Research Article Open Access
Studying Cost as a Factor in the Choice between Quality and Quantity of Life amongst Patients with Cancer and their Caregivers at a Cancer Centre in Singapore
Keson Tay1, Lee Jiayu Rachel1, Sim Shin Wei Dorsett2, Sumytra Menon3, Ravindran Kanesvaran4,5, Rukshini Puvanendran5,6 and Lalit Kumar Radha Krishna5,7*1Yong Loo Lin School of Medicine, National University of Singapore, Singapore
2Singhealth Residency, Singapore
3Lien Centre for Palliative Care, Duke-NUS, Singapore
4Division of Medical Oncology, National Cancer Centre Singapore, Singapore
5Tutor Practice Course 2, Duke-NUS, Singapore
6KK Womens and Children’s Hospital, Singapore
7Division of Palliative Medicine, National Cancer Centre Singapore, Singapore
- *Corresponding Author:
- Lalit Kumar Radha Krishna
Senior Consultant in Palliative Care, National Cancer Centre Singapore, Singapore
Tel: +65 64368000
E-mail: Lalit.krishna@nccs.com.sg
Received date: April 29, 2016; Accepted date: July 18, 2016; Published date: July 22, 2016
Citation: Tay K, Rachel LJ, Dorsett SSW, Menon S, Kanesvaran R, et al. (2016) Studying Cost as a Factor in the Choice between Quality and Quantity of Life amongst Patients with Cancer and their Caregivers at a Cancer Centre in Singapore. J Palliat Care Med 6:276. doi: 10.4172/2165-7386.1000276
Copyright: © 2016 Tay K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Background: Treatment costs and sociocultural concerns play a significant role in decisions regarding Quantity of Life (QuoL) options that seek to prolong life, such as chemotherapy, or a Quality of Life (QoL) approach where the patient refuses available treatments such as chemotherapy in favour of maximizing comfort and quality of life at the end of life in Singapore. Deciphering the reasons behind such care decisions is often difficult because of local social taboos regarding discussions about death and dying. Objectives: To scrutinize the rationale behind QuoL and QoL within the Singapore context and delineate the impact of cost upon such decisions. Methods: To overcome local sociocultural taboos about discussing death and dying with patients, participants watched a video vignette of a family discussing treatment options for their mother (Mrs Tan) who was recently diagnosed with terminal cancer. Participants were asked what advice they would offer Mrs Tan regarding her treatment plans in the face of a poor prognosis, incurable cancer and costly treatment. Participants were then asked what their advice would be when the costs of treatment was covered by the patient’s insurance policy. Their responses were evaluated using Grounded Theory analysis. Setting/Subjects: 132 oncology patients and their caregivers were recruited from an ambulatory treatment unit at a tertiary oncology centre. Results: 63 (47.7%) of 132 participants advised Mrs Tan to opt for the QoL approach but when treatment costs were covered by insurance, only 5 (3.8%) of 132 participants chose QoL, whilst 108 (81.8%) participants chose QuoL options. Conclusion: Whilst cost is a significant factor in end of life decision making, strong sociocultural influences that perceive QoL approaches as ‘giving up’ ultimately determines the course of care.
Keywords
Quality of Life; Palliative medicine; Decision-making; End-of-life care; Treatment costs
Introduction
End of life decision making processes within the Singaporean context do not always prioritize the best interests of the patient [1-18]. Underpinning these concerns are three local practices. First, the continued dominance of family centric decision-making in end of life care, where decisions may favour the family’s interests rather than the patient’s. Second, local conceptions of Confucian inspired filial piety which requires that the family provide for the financial, physical, social, spiritual and emotional needs of the patient in recognition for their previous contributions to the family or as a result of their place within the family unit [1-18]. Third, mounting care costs do create potential for conflicts of interests in meeting the duty to care for the patient and the primacy placed on protecting the interests of the family. On one hand financial costs of caring for the patient at the end of life may see families conflicted over the pursuit Quantity of Life (QuoL) options that seek to prolong life such as chemotherapy or a Quality of Life (QoL) approach where available treatments such as chemotherapy is declined in favor of maximizing comfort and quality of life [19-34]. On the other social expectations to provide continued care of patients see families sometimes opt for sometimes ‘futile’ treatments in order to meet their filial obligations.
