Case Report Open Access
Successful Outcome in a Rare Case of Large Adrenal Myelolipoma during Pregnancy Complicated by Uterine Inversion
Manu Goyal*, Alka Kriplani, Reeta Mahey and Garima KachhawaDepartment of Obstetrics and Gynaecology, All India Institute of Medical Sciences, New Delhi, India
- *Corresponding Author:
- Manu Goyal
Department of Obstetrics and Gynaecology
All India Institute of Medical Sciences
New Delhi, India
Tel: 91-9971833603
E-mail: drmanu_8@yahoo.co.in
Received date: August 31, 2016; Accepted date: October 28, 2016; Published date: October 31, 2016
Citation: Goyal M, Kriplani A, Mahey R, Kachhawa G (2016) Successful Outcome in a Rare Case of Large Adrenal Myelolipoma during Pregnancy Complicated by Uterine Inversion. J Preg Child Health 3:293. doi:10.4172/2376-127X.1000293
Copyright: © 2016 Goyal M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Pregnancy and Child Health
Abstract
Primary adrenal tumours are often functioning, and include adrenal cortical adenomas or phaeochromocytomas. With advances in imaging, uncommon tumours are more frequently reported. These are myelolipoma, lipoma, teratoma, angiomyolipoma and liposarcoma. Adrenal myelolipoma are rare tumors with few cases reported during pregnancy.
Keywords
Pregnancy; Myelolipoma; Inversion; Adrenal
Introduction
Primary adrenal tumours are often functioning and include adrenal cortical adenomas or phaeochromocytomas. With advances in imaging, uncommon tumours are more frequently reported. These are myelolipoma, lipoma, teratoma, angiomyolipoma and liposarcoma [1]. Adrenal myelolipoma are rare tumours with few cases reported during pregnancy.
We present a case of pregnancy with large adrenal myelolipoma and its successful management.
Case Summary
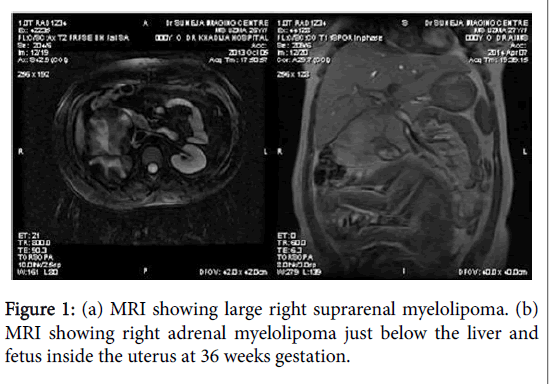
A 26 year old G2P1L1 presented to Gynaecology OPD at 20 weeks with large suprarenal mass on ultrasound. The maternal condition was stable, examination was normal, with pulse rate of 84 bpm, blood pressure of 124/76 mm Hg. Ultrasonography showed right suprarenal mass of 9 × 8 × 6.5 cm replacing adrenal gland, suggestive of myelolipoma. Fetus was normal and placenta was fundo-posterior. Urology opinion was sought and MRI revealed fat containing suprarenal mass of 9 × 6.5 × 5.5 cm consistent with right adrenal myelolipoma (Figure 1a). All investigations including hemogram, kidney and liver function tests, serum cortisol, 17- hydroxyprogesterone acetate, metanephrines, urinary vanillylmandelic acid, adrenaline, noradrenaline were normal. Repeat MRI at 36 weeks showed a well-defined encapsulated altered signal lesion measuring 11 × 6.5 × 7.5 cm in suprarenal region without visualisation of normal right adrenal gland and no calcification/hemorrhage (Figure 1b). Lesion was indenting inferior surface of liver and superior pole of right kidney with displacement of head of pancreas.
The patient delivered 3.3 kg male baby at 40 weeks by low forceps. Placenta was delivered completely by controlled cord traction without any signs of morbid adherence. Suddenly, uterus was seen protruding into the vagina up to introitus. Per abdominally, uterus was not palpable and patient had severe pain. It was second degree uterine inversion. Uterus was stopped from coming out further by putting right fist into vagina. Uterotonics were stopped, bladder catheterised, patient shifted immediately to operation theatre and general anaesthesia was administered. The uterus was relaxed, manual reposition was done using right hand by pushing the margins of uterus upwards slowly until whole fundus got reposited; hand was kept inside the uterus for few minutes after starting oxytocics and ergometrine to prevent re-inversion. There was blood loss of 1200 ml and 3 units packed red cell were transfused. Broad spectrum antibiotics were given for five days. Patient was discharged in stable condition on day 7. The adrenal mass was same in size on MRI after 2 months of delivery and patient is asymptomatic so it has not been planned for surgery.
