Stress Response and Emotional Security in the Intergenerational Transmission of Depressive Symptoms
Received: 07-Aug-2015 / Accepted Date: 26-Feb-2016 / Published Date: 29-Feb-2016 DOI: 10.4172/2375-4494.1000283
Abstract
The aim of this study is to focus on stress reactivity as a moderator of the transmission of depression from mothers to adolescents through emotional insecurity. One hundred mother-adolescent dyads living in the Northeast of the United States were examined, with adolescents between the ages of 13 to 17. Data was collected in the home through surveys, a mother-adolescent interaction task and physiological measures from the adolescent to examine stress response. Results suggested that adolescents’ emotional insecurity mediated the relationship between maternal and adolescent depressive symptoms. Findings also provided some support that adolescents who evidenced a higher stress response to the conflict interaction task appeared more vulnerable to the transmission of depression through emotional insecurity. These findings can help in the understanding the intergenerational transmission of depressive symptoms from mothers to adolescents through important factors such as quality of attachment and stress reactivity.
Keywords: Adolescence; Depressive symptoms; Emotional insecurity; Stress response
218173Introduction
Depressive disorders are accountable for several deaths a year with about seven in every 100,000 adolescents committing suicide in America every year due to depression [1]. The risk for depressive disorders during adolescence may be influenced by genetic and intergenerational components; studies indicate that a correlation exists between maternal depression and adolescent depression [2,3]. Identifying the underlying mechanisms that explain this transmission remains an important area of research. One potential mechanism that might account for this transmission is the extent to which adolescents feel they can count on their mothers for support and for a sense of security. Mothers who exhibit depressive symptoms may not have a warm and secure relationship with their adolescents, placing adolescents at risk for depressive symptoms [4]. Thus, one reason that depressive symptoms may be passed down from mothers to their adolescents is because maternal depressive symptoms impact adolescents’ sense of emotional security within the parent-adolescent relationship, which in turn may lead to increased depressive symptoms among adolescents [5,6]. To date, however, few studies have examined mechanisms that may help explain the transmission of depression from mothers to children during adolescence, with most studies only examining this transmission through emotional security in childhood.
In addition to identifying possible mechanisms that explain the transmission of depressive symptoms from mothers to adolescents, it is also important to examine which adolescents might be most vulnerable to this transmission. Stress has an important impact on the body and how emotions are managed and may act as a vulnerability for this transmission [7]. To our knowledge, research has not examined whether adolescents’ stress response may affect the transmission of depression symptoms from mother to adolescent. Thus, the goal of this study is to examine if adolescents’ stress response, as measured by heart rate, blood pressure, and self-reported affect moderates the effects of maternal depressive symptoms and emotional security on adolescents’ depressive symptoms.
Transmission of Depressive Symptoms
Maternal and adolescent depressive symptoms
Maternal depression and adolescent depression are highly correlated, suggesting that depressive symptoms are passed down in families and children of depressed mothers are at an increased risk of developing depression later in life [2,6,8]. Depression may be affected by specific and nonspecific factors [9]. A specific factor may be an immediate family member who has depression (i.e. mother) and a nonspecific factor may be the childhood that was experienced (e.g., a negative environment of poor parenting). If an adolescent has both of these factors, they are at a high risk for depression [10], which may be due to the adolescent’s inability to cope with stressful situations [2].
Transmission of depressive symptoms through emotional security
There are several different factors that may link maternal depressive symptoms to depressive symptoms in adolescents [2,4,10]. An important factor that deserves more research is the emotional security that adolescents’ feel in the parent-adolescent relationship. The construct of emotional security stems from attachment theory which proposes that children have a sense of felt security or insecurity depending on parenting behaviors. Children who are insecurely attached have trouble seeking help from their mothers and difficulty regulating their emotions when compared to securely attached children [6]. Davies et al. [11] extension of attachment theory proposes that a child’s sense of emotional security is based on past experiences between the parent and child that the child uses to cope with certain situations in the present and the future. Emotional security is the driving force behind emotion regulation and coping in the face of stress. If a child is introduced to a destructive environment while growing up, the child is less likely to develop a secure sense of emotional security for future life experiences.