Singapore’s Health Care System
Singapore’s healthcare financing structure combines government subsidies with compulsory individual medical savings accounts called Medisave, which all working Singaporeans and their employers pay into monthly [20]. This “compulsory individual medical savings account scheme, which allows practically all Singaporeans to pay for their share of medical treatment” may be supplemented by Medishield insurance, the government’s basic healthcare insurance plan [19-21]. More comprehensive cover may be purchased through an integrated Medishield insurance plan [21]. All these schemes are subject to withdrawal limits and co-payments. Despite generous government subsidies, patients and their families may have to bear some out-ofpocket expenses [2,19-25]. Such expenses may include costs of renting medical equipment for home care and fees for some professional caregivers [22,23]. When the patient’s Medisave account is depleted, the family member’s finances may be affected as they dip into their own Medisave accounts or own savings to make payment instead [22,23].
Although it may be argued that family members are not obliged to do so, they often do in the face of regnant sociocultural beliefs that emphasize familial obligations to care for ill family members [1-18].
Filial Piety in Singapore
Filial piety revolves around the expectation that adult children must care and support their elders in recognition of the care they received earlier [31,35,36]. This obligation is often met in two ways, the provision of emotional, spiritual, physical and financial support at the end of life and by maintaining the patient’s ‘hopes’ and reducing ‘stress’. The former often translates to doing everything possible to prolong the life of the patient. The latter is seen as critical given that a loss of ‘hope’ or the presence of stress during periods of illness especially at the end of life is believed to hasten death. The culmination of both these factors often sees children colluding with health professionals to hide or moderate the diagnosis and/or prognosis to protect the parent from ‘concern and anxiety’, over their life-limiting illness and not infrequently pursuing second ‘opinions’, alternative treatment options and even futile treatment options in order to prolong the life of the patient [3-6,28-49].
The wider family and community police compliance of filial obligations [29,31-44]. Failure to meet these societal and familial standards is said to result in a ‘loss of face’ or personal honour for the immediate family, a fate fearfully avoided within the local community [4,14,29,31,33]. Thus being seen to be filial and to be meeting one’s duty to care for the patient is critical to some.
Views of Quality of Life Advocates
Given the societal backdrop, advocates for a Quality of Life (QoL) approach to care are often regarded suspiciously by families and by the wider society and this has an impact on end of life decision-making. Elucidating the views of patients and their caregivers as to QoL and QuoL options has a significant impact upon how end of life care and palliative and hospice care is perceived locally.
Study Methodology
Subjects
All patients and their caregivers were recruited from the Ambulatory Treatment Unit at the National Cancer Centre Singapore. Written informed consent was obtained from participants prior their participation in this Singhealth Centralized Institutional Review Board approved study. A total of 136 patients and caregivers were interviewed. Four interviews were incomplete and were excluded from data analysis given that they did not proceed beyond collection of demographic data (Table 1).
| Number of participants | 132 |
|---|---|
| Male, n (%) | 48 (36.4) |
| Female, n (%) | 84 (63.6) |
| Age, Mean (SD) | 49.7 (12.5) |
| Race, n (%) | |
| Chinese | 109 (82.6) |
| Malay | 3 (2.3) |
| Indian | 15 (11.4) |
| Other | 5 (3.8) |
| Education level, n (%) | |
| No formal education | 2 (1.5) |
| Primary | 24 (18.2) |
| Secondary | 60 (45.5) |
| Tertiary | 38 (28.8) |
| Professional qualifications | 8 (6.1) |
| Marital Status, n (%) | |
| Single | 14 (10.6) |
| Married | 110 (83.3) |
| Divorced | 3 (2.3) |
| Widowed | 5 (3.8) |
| Housing, n (%) | |
| 2/3-Room flat | 18 (13.6) |
| 4-Room flat | 82 (62.1) |
| Private condominium | 13 (9.8) |
| Landed property | 15 (11.4) |
| Other | 4 (3.0) |
Table 1: Respondent Demographics.
Participants and eligibility criteria
Convenience sampling was used to recruit patients, aged 21 or older, with a cancer diagnosis (any stage), and able to understand English or Mandarin. Patients identified primary caregivers, whom we recruited. They also had to be at least 21 and able to understand English or Mandarin. Nine trained interviewers carried out all the audio-recorded interviews. Transcription and translation to English (when required) was carried out by two of the authors.
