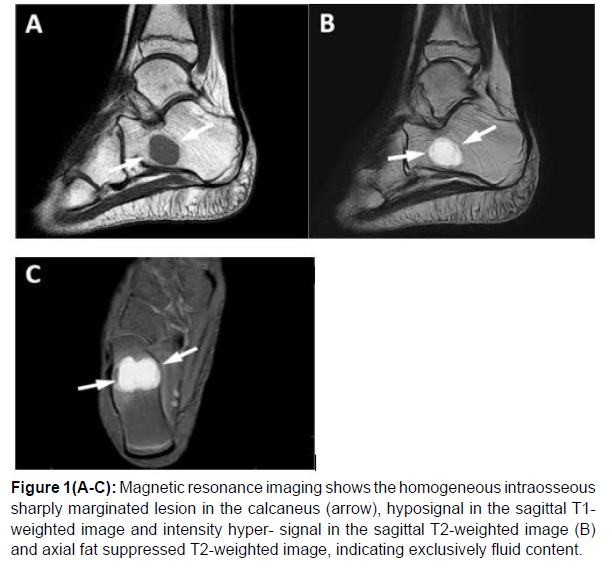
On physical examination, the patient appeared relatively healthy and well nourished. She did not suffer from any other medical conditions and took no medications. On local examination, tenderness over the right calcaneal region was the only noteworthy sign; there was no muscle atrophy and the limbs appeared symmetric with full active and passive range of motion. There was no right ankle edema and initial plane radiographs of the right ankle and foot showed a well-demarcated cystic lesion without fractures, new bone formation, cortical disruption, scalloping or periosteal reaction in the right calcaneus. Contralateral radiographs from the left ankle and foot were also taken and no abnormalities were observed. An MRI of the right ankle and foot demonstrated a homogeneous low T1 signal and a hyperintense T2 signal, suggestive of a simple bone cyst, which measured approximately 18.2 x 21.5 x 14 mm (L x W x H), with an estimated volume of 2.86 ml , in the anterior process of the calcaneus (Figure 1).
Figure 1(A-C): Magnetic resonance imaging shows the homogeneous intraosseous
sharply marginated lesion in the calcaneus (arrow), hyposignal in the sagittal T1-
weighted image and intensity hyper- signal in the sagittal T2-weighted image (B)
and axial fat suppressed T2-weighted image, indicating exclusively fluid content.
Laboratory evaluation consisting of a complete blood count, erythrocyte sedimentation rate (ESR) levels of calcium, phosphate and serum albumin, renal function tests (blood urea nitrogen [BUN] creatinine), urinalysis, coagulation tests (partial thromboplastin time [PTT], prothrombin time [PT] and international normalized ratio [INR]) were analysed and the results were all within normal limits.
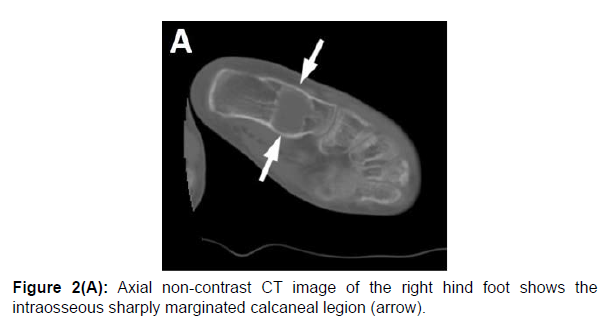
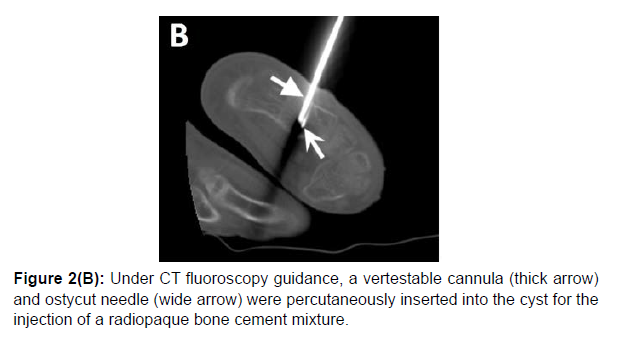
Based on the clinical and radiological findings, a simple bone cyst was diagnosed and radiological intervention was planned for the patient. Written informed consent was obtained from the patient and her family prior to the procedure (Figure 2A). During the intervention, the patient was administered local anesthetics (5 CC of lidocaine 2%) and was consciously sedated (1 mg midazolam, 1 mg/kg ketamin and 1mg/kg propofol as maintenance). Initially, a VerteStable cannula was percutaneously inserted into the cyst under the guidance of CT fluoroscopy to inject cement and an Ostycut needle (16G) × 100 mm (Angiomed/Bard, Karlsruhe, Germany) was also inserted percutaneously to allow the efflux of serosanguineous fluid from the cyst (Figure 2B).
