Successful Kidney transplantation after recovery from COVID -19
Received: 04-Jan-2021 / Accepted Date: 15-Mar-2021 / Published Date: 28-Mar-2021 DOI: 10.4172/2475-7640.1000132
Abstract
This case describes successful renal transplantation in an elderly patient following diagnosis with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pneumonia. Forty-six days prior to transplant, a 65-year-old African American Male with end stage renal disease on kidney transplant waitlist, hypertension, hyperlipidemia, and chronic diastolic heart failure presented to the emergency department and was diagnosed with SARS-CoV-2 pneumonia. Following treatment with dexamethasone and convalescent plasma therapy during the two-week inpatient admission, the patient was discharged home. Subsequently, the patient was reactivated on waitlist following two confirmatory negative SARS-CoV-2 PCR tests. Upon the transplant admission, repeat PCR and rapid antigen tests resulted negative. The patient received anti-thymocyte globulin 4.5 mg/kg as induction therapy. Post-operative course was uneventful with immediate graft function. Maintenance therapy included tacrolimus, mycophenolate, and corticosteroid taper. A SARS-CoV-2 IgG antibody test collected during the admission resulted positive. The patient was discharged on post-operative day 4 with a serum creatinine of 1.6 mg/dL. At 2 month following transplant, the patient remains asymptomatic with stable renal function. In this case report, the patient safely received T-cell depleting induction therapy following SAR-CoV-2 pneumonia. Positive SARS-CoV-2 antibodies at the time of transplant may have provided protection against recurrent infection.
Keywords: Kidney transplantation; Serum creatinine; Antibiotics; lymphopenia; Tacrolimus
Abbreviations
AKI: Acute Kidney Injury; ARDS: Acute Respiratory Distress Syndrome; ALT: Alanine Aminotransferase; AST: Aspartate Aminotransferase; AZM: Azithromycin; BNP: B-type Natriuretic Peptide; COVID-19: Coronavirus Disease 2019; CRO: Ceftriaxone; CRP: C-Reactive Protein; CT: Computed Tomography; CVA: Cerebrovascular Accident; CXR: Chest X-ray; IVMP: IV Methylprednisolone; NC: Nasal Cannula; PCR: Polymerase Chain Reaction; SARS - CoV-2: Severe Acute Respiratory Syndrome Coronavirus 2; SCr: Serum Creatinine; WBC: White Blood Cell Count
Introduction
Since the first reported case of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (COVID-19) in December 2019 in Wuhan, China, this pandemic has claimed more than 1,000,000 lives worldwide to date and infected more than 27,900,000 people around the globe.
The pandemic has had great implications on the transplant community. The rising toll of deaths and immediate need to access hospitals by infected patients or those with suspected infection had to alter our resource allocation and hospital priorities. This resulted in a decrease in total transplants, deceased and living donors, until the emergence of better public health measures, availability diagnostics and encouraging therapeutics [1-3].
There have been reported sequela to SARS-CoV-2 infection including hypercoagulability, cardiac myopathy, arrhythmias and postop pulmonary fibrosis and with reported cases of recurrent infection there is no clear consensus on what is an adequate disease free time prior to transplantation and if modification to usual induction and maintenance immunosuppressive therapies are warranted [4-6].
We report here a case of successful kidney transplantation in a patient 46 days after diagnosis with COVID-19.
Case Report
65 year old African American gentleman, with end-stage renal disease secondary to hypertension, who has been on our kidney transplant waitlist, presented to emergency department with progressive shortness of breath symptoms for 2 days. This patient had history of exposure to a COVID 19 positive patient, his father who is 82 years old, only a couple days prior. He also reported low grade fever, chest pain, fatigue and lethargy. His past medical history was also notable for hyperlipidemia, chronic diastolic heart failure, hemorrhagic CVA in 2012 with no residual weakness, depression and mild dementia. Upon arrival patient was febrile 39.2°C, oxygen saturation were 98% on 2L of nasal cannulas, heart rate 112 bpm but normotensive. Patient looked dyspneic despite saturating well on nasal cannula (NC). He was non-cyanotic, had bibasilar rales and no pitting edema.