Methodology
In deference to cultural sensitivities on discussing end of life issues, and in order to produce a less threatening means to explore sensitive topics, a video vignette was shown separately to patients and caregivers [4,14]. The video scenario depicted a family of three adult children who were discussing the treatment options for their mother (Mrs Tan) who was diagnosed with an advanced and incurable cancer. The doctor estimated that Mrs Tan would survive for seven to ten months if she opted for chemotherapy, or four months if she did not. Each adult child expressed a different view of how to proceed. One daughter focused upon the prohibitive costs of potential treatment compounded by the families’ financial difficulties following aggressive and expensive cancer treatment for their father who passed away last year. The second daughter focused upon the maximisation of Mrs Tan's quality of life (QoL) in the face of treatment side effects and poor anticipated response to chemotherapy. (This approach does not negate treating remediable causes of deterioration). Mrs Tan's only son advocated a quantity of life (QuoL) approach which focuses on life prolonging efforts. We asked participants a series of questions using a semistructured questionnaire to scrutinize the impact of cost on treatment decisions. This questionnaire was designed using prevailing local data, feedback from patients, and input from our panel of local experts.
Coding
The completed transcripts of the audio-taped interviews were labelled with unique numeric identifiers and de-identified. The 132 completed transcripts were coded manually and independently by three members of the investigating team. We used Grounded Theory to identify key ideas, which evolved during thematic analysis. Saturation of thematic analysis was attained within the first 30 cases and there were no contradicting data in the following 100 cases. Any discordance in the coding was discussed by all the members of the team and a majority verdict was applied. Not all questions were answered by the participants and caregivers. This was mainly because they were called away for treatment.
Results
The choice between quality and quantity of life
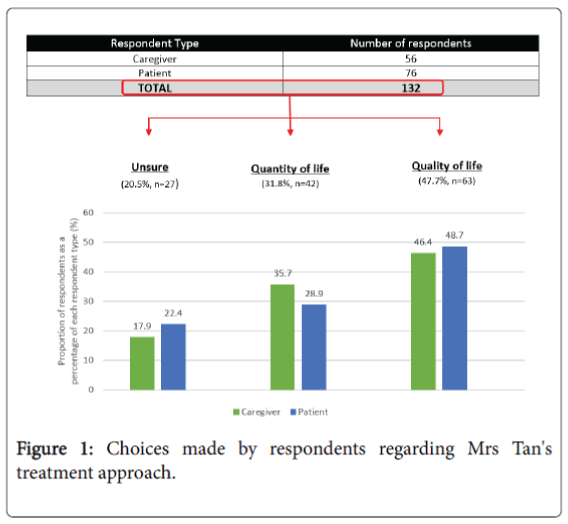
Participants were asked whether Mrs Tan should pursue a quality of life (QoL) approach to avoid any side effects and conserve the family’s financial resources, or adopt a Quantity of Life (QuoL) approach, which involved treatment such as chemotherapy but would likely cause side effects and be expensive. Of the 132 responses, 47.7% (63) opted for a QoL approach, 31.8% (41) preferred a QuoL approach and 20.5% (27) were unsure (Figure 1).
Caregivers
Twenty (35.7%) of 56 caregivers opted for QuoL measures (Figure 1). Caregivers believed this approach was optimistic, avoided ‘bad’ news, maintained hope and supported the patient. Most were "not yet ready to let go" and wished for the patient to keep fighting.
Twenty six (46.4%) of the 56 caregivers preferred QoL and although QuoL was important, it “was not worth it” if the patient suffered as a result. Ten (17.9%) caregivers struggled to determine what was best for the patient.
Patients
Thirty seven (48.7%) of the 76 patients valued QoL over QuoL, citing concerns about the side effects of chemotherapy, Mrs Tan's age at diagnosis and poor prognosis. Most (91.9%) of these 37 patients saw the cessation of treatment as the natural end-point to Mrs Tan's disease journey.
Twelve (32.4%) of these 37 patients saw a QoL approach as something to “settle for” if there were no treatment options, treatment was unaffordable or treatment side-effects were unbearable.