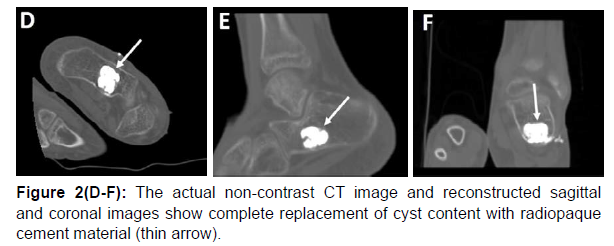
Unlike previous techniques, aspiration was only performed to reveal serosanguineous fluid content. Subsequently, through a VerteStable cannula, the radiopaque bone cement mixture (BonOs Inject 1×24, OSARTIS GmbH, Munster, Germany) was injected into the cyst. The injection from one needle was immediately associated with the efflux of serosanguineous fluid from the Ostycut needle. Cement injection was continued until there was no more serosanguineous fluid efflux from the second needle and only cement efflux was witnessed (Figure 2C). The procedure was performed under fluoroscopy control to warrant complete replacement of cyst content with cement material (Figure 2D-F). The system was kept closed to prevent air embolism. Having completely filled the cyst, the needles were removed and a dressing was placed over the injection sites. The duration of the procedure was estimated to be 15 minutes and the total dose length product (DLP) and smartview DLP were 577.9 mGy*cm and 13 mGy*cm, respectively. After the procedure, the patient's hemodynamic status was stable and she was discharged the next day. No weight-bearing was recommended for 1-month postoperatively and full weight-bearing without support was initiated one month after the procedure. The response to intervention was assessed by the relief of symptoms. The patient experienced itching and warmth at the site of the procedure immediately after the intervention. 3 weeks after the procedure, the injection site healed smoothly and the patient reported pain with weight bearing activities and limping after prolonged standing. On patient follow- ups conducted approximately 6 months and one year after the procedure, there were no reports of itching or warmth at the site of the procedure and no complaints of limping. The patient had experienced a few scattered episodes of mild pain after prolonged standing, which had been relieved with rest.
Discussion
Unicameral bone cysts (UBCs) are non-neoplastic fluid-filled cavities that account for up to 3% of primary bone lesions and solely arise in children and adolescents [2, 6, 7, 10]. Although the exact cause of the formation of these lesions has not been elucidated, many theories have been proposed, such as local disruption in bone formation, small trapped nests of synovial cells in bones and blockage in the venous drainage [4, 5, 20]. Based on observations that have shown a slight increase in the internal pressure of the involved bone compared to the normal pressure of the bone marrow and a lower partial pressure of oxygen in the cyst fluid compared to arterial or venous blood, the most widely accepted theory is a blockage in venous drainage [20]. UBCs are mainly diagnosed by clinical presentations and plain radiography, which is the imaging modality of choice and possesses high diagnostic accuracy [6]. Despite the fact that both CT and MRI add little to the diagnosis, these modalities can be helpful with regards to eliminating other entities that can mimic a simple bone cyst [1, 11]. UBCs of the calcaneus mostly affect the anterolateral aspect of the bone, which is far away from the area where most body weight is transmitted [8].
A variety of strategies ranging from non-operative management, intralesional steroid injection, percutaneous or open curettage with or without bone grafting, percutaneous injection of allogenic demineralized bone matrix to more invasive procedures, such as cannulated pin/ screw insertion and surgical procedures have demonstrated acceptable efficacy. However, the optimal management of these lesions remains an issue of debate. In patients who are incidentally diagnosed and have no risk of pathological bone fractures, non-operative management with close follow-up is recommended. Spontaneous resolution of heel pain has been reported in 1 to 2% of patients managed non-operatively [4, 19].