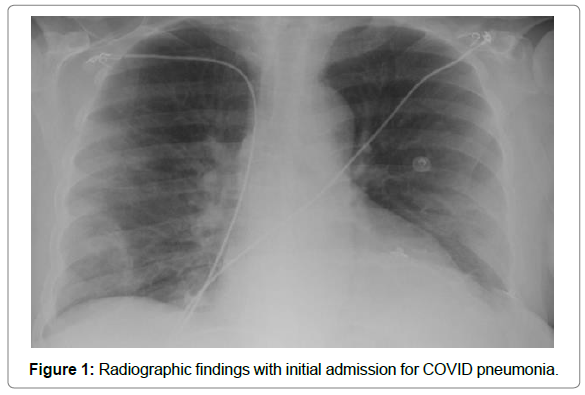
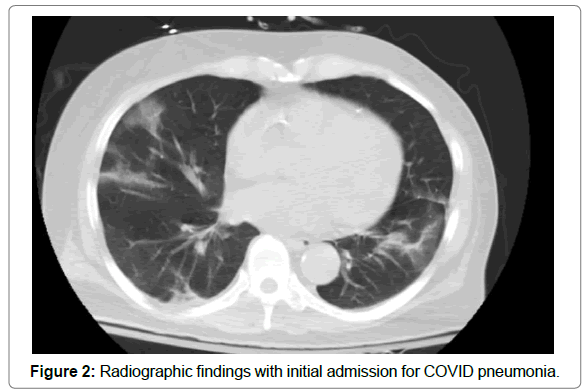
Initial laboratory testing WBC was 5.0 K/mm3, Hb 8.3 g/ dL, Platelet count was 165 k/mm3. Lactate 0.8 units/L, pro B type natriuretic peptide (BNP) 360 pg/ml (normal 5.0-100.0 pg/ml) and positive nasopharyngeal swab SARS-CoV-2 PCR. Patient was admitted to COVID unit, pan-cultured, started empirically on piperacillin/ tazobactam and azithromycin, and heparin subcutaneously for venous thromboembolism prophylaxis. Chest X-ray (CXR) revealed a right mid-lower lung haziness concerning for infiltrate (Figure 1), a CT of his chest revealed ground glass opacities with linear margins were compatible with a COVID-19 pneumonia (Figure 2). Patient was started on a 10-day course of dexamethasone. He received convalescent plasma as his oxygen requirements deteriorated by second day of admission to 94% on 4L NC. Given patient’s end stage renal disease he was not considered a candidate for remdesivir. During course patient had episodes of non-sustained ventricular tachycardia, but transthoracic echocardiogram showed normal ejection fraction of 55% with no other structural concerns. Troponin was <0.04 ng/ml 12 hours apart. His oxygen requirement did not exceed 4L on NC. Patient continued to improve. He was tested within 1 week of treatment and was still positive for SARS-CoV-2 PCR. He was discharged home on day 14 of admission without any oxygen requirement and a first negative COVID 19 PCR test.
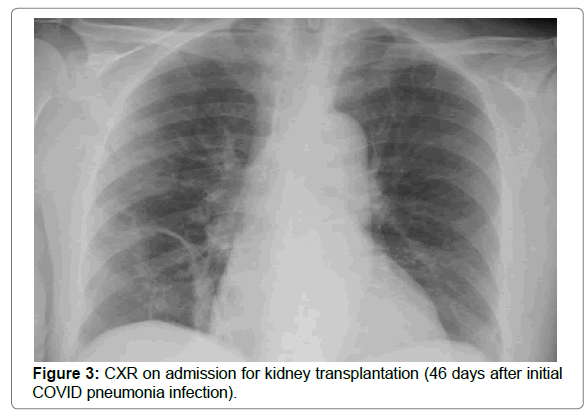
Forty-six days later patient was admitted for a potential kidney transplant. Patient had in the interim an uneventful recovery and was reactivated on kidney transplant waitlist after a second negative COVID 19 negative PCR. On admission his vitals were within normal limits, he had a rapid SARS-CoV-2 antigen test and a SARS-CoV-2 PCR. His admission CXR although had no definite process, showed similar scarring/ atelectasis in the right lower lung field (Figure 3). The patient was a B blood group patient with 0 panel reactive antibodies (PRA) and anti A blood group antibody titers of 1:2. The donor was a 30 year old brain dead female donor with A2 blood group, 40% kidney profile donor index and had a terminal creatinine was 1.4 mg/dL. The kidney was transplanted at 15 hours of cold ischemic time, the right kidney was used, it had 2 arteries, 1 vein and 1 ureter anatomy. The operative course was uneventful. Patient received 1.5 mg/kg of thymoglobulin for induction and 500 mg of methyl prednisone intraoperatively. The kidney was functional immediately with a 150-300ml/hr of urine output and a declining serum creatinine. The patient postoperative course was uneventful he completed over the following 2 days a total of 4.5 mg/ kg of thymoglobulin in divided doses. He was started immediately on LCP-tacrolimus and mycophenolate sodium on day 0 postop. He received a taper of steroids 250 mg, 125 mg, 60 mg and then 20 mg over the following 4 days. Patient bowel function returned by postop day 2. Post-operative A2 antibody titers on day 3 and day 5 remained at 1:4. Patient had therapeutic tacrolimus levels by postoperative day 5. Patient did not suffer from any respiratory symptoms, his incentive spirometer effort on the day of discharge were 4000 mls. The patient was discharged on Postop Day 4.