Adolescence may be a particularly critical period for developing a sense of security in the family context and may put adolescents at risk for adjustment problems [5]. Specifically, instability within the family (e.g. maternal depression) may negatively impact adolescent’s sense of emotional security and put the adolescent at risk for psychological problems later in life [5,11,12] implying that emotional security may play an important role in adolescents’ depressive symptoms.
Few studies have examined the pathway between maternal depressive symptoms and adolescent depressive symptoms through emotional security. Exceptions include, studies by [2,6] both of which suggested that depressed mothers were at a higher risk for a negative parenting style, which impacted the child’s sense of emotional security and longitudinally predicted depressive symptoms in children. Similarly, Teti et al. [4] examined the transmission of depressive symptoms through a longitudinal design using depressed and nondepressed mothers and their infants. Results indicated that children who had strategies for coping with stressful situations among their attachment figure were less at risk for depressive symptoms than children with no attachment strategies. The small percentage of children with a secure attachment to their mothers were less stressed (through observational analysis) and expressed low levels of depressive symptoms, suggesting that children’s handling of stress may make them more or less vulnerable to the transmission of depressive symptoms. The current study will build on this research and examine the full pathway from maternal depressive symptoms to adolescent depressive symptoms through the mediator of emotional insecurity.
Stress response
Adolescents’ stress response may increase adolescents’ vulnerability for the intergenerational transmission of depressive symptoms. When an adolescent is exposed to adversity over a long period of time, they may evidence very high levels of stress during and after stressful situations [13]. Stress response can be measured through behavioral indicators (e.g., expressed affect), as well as physiological responses (e.g., heart rate and blood pressure). When the body experiences a stressful situation, the necessary systems are inhibited while others remain activated. This process is vital in the short term, however, if this response remains active over long periods of time, it can lead to a dysregulation of the body’s natural stress response both in times of acute stress and times of rest. This dysregulation may be seen in an extreme physiological response to acute stressor and trouble down regulating that response as indicated by high heart rate or blood pressure. Adolescents may also evidence variability in stress response through negative affect. Negative affect can include emotions such as distress and sadness [14]. Research suggests that adolescents may exhibit negative affect in the face of stress [15], which in turn may contribute to depressive symptoms.
Ellis et al. [7] proposed the biological sensitivity to context theory (BSC), which suggests that adolescents interpret stressful situations depending on their level of stress reactivity, and the context in which they develop. These individual differences in reactivity may have developed as a result of genetic and early environmental experiences. This concept is similar to the diathesis-stress perspective in which an individual has a vulnerability to develop a dysregulated stress response and this vulnerability increases adolescents’ chances of developing depression if they are exposed to stressful life experiences [16]. Ellis et al. [7] found that adolescents who evidence high stress reactivity are sensitive to the effects of both positive and negative environments on development. If an adolescent was exposed to a stressful environment, such as the environment that may be experienced in homes where mothers report depressive symptoms, the adolescent will be at a greater risk for psychological problems later on in development. BSC explains that high stress reactivity is not necessarily a vulnerability, however, it can create a vulnerability if the surrounding environment is negative. This view differs from that of a diathesis-stress perspective, which would view adolescents’ heightened stress response only as a vulnerability. Across both theories, though, adolescents’ stress reactivity would act as a vulnerability that would increase the transmission of depressive symptoms within the family.
Emotional security, stress response and depression
Adolescents who evidence heightened stress reactivity and a more emotionally insecure relationship with their depressed mothers may be more vulnerable to developing depressive symptoms than youth who do not evidence these vulnerabilities. Studies have not specifically examined the impact that stress reactivity may have on the transmission of depressive symptoms from mothers to adolescents. However, related research by Lupien et al. [17] reviewed articles that examined the effects of stress on both animals and humans. These researchers found that parent-child interactions as well as the psychological state of the mother had an effect on a child’s stress and behaviors in the future such that if a child did not receive adequate care and attention from their mother, they were more vulnerable for health problems, especially if the child was introduced to stressful situations. According to Lupien, the brain is most vulnerable to stress during adolescence. If an adolescent does not experience a warm secure relationship with their maternal caregiver, the adolescent will be vulnerable to stressful environments because they will not have the experience to handle and cope with stress. Research suggests that this inability to cope with stress may create a higher risk for adolescents to develop psychopathology such as depression [18].