Intralesional steroid injection was first introduced as a successful management strategy for simple bone cysts. Despite the reported outcomes, recent studies on calcaneal UBCs have demonstrated a high recurrence rate even after multiple steroid injections [13, 21]. Scaglietti et al reported only 24% cyst healing after a single injection and incomplete healing even after multiple injections. Glaser et al performed 9 steroid injections on 6 patients and curettage combined with bone grafting on 9 patients [22]. All of their patients were asymptomatic and the study reported a 0 healing rate with persistent cysts in 2 of the cases injected which steroids and complete healing without recurrence in cases who underwent curettage with bone grafting after a minimum follow-up period of 12 months. Moreover, a few studies have suggested that the steroids have minimal effect with regards to resolving the cyst, and that the mechanical effect of punctures, which helps normalise local circulation, is the key factor.
Percutaneous or open curettage, which can be performed with or without bone grafting, is the traditional method for the management of symptomatic calcaneal UBCs. Although open curettage with bone grafting has demonstrated significant improvement in the resolution of heel pain, it has been associated with a high recurrence rate in cases where the graft had been incompletely packed [16]. Innami et al performed endoscopic curettage in conjunction with percutaneous injection of calcium phosphate to treat symptomatic calcaneal UBCs [12]. Their findings showed the complete resolution of pain and radiological healing in all patients after a follow-up period of 3 years. Aiba et al performed endoscopic curettage on 6 calcaneal UBCs and reported complete healing after a mean follow-up period of 4 months without cyst residue [14].
Abdel-Wanis et al used minimal curettage, multiple drilling and continuous decompression as an alternative to auto grafting in children [18]. Due to the patients’ young age, harvesting a large volume of autographs can be difficult. On the other hand, the risk of disease transmission by autografting should not be overlooked, no matter how small. This study reported complete radiographic healing in all patients and total pain relief without recurrence in 59% of cases. Other methods, such as a cannulated screw placed for continuous decompression, have demonstrated lower recurrence rates, higher rates of healing and a significant reduction in heel pain following decompression. Saraph V et al treated 9 calcaneal UBCs with continuous decompression using cannulated screws, among whom 8 cases showed complete healing and one showed a residual region on imaging with complete pain relief after a minimum follow-up period of 24 months [22]. The only complication reported in the study was irritation at the screw insertion site observed in one patient, which led to early removal of the screw. Shirai et al managed 23 simple bone cysts in the calcaneus by using cannulated hydroxyapatite (HA) pins, which were used to achieve continuous decompression [24]. After a mean follow-up period of 5 months, their results showed complete healing in all patients. In another study, Park et al compared open chip allogenic bone grafting with percutaneous injection of bone powder [15]. Complete healing was reported in 70% of open chip allogenic bone grafts and 50% of cases percutaneously injected with bone powder after a mean follow-up up of 49.4 months. Persistent cysts were reported in 15% of cases treated using open chip allogenic bone grafts and 20% of those managed by percutaneous injection of bone powder.
In this case presentation, we treated a simple bone cyst in the calcaneus with a novel technique by inserting two needles into the cyst without aspiration, and injecting cement until the cyst was completely filled. Utilizing two needles enabled us to fully drain the cysts with a radiopaque bone cement mixture in a relatively short period of time (15 minutes) without any complications.
The authors believe this novel technique has the potential to be used as a feasible minimally invasive approach to manage symptomatic simple bone cysts in the calcaneus. Nevertheless, further studies are required to validate its long-term safety and efficacy with regards to the management of symptomatic calcaneal simple bone cysts.
References
- Kadhim M, Thacker M, Kadhim A, Holmes L, Jr. (2014) Treatment of Unicameral Bone Cyst: Systematic Review and Meta Analysis. J Child Ortho 8:171-191.
- Rosenblatt J, Koder A. (2019) Understanding Unicameral and Aneurysmal Bone Cysts. Pediatr Rev 40:51-59.
- Subramanian S, Kemp AK, Viswanathan VK. Bone Cyst. StatPearls. Treasure Island (FL)
- Komiya S, Inoue A. (2000) Development of a Solitary Bone Cyst–A Report of a Case Suggesting Its Pathogenesis. Arch Orthop Trauma Surg 120:455-457.
- Abdel-Wanis ME, Tsuchiya H. (2002) Simple Bone Cyst is Not a Single Entity: Point Of View Based on a Literature Review. Medical hypotheses 58:87-91.
- Mascard E, Gomez-Brouchet A, Lambot K. (2015) Bone Cysts: Unicameral and Aneurysmal Bone Cyst. Ortho Traumatol Surg Res 101:S119-S127.
- Pretell-Mazzini J, Murphy RF, Kushare I, Dormans JP. (2014) Unicameral Bone Cysts: General Characteristics and Management Controversies. J Am Acad Ortho Surg 22:295-303.