Discussion
In this case report, we described a successful outcome of an elderly renal transplant following recent SARS-CoV-2 induced pneumonia. In the United States, despite similar mortality between solid-organ transplant and non-solid organ transplant patients with SARS-CoV-2 (Molnar et al) the pandemic has tremendously impacted operational logistics and clinical decision making for new transplants. For many programs, transplant activities have been disrupted. As hospitals resume transplanting activities, the risk of SARS-CoV-2 infection post-operative remains unknown. Furthermore, among wait-list patients who have contracted SARS-CoV-2, little is known regarding the appropriate time to relist and post-transplant immunosuppression approach [7,8].
Currently, the American Society of Transplant recommends that a COVID-infected waitlist candidate should not be reactivated until the PCR is negative. In deceased donor transplants, polymerase chain reaction (PCR) testing for SARS-CoV-2 virus immediately (within 12 hours) prior to organ transplantation should be performed. Living donor candidates are suggested to have a negative PCR test 7 to 14 days prior to surgery followed by self-isolation for 7-14 days. Temperature check and chest x-ray on the day of surgery are also recommended . Patients with positive results regardless of presence or absence of symptoms should not undergo transplant surgery. Lei S et al. showed that asymptomatic patients with positive PCR had increased morbidity and mortality after proceeding with general surgery. Although patients with anti-COVID antibodies who are PCR negative are thought as being relatively immune to subsequent infection, further empirical evidence is needed to confirm this. In our case report the patient had two negative PCR tests prior to relisting them. He also had anti-COVID-19 IgG antibodies at the time of transplant which may be reflective of acquired immunity as he remained COVID-19 negative 2 months later after standard induction and maintenance immunosuppression. However, it is still unclear the duration of protection, and the impact of future vaccinations.
Severe COVID infections are associated lymphopenia and extreme pro-inflammatory response. Although the Montefiore experience suggests increased risk of COVID infection with T-cell depleting agents for induction i.e. thymoglobulin, inadequate induction therapy increases risk of acute rejection. Subsequent therapies for rejection treatment and enhanced maintenance immunosuppression may ultimately enhance the overall risk of contracting infections. For this reason, our center chooses to continue anti-thymocyte globulin for renal transplant induction. Whereas our pre-COVID era protocol called for 6.0 mg/kg total of thymoglobulin among African American recipients, a lesser dose was given to the patient in this case. Given the pandemic, advanced age, otherwise low immunologic risk as demonstrated by negative cPRA and donor specific antibodies, and therapeutic calcineurin inhibitor level achieved within the first week, we believed a total thymoglobulin dose of 4.5 mg/kg was sufficient to prevent acute rejection while balancing infectious risks.
This is a 2 month follow up of a 65 years old gentleman who was infected with mild COVID pneumonia managed with dexamethasone, antibiotics and convalescent plasma, who had a successful kidney transplant within 2 months of their infection. The patient received full dose 4.5 mg/kg of thymoglobulin induction and tacrolimus, myfortic and prednisone maintenance. The patient had IgG positive COVID-19 antibodies at the time of transplant, which may confirm immunity. The patient remains healthy with excellent renal function and without infectious complications.
Conflicts of Interest
The authors of this manuscript have no conflicts of interest to disclose.
References
- Rodrigo E, Minambres E, Gutierrez-Banos JL, Valero R, Belmar L, et al. (2020). COVID-19-related collapse of transplantation systems: A heterogeneous recovery? Am J Transplant.
- Miklos Z Molnar, Anshul Bhalla, Ambreen Azhar, Makoto Tsujita, Manish Talwar, et al. (2020) Outcomes of critically ill solid organ transplant patients with COVIDâ€19 in the United States. Am J Transplant 00:1-11.
- https://asts.org/advocacy/covid-19-resources/asts-covid-19-strike-force/reengaging-organ-transplantation-in-the-covid-19-era#
- Shaoqing Lei, Fang Jiang, Wating Su, Chang Chen, Jing li Chen, et al. (2020) Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. The Lancet 21:100331.
- Huang I, Pranata R (2020) Lymphopenia in severe coronavirus disease-2019 (COVID-19): systematic review and meta-analysis. J Intensive Care 8: 36.
- Zeng F, Huang Y, Guo Y (2020) Association of inflammatory markers with the severity of COVID-19: A meta-analysis. Int J Infect Dis 96: 467-474.
- EnverAkalin, YorgAzzi, Rachel Bartash, Harish Seethamraju, Michael Parides, et al. (2020) COVID-19 and Kidney transplantation. N Engl J Med 24: NEJMc2011117.
Citation: Reyad AI, Dao A, Guiteau JJ, Madhrira MM, Allam SR (2021) Successful Kidney transplantation after recovery from COVID -19. J Clin Exp Transplant. 6: 132. DOI: 10.4172/2475-7640.1000132
Copyright: © 2021 Reyad AI, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2915
- [From(publication date): 0-2021 - Apr 18, 2025]
- Breakdown by view type
- HTML page views: 2181
- PDF downloads: 734