Research also supports the assertion that stress reactivity and context may work in concert to affect adjustment. Obradovic, et al. [19] found that children with a heightened stress response were at an increased risk for behavioral and health problems in high stress environments (e.g. marital conflict or divorce); whereas children with heightened stress response in low stress environments did not show risk for behavioral or health problems. In a laboratory study, Obradovic, et al. [20] elicited stress response from children using different challenging tasks and found that highly reactive children that were faced with a difficult task or marital conflict displayed higher levels of anxiety, frustration and other internalizing symptoms because highly reactive children were sensitive to context and had a difficult time managing negative emotions. Lewinsohn, et al. [21] suggested that an adolescent’s vulnerability to internalizing behaviors (e.g. depressive symptoms) may be due to a diathesis-stress effect. The researchers conducted a longitudinal study with high school students and found that some adolescents that were introduced to a stressful and negative context (e.g., fights with parents) were at increased risk for depressive symptoms in comparison to other students indicating that there may be a trait vulnerability to internalizing symptoms that is exacerbated under stressful environments. Finally, a recent study by Waugh, et al. [22] found that dysregulation of stress in young girls of depressed mothers put the girls at risk for depressive symptoms. Girls that had a dysregulated stress response and experienced more negative affect from their mothers displayed higher depressive symptoms. This research provides preliminary evidence that the transmission of maternal depressive symptoms to adolescents through emotional insecurity is exasperated for adolescents who evidence a heightened stress response.
Hypotheses
There are several studies that support the relationship between adolescent depression and maternal depression. These studies are limited, however, because they do not focus on emotional security as a possible explanation as to why depressive symptoms may be transmitted from mothers to adolescents and they do not look at possible moderators to this pathway. Thus, this study examines whether a dysregulated stress response creates a vulnerability in the transmission of depressive symptoms from mothers to adolescents. Specifically, we hypothesize that emotional security will act as a mediator such that one reason why maternal depressive symptoms and adolescent depressive symptoms will be associated is because adolescents develop a sense of emotional insecurity. Secondly, we hypothesize that a dysregulated stress response will heighten the negative impact of maternal depressive symptoms on emotional insecurity and adolescent depressive symptoms, such that adolescents with a heightened stress response will be more at risk for the negative effects of maternal depression than adolescents who do not evidence a dysregulated stress response.
Method
Participant
Participants were 100 adolescents (68% female, 78% Caucasian) and their maternal caregivers (91% biological) who live in the Northeastern part of the United States, in close proximity to an urban city. Adolescents in 9th thru 11th grade between the ages of 13 and 17 (M = 15.1, SD = 0.98) were recruited through flyers posted in businesses and places that parents and adolescents frequent (e.g., libraries), the American Student List (commercial mailing list) and speaking to adolescents and parents at local events and private schools in the area. Seventy-four percent of the mothers reported being married, with 64% of that total reporting that this was their first marriage. The median level of education for mothers was a college degree (41%). The median level household income for the family was reported as falling between $80,000 and $89,999 which is similar to married-couple families within the state ($88,243 Income) [23].
Procedure
Data were collected through a 2½ hour home visit. Prior to the home visit, consent was obtained from the mothers, fathers (when available) and the adolescents. During that time, measures of heart rate and blood pressure were obtained from the adolescent at five different time periods (baseline, peak - right after stressor, and the recovery period after the stressor) in order to measure how the adolescent copes with stressful situations. To obtain the baseline, the adolescent watched a relaxation DVD (sea or nature video) for 20 minutes and measures of heart rate and blood pressure were obtained twice during that time.
Surveys were also given to both the adolescent and the mother to measure demographics, parenting and internalizing/externalizing behaviors. Two videotaped interaction tasks also took place between the mother and the adolescent about an issue of conflict within the home and outside of the home. The issue of conflict within the home was obtained through a Family Issues Checklist [24], which included topics of conflict such as doing homework and coming home on time. The issue of conflict outside of the home was obtained by asking the adolescent to identify an issue (e.g. a problem with a friend) that they are experiencing outside of the home. Each interaction task was eight minutes long and heart rate was obtained every 30 seconds throughout each interaction task. The purpose of the interaction tasks for this study was to induce stress that adolescents might experience in everyday interactions with their parent. The mother and adolescent were compensated $40 each for their time on the study.