- Levy DM, Gross CE, Garras DN. (2015) Treatment of Unicameral Bone Cysts of the Calcaneus: A Systematic Review. J Foot Ankle Surg 54:652-656.
- Donaldson S, Wright JG. (2015) Simple Bone Cysts: Better With Age? J Pediatr Ortho 35:108-114.
- Noordin S, Allana S, Umer M, Jamil M, Hilal K et al. (2018) Unicameral Bone Cysts: Current Concepts. Ann Med Surg (Lond) 34:43-49.
- Wootton-Gorges SL. (2009) MR Imaging Of Primary Bone Tumors and Tumor-Like Conditions in Children. Magn Reson Imaging Clin N Am 17:469-487.
- Innami K, Takao M, Miyamoto W, Abe S, Nishi H et al. (2011) Endoscopic Surgery for Young Athletes With Symptomatic Unicameral Bone Cyst of The Calcaneus. Am J Sports Med 39:575-581.
- Rougraff BT, Kling TJ. (2002) Treatment of Active Unicameral Bone Cysts With Percutaneous Injection of Demineralized Bone Matrix and Autogenous Bone Marrow. J Bone Joint Surg Am 84:921-929.
- Aiba H, Kobayashi M, Waguri-Nagaya Y, Goto H, Mizutani J et al. (2018) Treatment of Simple Bone Cysts Using Endoscopic Curettage: A Case Series Analysis. J Ortho Surg Res 13:168.
- Park IH, Micic ID, Jeon IH. (2008) A Study Of 23 Unicameral Bone Cysts of The Calcaneus: Open Chip Allogeneic Bone Graft Versus Percutaneous Injection of Bone Powder With Autogenous Bone Marrow. Foot Ankle Int 29:164-170.
- Spence KF, Jr., Bright RW, Fitzgerald SP, Sell KW. (1976) Solitary Unicameral Bone Cyst: Treatment With Freeze-Dried Crushed Cortical-Bone Allograft. A Review of One Hundred and Forty-Four Cases. J Bone Joint Surg Am 58:636-641.
- Hashemi-Nejad A, Cole WG. (1997) Incomplete Healing of Simple Bone Cysts After Steroid Injections. J Bone Joint Surg Br 79:727-730.
- Abdel-Wanis ME, Tsuchiya H, Uehara K, Tomita K. (2002) Minimal Curettage, Multiple Drilling, and Continuous Decompression Through A Cannulated Screw for Treatment of Calcaneal Simple Bone Cysts in Children. J Pediatr Ortho 22:540-543.
- Polat O, Sağlik Y, Adigüzel HE, Arikan M, Yildiz HY. (2009) Our Clinical Experience on Calcaneal Bone Cysts: 36 Cysts in 33 Patients. Arch Ortho Trauma Surg 129:1489-494.
- Chigira M, Maehara S, Arita S, Udagawa E. (1983) The Aetiology and Treatment of Simple Bone Cysts. J Bone Joint Surg Br 65:633-637.
- Chang CH, Stanton RP, Glutting J. (2002) Unicameral Bone Cysts Treated by Injection of Bone Marrow or Methylprednisolone. J Bone Joint Surg Br 84:407-412.
- Glaser DL, Dormans JP, Stanton RP, Davidson RS. (1999) Surgical Management of Calcaneal Unicameral Bone Cysts. Clin Ortho Relat Res 360:231-237.
- Saraph V, Zwick EB, Maizen C, Schneider F, Linhart WE. (2004) Treatment of Unicameral Calcaneal Bone Cysts in Children: Review of Literature and Results Using a Cannulated Screw for Continuous Decompression of The Cyst. J Pediatr Ortho 24:568-573.
- Shirai T, Tsuchiya H, Terauchi R, Tsuchida S, Mizoshiri N et al. (2015) Treatment of a Simple Bone Cyst Using a Cannulated Hydroxyapatite Pin. Medicine (Baltimore) 94:e1027.
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Citation: Hossein G, Arezou HZ, Alireza A (2022) Successful Treatment of a Symptomatic Unicameral Calcaneus Bone Cyst by Cement Injection Using a Double Needle Technique under CT Guidance: A Case Report. Clin Res Foot Ankle, 10: 327. DOI: 10.4172/2329-910X.1000327
Copyright: © 2022 Hossein G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4694
- [From(publication date): 0-2022 - Dec 07, 2025]
- Breakdown by view type
- HTML page views: 3970
- PDF downloads: 724