Conversely 39 (51.3%) patients chose QuoL because it offered a 'chance' to prolong life, ameliorate suffering and demonstrated the patient did not give up. Seventeen (22.4%) of 76 patients were unsure given insufficient information featured in our vignette.
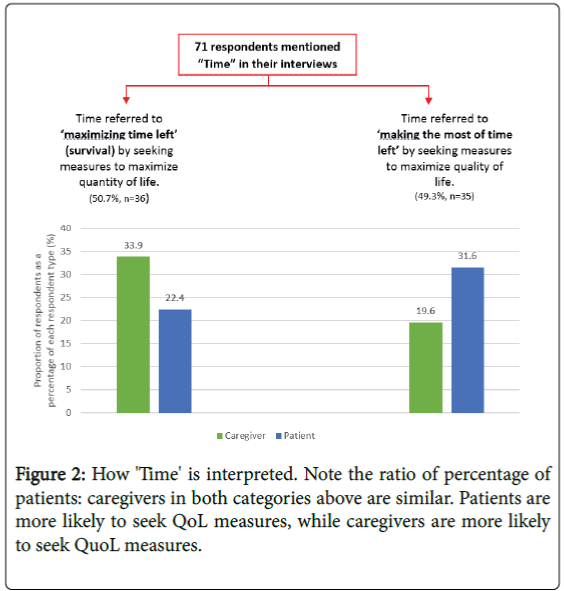
Time
The most significant consideration in the choice between a QoL and a QuoL approach was how best to use the time remaining. Of the 71 respondents, 36 (50.7%) favoured a QuoL approach, while 35 (49.3%) favoured QoL. Patients (31.6%) veered toward QoL measures and caregivers (33.9%) preferred QuoL measures (Figure 2).
Importance of cost
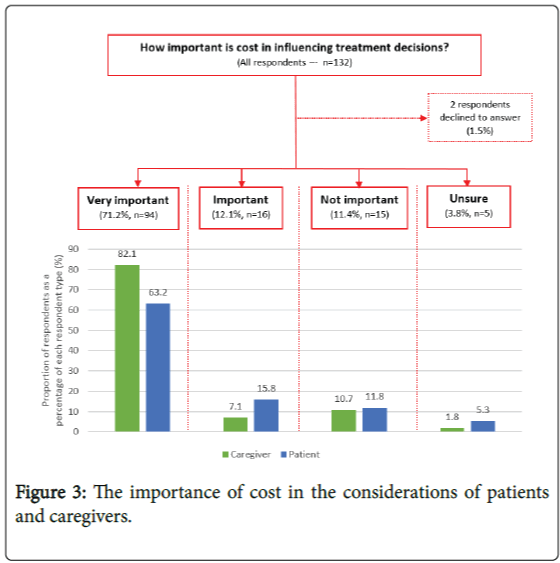
More than 80% of our participants indicated that their treatment decisions were dictated by treatment costs (Figure 3).
Sixty (78.9%) patients and 50 (89.3%) caregivers said cost was very important or important whilst 9 (11.8%) patients and 6 (10.7%) caregivers reported that cost were unimportant. The remainder were unsure.