Measures
Control variables: Gender was the only control in these analyses because it was the only demographic variable that had a significant relationship with variables of interest in this study. Male participants were coded as a zero and female participants as a one.
Maternal depressive symptoms: It is important to note in this study that we were not looking at clinical levels of depression but just symptoms of depression that might indicate a disturbance by not meet diagnostic criteria. Subclinical levels of depressed symptoms may include low self-esteem, decreased motivation, sadness, and difficulty in finding pleasure in formerly pleasurable activities. The Center for Epidemiologic Studies Depression Scale [25] was used to measure maternal depressive symptoms. Depressive behaviors on the CES-D Scale include statements such as “I felt everything I did was an effort” and “I felt lonely.” Response options range from a 1 (Rarely or none of the time) to a 4 (Most or all of the time) where higher scores represented a higher level of depressive symptoms. The CES-D is a widely used instrument and demonstrated good reliability (α = 0.89).
Parent/Adolescent emotional security: Emotional security was measured through the Inventory of Parent and Peer Attachment [26] on the adolescent survey which assesses warmth, support, communication, and alienation in the parent-adolescent relationship. Sample items include “My mother accepts me as I am” and “When we discuss things, my mother cares about my point of view.” Responses range from a 1 (Almost Always or Always True) to a 5 (Almost Never or Never True) where higher scores represent a lower level of emotional security. This scale has been used to describe attachment and emotional security [27,28]. The IPPA had high reliability (α = 0.94).
Stress response: Stress response was measured through cardiovascular response. A Contec 08C blood pressure cuff was used to assess systolic blood pressure (SBP) and diastolic blood pressure (DBP). A Pulsox sensor was attached to the adolescent’s finger to assess heart rate (HR). Blood pressure and heart rate were obtained at various time points during the visit and in the middle of the two interaction tasks. These time points included a baseline measure, peak measure, and a recovery period. For the analysis, a peak minus baseline score was used for heart rate and blood pressure measures. Heart rate was obtained every 30 seconds during each interaction task. In addition to cardiovascular response, self-report of emotions was obtained six times over the course of the visit through the negative affect subscale of the PANAS which measured emotions such as, “Irritable” and “Upset” and responses ranged from a 1 (Very slightly or Not at all) to a 5 (Extremely). Reliability for the baseline negative affect scale and the peak negative affect scale were α = 0.80 and 0.83, respectively. Winsoring was used for the stress reactivity measures that were three standard deviations away from the mean. Past literature supports the use of winsoring to deal with large outliers [29].
Adolescent depressive symptoms: Adolescent depressive symptoms were measured with the Child Behavior Checklist Scale [30,31] from both the mother’s and the adolescent’s survey. Statements included “I feel confused or in a fog” and “I am overtired.” Responses range from 1 (Not true) to 3 (Very/Often true) where higher scores represent a higher level of internalizing behaviors. For purposes of this project, adolescent’s report on the YSR (α = 0.90) and the mother’s report on the CBCL (α = 0.85) were used to create an average variable representing adolescent depressive symptoms.
Analytic strategy
To examine the mediational and moderation hypotheses AMOS 20.0 structural equation-modeling program (SEM) was used to estimate path models. The first step in data analysis examined the direct relationship between maternal depressive symptoms and adolescent depressive symptoms. The second step included the emotional insecurity variable in the model to see if it minimized the direct relationship between maternal depression and adolescent depression. Model fit for path models was examined using the chisquare goodness of fit statistic, the comparative fit indices (CFI), and the standardized root mean square residual (SRMR). A non-significant chi-square indicated a good model fit [32]. CFI values of 0.95 or higher indicated a good model fit and SRMR values below 0.09 indicated a good model fit [33,34]. Error variances were included for all the dependent variables. The significance of all models was set at p < 0.05.