Discussion
Myelolipoma has been reported in 0.08-0.4% of the diagnosed adrenal tumors [1]. It occurs in 40-60 years age with equal sex distribution. They are benign, non-functioning, asymptomatic neoplasms composed of adipocytes and hematopoietic tissue [2]. Large tumors present as pain or acute abdomen due to rupture or hemorrhage [3]. Diagnosis is made on CT or MRI which delineate the features of fat containing encapsulated extrarenal mass as in our case. MRI is the investigation of choice due to high sensitivity and no radiation hazards. Differential diagnosis includes adrenal adenomas, phaeochromocytoma.
Our patient was pregnant and asymptomatic, so biopsy was not done. Studies have recommended surgical removal of adrenal myelolipoma larger than 5 cm because of rupture or hemorrhage [4]. Surgery during pregnancy has risk of abortion, placental separation, preterm labour, prematurity, anaesthesia risks and fetal demise. Our patient presented with tumor at 20 weeks without symptoms so we planned to avoid adrenalectomy. Our patient had postpartum uterine inversion which is very rare. The incidence varies from 1:2150 to 1:6500 [5]. Puerperal uterine inversion is due to displacement of uterine fundus during third stage of labour. It is classified as complete if fundus passes through cervix or incomplete if it remains above this level. The most likely cause is strong traction on umbilical cord, particularly when the placenta is in fundal location. Other factors include fundal pressure, relaxed uterus, lower segment and cervix; placenta accreta, particularly involving the fundus, short umbilical cord, congenital weakness or anomalies of uterus, and antepartum use of magnesium sulfate or oxytocin [6]. In our case, there was no placenta accreta, fundal pressure or short cord. Management of uterine inversion has two components: treatment of haemorrhagic shock and replacement of the uterus. Resuscitation should start immediately while attempts are made to replace uterus manually with success rate of 22-43% [7-9]. The uterus can be reposited by use of hydrostatic pressure (a litre bag of warm crystalloid attached to silicone vacuum suction cap held firmly in vagina). If the uterus remains inverted, contraction of the cervix may require relaxation by general anaesthesia or tocolytics. Severe cases require laparotomy. The inversion was successfully managed in our case by manual reposition of uterus and pregnancy outcome was good for both mother and the fetus.
To conclude, adrenal myeolipoma can be managed conservatively during pregnancy if asymptomatic and surgery can be delayed with interval imaging. These cases should be referred to tertiary centre for multidisciplinary approach.
References
- Abouleski E, Ali V, Joumaa B, Lopez M, Gupta D (1995) Anaesthetic management of acute puerperal uterine inversion. British Journal of Anaesthesia75: 486-487.
- Brar HS, Greenspoon JS, Platt LD, Paul RH (1989) Acute puerperal uterine inversion. New approaches to management. Journal of Reproductive Medicine 34: 173-177.
- Doddi S,Singhal T, Leake T, Sinha P (2009) Management of an incidentally found large adrenal myelolipoma: A case report. Cases Journal 2: 8414.
- Geelhoed GW, Druy EM (1982) Management of the adrenal ��?incidentaloma�. Surgery 92: 866-874.
- Han M, BurnettAL, Fishman EK, Marshall FF (1997) The natural history and treatment of adrenal myelolipoma. Journal of Urology 157: 1213-1216.
- Hisamatsu H, Sakai H, Tsuda S, Shigematsu K, Kanetake H (2004) Combined adrenal adeonoma and myelolipoma in a patient with Cushings syndrome: Case report and review of the literature. International Journal of Urology 11: 416-418.
- Lam KY, Lo CY (2001) Adrenal lipomatous tumors: A 30 year clinicopathological experience at a single institution. Journal of Clinical Pathology 54: 707-712.
- Kenney P, Wagner B, Rao P, Heffess C (1998) Myelolipoma CT and pathologic features. Radiology 208: 87-95.
- Zahn CM, Yeomans ER (1990) Postpartum hemorrhage: Placenta accreta, uterine inversion and puerperal hematomas. Clinical Obstetrics Gynecology 33: 422-431.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 10857
- [From(publication date):
October-2016 - Dec 15, 2024] - Breakdown by view type
- HTML page views : 10187
- PDF downloads : 670