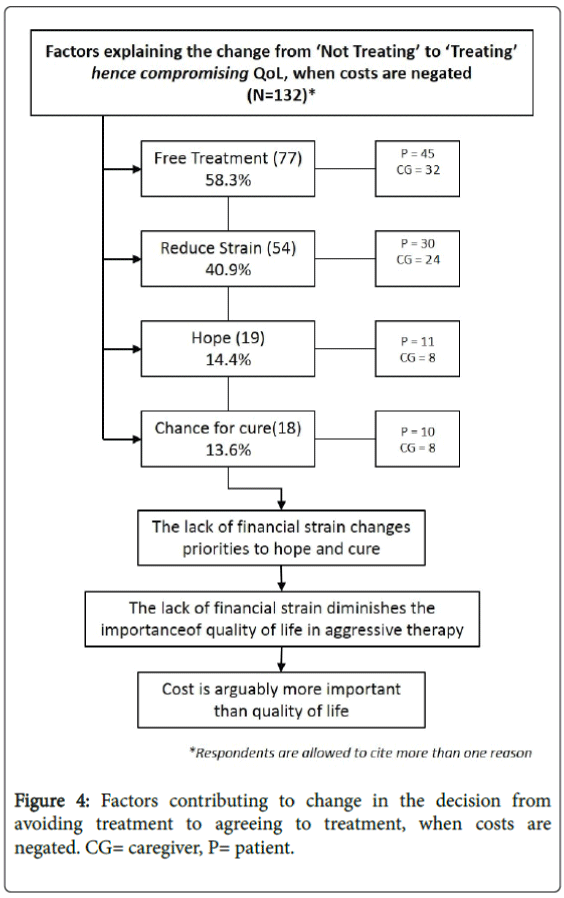
When the importance of cost is negated
When costs were covered by insurance and care effectively 'free', 109 (82.6%) of 132 participants said they would opt for a QuoL approach. Five participants (3.8%) maintained a QoL approach and 18 (13.6%) were unsure. The rationale for a QuoL approach even at the cost of QoL revolved around hope and maximising their chances of survival and even cure. “Just try it out” and “Why not go for it?” conveyed the dominant sentiments even amongst those who had previously chosen QoL over QuoL (Figure 4).
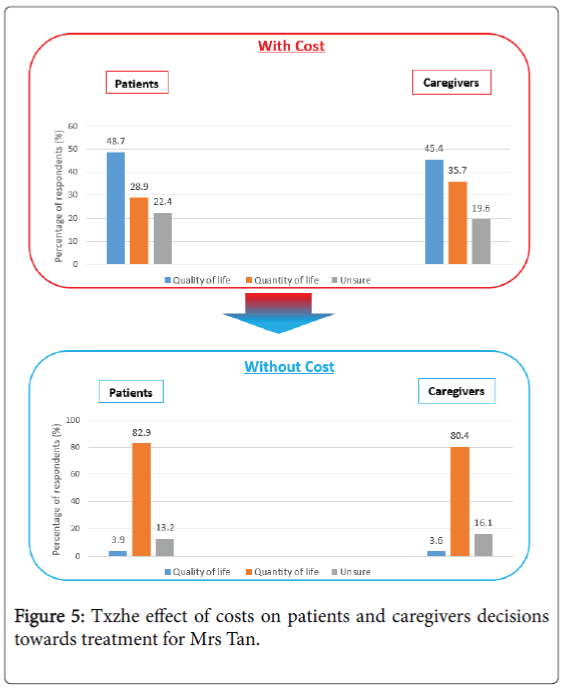
When cost was irrelevant, respondents heavily favoured QuoL (Figure 5). The proportion of patients choosing QuoL shifted from 28.9% (22 of 76 patients) to 82.9% (63 of 76 patients), and the proportion of caregivers choosing QuoL shifted from 35.7% (20 of 56 caregivers) to 80.4% (45 of 56 caregivers).
Two (3.6%) caregivers maintained their QoL position despite free treatment based on 'social concerns' such as the need to accompany patients to therapy, changes in lifestyle, and the potential for “suffering”. Forty-five (80.4%) caregivers stated if treatment was free the risk-benefit analysis tipped in favour of a QuoL approach.
Discussion
Our data suggests that decisions between QoL and QuoL options in terminal cancer are defined by cost concerns. But the truth is more nuanced. A review of participant responses revealed that there was a poor understanding of QoL measures and palliative care, which was equated to 'giving up' and abandonment. So, it is unsurprising that most participants believed that a QoL approach is only acceptable when care costs are prohibitive, and when there was little realistic chance of improving the patient's condition. Patients and caregivers believed free treatment cannot be rejected when the patient looked as “well” as Mrs Tan was. Patients are also expected to set an example by ‘fighting on’ and not ‘giving up’ rather than adopting a QoL approach perceived as 'wishing to hasten death'. Failure to meet these expectations reflects poorly on the family and is liable to result in a loss of 'face'.
Caregivers felt obliged to opt for the QuoL approach when treatment was free because it was “easier to live with” and relieved their concerns of guilt and abandonment. Whilst they are expected to protect familial interests, they are also expected to continue to provide physical, financial, emotional and spiritual care, maintain hope and not abandon family members [31,49]. Many caregivers reported being illprepared for either the pressures of being decision-makers or the inevitable scrutiny of their intentions should they opt for a QoL approach when treatment is free.