To examine the moderating hypothesis, we created a count variable comprised of adolescents’ Autonomic Nervous system (ANS) response as measured by peak minus baseline of heart rate, SBP and DBP to the family based stressor. Research suggests that heart rate variability as well as blood pressure are good indicators of ANS as these physiological measures are key contributors to sympathetic nervous system activation [35]. To reflect heightened reactivity each peak minus baseline score was then recoded, such that participants scoring in the top 75% for each physiological measure received a score of one and every other participant below 75% received a score of zero [36]. A count variable, ranging from 0 (no ANS response in the top 75%) to 3 (ANS response on all 3 indicators above 75%) was created [36] and then recoded into two different groups, participants who scored in the top 75% for one of the physiological measures were given a score of one and labelled higher reactivity and individuals who scored below 75% on all three measures were coded zero. These variables were entered as a grouping variable in a multiple group model in AMOS. Multiple group models allowed researchers to test if the regression pathways differed across groups. This was accomplished by comparing a model that is fully constrained to a model that allows the regression pathways to vary across the groups (e.g., maternal depression to emotional insecurity). A second multiple group model was also tested using negative affect data, difference scores were created for negative affect and participants in the top 75% of increased negative affect received a score of one and all others scoring below the 75% received a score of zero [37].
To examine if moderation was present several criteria that included chi square difference tests, critical ratios, and if coefficients differed across the models in their significance level were used. In the context of multiple group models, chi square difference tests compare a model where pathways are assumed to be equal across groups and a model where pathways are assumed to be different across groups, with a significant p-value indicating that the model where paths are allowed to vary across groups is the better fitting model. Standardized coefficients and critical ratios were also examined for other evidence of moderation. Critical ratios above 1.96 indicated a significant difference in the regression pathways across models [38]. Full information maximum likelihood estimation procedure (FIML) was used in this study.
Results
Bivariate correlations, means and standard deviations were obtained for all variables (Table 1).
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| 1.Maternal depression | - | ||||||
| 2. Adolescent depression-adolescent report | 0.16 | - | |||||
| 3. Adolescent depression-mom report | 0.33** | 0.60** | - | ||||
| 4. Emotional Insecurity | 0.20* | 0.33** | 0.21* | - | |||
| 5. Gender | 0.17 | 0.25* | 0.29** | 0.19 | |||
| 6. ANS | 0.07 | 0.07 | 0.04 | 0.11 | 0.07 | - | - |
| 7. Negative affect | 0.06 | 0.20* | 0.12 | 0.31* | -0.05 | -0.03 | |
| M | 1.5 | 1.51 | 1.38 | 2.17 | N/A | 0.58 | 0.25 |
| SD | 0.43 | 0.41 | 0.32 | 0.69 | N/A | 0.5 | 0.44 |
Note: * indicates a significant relationship at p < 0.05 and ** indicates a significant relationship at p < 0.01. For gender, males coded zero and females were coded one.
Table 1: Means, Standard Deviations and Correlations between Study Variables (N = 100).
Mediation
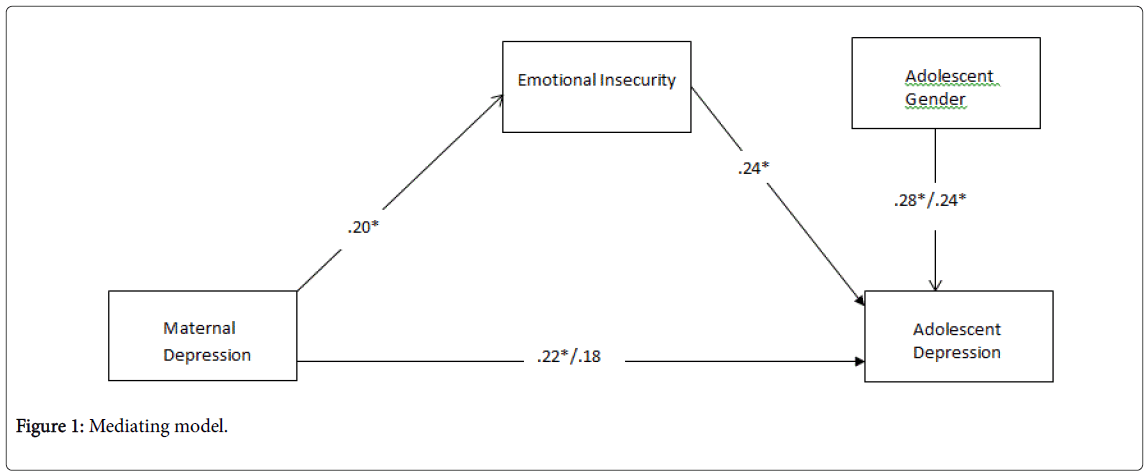
In the direct effect model we found a significant association between maternal depressive symptoms and adolescent depressive symptoms (β = 0.22, p = 0.02), 95% CFI [0.02, 0.37] indicating that higher maternal reports of depressive symptoms were correlated with higher reports of adolescent depressive symptoms. When emotional insecurity was included into the model, the direct effect between maternal and adolescent depressive symptoms was reduced to non-significance (β = 0.18, p = 0.06), 95% CFI [0.01, 0.31] indicating mediation (Figure 1). Sobel’s test was used to test for mediation and approached significance at z = 1.69 p = 0.05. Comparative fit index (CFI) = 0.93 indicated a good model fit and SRMR = 0.05 indicated an adequate fit to the mediating model. The chi-square of the model was non-significant χ2 = 2.67, df = 1, p > 0.05.
Moderation
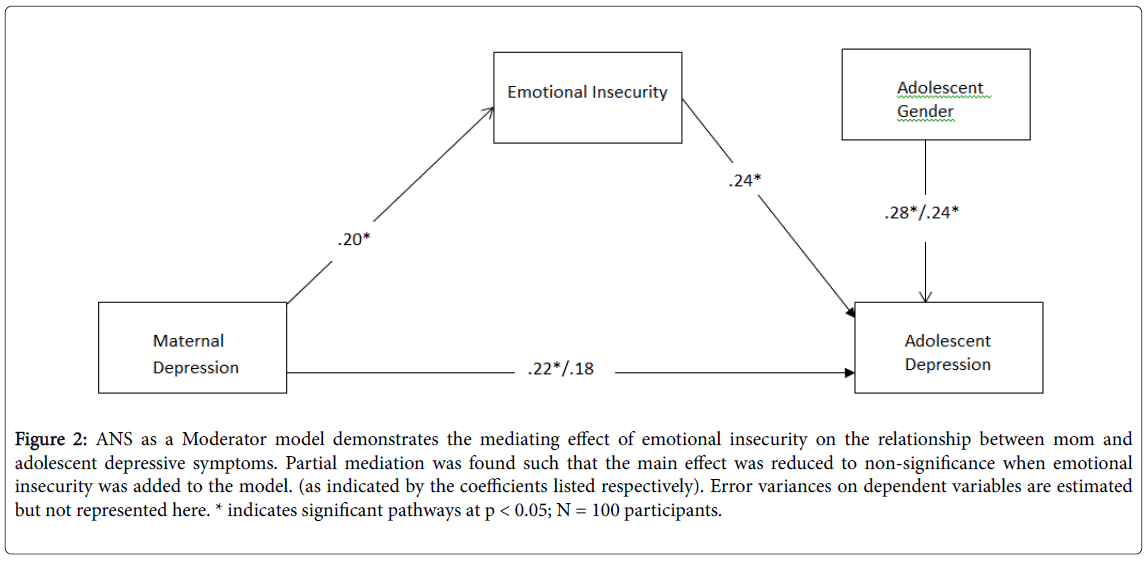
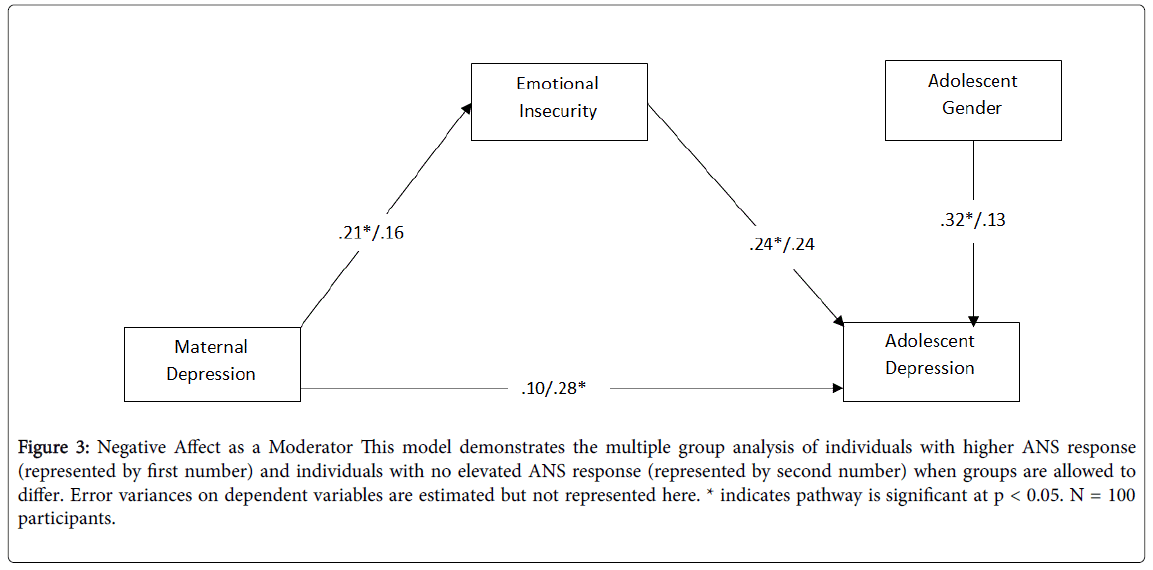
ANS response: Results from the group difference test indicated that there was not a significant change in chi-square when the paths were allowed to differ for those high in ANS and those low in ANS, Δχ2 = 2.83, df = 4, p = 0.58 (Figure 2). None of the critical ratios reached 1.96. Although the omnibus test results did not meet requirements for moderation, a closer examination of the betas across the two models indicated some evidence of moderation. The elevated ANS response group yielded significant findings from maternal depressive symptoms to emotional insecurity (β = 0.21, p = 0.04) but maternal depressive symptoms to emotional insecurity was not significant (β = 0.16, p = 0.13) in the group evidencing a lower ANS response (Figure 3).
Figure 2: ANS as a Moderator model demonstrates the mediating effect of emotional insecurity on the relationship between mom and adolescent depressive symptoms. Partial mediation was found such that the main effect was reduced to non-significance when emotional insecurity was added to the model. (as indicated by the coefficients listed respectively). Error variances on dependent variables are estimated but not represented here. * indicates significant pathways at p < 0.05; N = 100 participants.
Figure 3: Negative Affect as a Moderator This model demonstrates the multiple group analysis of individuals with higher ANS response (represented by first number) and individuals with no elevated ANS response (represented by second number) when groups are allowed to differ. Error variances on dependent variables are estimated but not represented here. * indicates pathway is significant at p < 0.05. N = 100 participants.