Study Limitations
The primary limitation of our study is the variances in the pervasiveness and the interpretation of filial obligations amongst participants. However consistent with prevailing data our findings do highlight the continued albeit evolving role filial obligations have upon the manner that end of life decisions are made in Singapore [31,45-49].
Conclusion
This study into the considerations behind end of life decision making in Singapore indicates that cost is a significant factor in treatment decisions. However, filial obligations and societal expectations also have an impact and should not be underestimated. Excessive cost and poor prognosis are more palatable reasons not to pursue treatment rather than stating the interests of the family outweigh those of the patient. Whilst efforts to make treatment options more affordable continue to be welcomed, demystifying the role and purpose of a QoL approach will promote patient centered and allow palliative care to thrive.
Acknowledgements
This study was funded by a research grant from the Lien Centre of Palliative Care. The authors would like to thank Dr Deborah Susan Watkinson who contributed significantly to the conceptualizing, design and grant application for this study and who sadly passed away before its completion.
References
- Ong JK, Back MF, Lu JJ, Shakespeare TS, J Wynne CJ (2002) Cultural Attitudes to cancer management in traditional South East Asian Patients. AustralasRadiol 46: 370-374.
- Ong WY, Yee CM, Lee A (2012) Ethical dilemmas in the care of cancer patients near the end of life. Singapore Med J 53: 11-16.
- Low JA, Kiow SL, Main N, Luan KK, Sun PW, et al. (2009) Reducing collusion between family members and clinicians of patients referred to the palliative care team. Perm J 13: 11-15.
- Goh CR (2008) Challenges of cultural diversity. In J Beattie & S Goodlin (eds.) Supportive Care in Heart Failure Oxford, New York: Oxford University Press 451-461.
- Toh HC (2011) Providing hope in terminal cancer: when is it appropriate and when is it not? Ann Acad Med Singapore 40: 50-55.
- Tan TK, Teo FC, Wong K, Lim HL (1993) Cancer: To tell or not to tell? Singapore Med J 34: 202-203.
- Kuah KE (2007) Confucian ideology and social engineering in Singapore. J ContempPhys 20: 370-389.
- McCarthy T (1998) In defense of Asian values: Singapore’s Lee Kuan Yew. Time.
- Qiang L (2001) Core culture values and beliefs of Singapore.
- Tan C (2012) Our Shared Values in Singapore: A Confucian Perspective. Educational Theory 62: 449-463.
- Wu HY, Kei AL, Onn IL, Hwang MK, Chan S (2006) Older adults' attitudes to death, palliative treatment and hospice care: a view from Singapore. Palliat Med 20: 117-118.
- Nakada H, Arakawa M (2016) Caregiver Perspectives on End-of-Life Experiences of Patients With Left Ventricular Assist Devices. JAMA Intern Med 176: 1231.
- Teo P, Chan A, Straughan P (2003) Provid ing health care for older persons in Singapore. Health Policy 64: 399-413.
- Goh CR (2007) Culture, ethnicity and illness. in Palliative Medicine TD Walsh, AT Caraceni, R Fainsinger, KM Foley, P Glare, C Goh, M Lloyd-Williams, JN Olarte& L Radbruch (eds.), PA:Saunders/Elsevier Philadelphia 51-54.
- Lee A, Wu HY (2002) Diagnosis disclosure in cancer patients--when the family says "no!". Singapore Med J 43: 533-538.
- Back MF, Huak CY (2005) Family centred decision making and non-disclosure of diagnosis in a South East Asian oncology practice. Psychooncology 14: 1052-1059.
- Ng R, Lip H (2009) Advance care planning: lets talk about your preferences for care at the end of life. Singapore Fam Physician 35: 93–99.
- Tsai DF (2001) How should doctors approach patients? A Confucian reflection on personhood. J Med Ethics 27: 44-50.
- (2014) Costs and Financing. Ministry of Health, Singapore.
- Medisave (2014) Ministry of Health Singapore.
- Medishield (2014) Ministry of Health Singapore.
- Lim MK (2004) Shifting the burden of health care finance: a case study of public-private partnership in Singapore. Health Policy 69: 83-92.