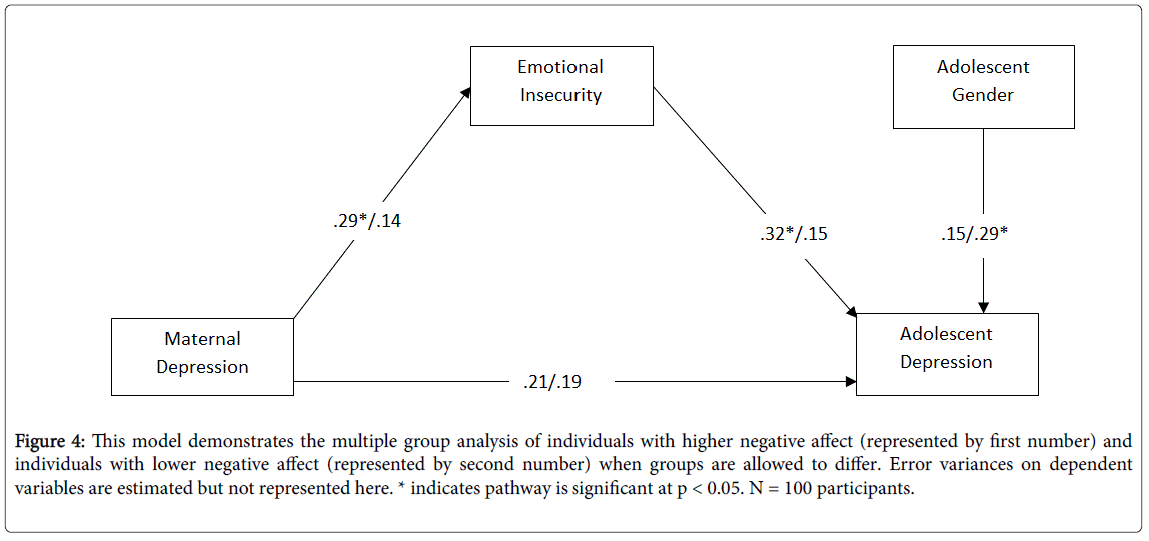
Negative affect: Results from the group difference test indicated that there was a trend level of significant change in chi-square when the paths were allowed to differ for those high in negative affect and those low in negative affect, Δχ2 = 8.62, df = 4, p = 0.07. Critical ratios indicated that the structural pathways from maternal depressive symptoms to emotional insecurity for higher negative affect individuals yielded a significant critical ratio indicating differences across groups. Specifically, for participants who evidenced higher negative affect, maternal depressive symptoms were correlated with emotional insecurity (β = 0.29, p = 0.01) but for participants who evidenced lower negative affect, maternal depressive symptoms were not correlated with emotional insecurity (β = 0.14, p = 0.16). Confidence intervals are presented in Table 2. These results suggest that evidencing higher negative affect in stressful situations may act as a vulnerability that exacerbates the impact of maternal depression on emotional insecurity (Figure 4).
| Higher ANS | 95% CI | Lower ANS | 95% CI | |||
|---|---|---|---|---|---|---|
| Effect (standardized path) | Parameter | Lower | Upper | Parameter | Lower | Upper |
| Direct Effect of Maternal Depression Symptoms on Adolescent Depressive Symptoms | 0.1 | 0.001 | 0.39 | .28* | 0.001 | 0.38 |
| Direct Effect of Adolescent Gender on Adolescent Depressive Symptoms | 0.32* | 0.02 | 0.41 | 0.13 | -0.003 | 0.57 |
| Direct Effect of Maternal Depressive Symptoms on Adolescent Emotional Security | 0.21* | 0.02 | 0.4 | 0.16 | 0.01 | 0.37 |