- Krishna LR (2012) Best interests determination within the Singapore context. Nurs Ethics 19: 787-799.
- Brydon K (2011) Social policy in Singapore: insights from a social work perspective. Asian Social Work and Policy Review 5: 20-32.
- Khan H (2011) Social policy in Singapore: A Confucian Model. The International Bank for Reconstruction.
- (2014) The Maintenance of Parent Act, Official Web Site.
- (1991) White Paper, Shared Values. Singapore.
- Krishna L (2011) Nasogastric feeding at the end of life: a virtue ethics approach. Nurs Ethics 18: 485-494.
- Krishna L (2011) The position of the family of palliative care patients within the decision making process at the end of life in Singapore. Ethics Med 27: 183–190.
- Krishna L, Chin J (2011) Palliative sedation within the duty of palliative care within the Singaporean clinical context. Asian Bioeth Rev 3: 201–215.
- Ho ZJ, Radha Krishna LK, Yee CP (2010) Chinese familial tradition and Western influence: a case study in Singapore on decision making at the end of life. J Pain Symptom Manage 40: 932-937.
- Krishna L (2011) Decision making at the end of life: A Singaporean Perspective. Asian Bioethics Review 3:118-126.
- Krishna LK, Watkinson DS, Beng NL (2015) Limits to relational autonomy--the Singaporean experience. Nurs Ethics 22: 331-340.
- Krishna LKR, Menon S (2014) Understanding the Practice of Collusion on End of Life Care in Singapore. J Med Research 4: 8.
- Tsai DF (1999) Ancient Chinese medical ethics and the four principles of biomedical ethics. J Med Ethics 25: 315-321.
- Tsai DF (2005) The bioethical principles and Confucius' moral philosophy. J Med Ethics 31: 159-163.
- Hui E (2008) Parental refusal of life-saving treatments for adolescents: Chinese familism in medical decision-making re-visited. Bioethics 22: 286-295.
- Pang MC (1999) Protective truthfulness: the Chinese way of safeguarding patients in informed treatment decisions. J Med Ethics 25: 247-253.
- Fan R (2002) Reconsidering surrogate decision making: Aristotelianism and Confucianism on ideal human relations. Philos East West 52: 346-372.
- Fan R (2007) Which care? Whose responsibility? And why family? A Confucian account of long-term care for the elderly. J Med Philos 32: 495-517.
- Fan R (1997) Self-determination vs. family-determination: two incommensurable principles of autonomy: a report from East Asia. Bioethics 11: 309-322.
- Cheng KY, Ming T, Lai A (2012) Can familism be justified? Bioethics 26: 431-439.
- Tan JOA, Chin JJL. Kaan TSH, Chan TE (2011) What Doctors say about care of the dying. Lien Foundation Singapore.
- Chai HZ, Krishna LKR, Wong VHM (2013) Feeding: What it means to patients and caregivers and how these views influence Singaporean Chinese Caregivers’ decisions to continue feeding at the end of life. Am J Hos Pall Med.
- Krishna LK, Alsuwaigh R, Miti PT, Wei SS, Ling KH, et al. (2014) The influence of the family in conceptions of personhood in the palliative care setting in Singapore and its influence upon decision making. Am J HospPalliat Care 31: 645-654.
- Ching JA, Quah YL, Yang GM, Menon S, Radha Krishna LK (2013) Patient and family involvement in decision making for management of cancer patients at a centre in Singapore. BMJ Support Palliat Care.
- Yang GM, Kwee AK, Krishna L (2012) Should Patients and Family be Involved in "Do Not Resuscitate" Decisions? Views of Oncology and Palliative Care Doctors and Nurses. Indian J Palliat Care 18: 52-58.
- Wong VHM, Krishna LKR (2014) The Meaning of Food amongst Terminally Ill Chinese Patients and Families in Singapore. J Med Research.
- Tsai DFC (2002) The Two-Dimensional Concept of Confucian Personhood in Biomedical Practice, Daniel Fu-Chang Tsai, in Ole Doering and Chen Renbiao (Eds.) Advances in Chinese Medical Ethics: Chinese and International Perspectives 195-213.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 13379
- [From(publication date):
July-2016 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 12459
- PDF downloads : 920