| Direct Effect of Adolescent Emotional Security on Adolescent Depressive Symptoms | 0.24* | 0.06 | 0.48 | 0.24 | 0.02 | 0.38 |
| Indirect Effect of Maternal Depression Symptoms on Adolescent Depressive Symptoms | 0.09 | 0.01 | 0.14 | 0.03 | 0.002 | 0.13 |
| Higher NA | 95% CI | Lower NA | 95% CI | |||
| Effect (standardized path) | Parameter | Lower | Upper | Parameter | Lower | Upper |
| Direct Effect of Maternal Depression Symptoms on Adolescent Depressive Symptoms | 0.21 | -0.1 | 0.54 | 0.19 | -0.08 | 0.44 |
| Direct Effect of Adolescent Gender on Adolescent Depressive Symptoms | 0.15 | -0.19 | 0.56 | 0.29* | 0.07 | 0.49 |
| Direct Effect of Maternal Depressive Symptoms on Adolescent Emotional Security | 0.29* | 0.1 | 0.49 | 0.14 | 0.06 | 0.34 |
| Direct Effect of Adolescent Emotional Security on Adolescent Depressive Symptoms | 0.32* | 0.01 | 0.5 | 0.15 | 0.06 | 0.33 |
| Indirect Effect of Maternal Depression ymptoms on Adolescent Depressive Symptoms | 0.1 | 0.01 | 0.19 | 0.02 | 0.02 | 0.06 |
N Parameter values represent standardized regression weights. Confidence intervals were obtained from Bootstrapping in AMOS. *Indicates that the direct effect was significant at p < 0.05.
Table 2: Betas and confidence intervals for moderating models.
Figure 4: This model demonstrates the multiple group analysis of individuals with higher negative affect (represented by first number) and individuals with lower negative affect (represented by second number) when groups are allowed to differ. Error variances on dependent variables are estimated but not represented here. * indicates pathway is significant at p < 0.05. N = 100 participants.
Discussion
Findings from this study support that maternal depressive symptoms are correlated with adolescent depressive symptoms. Additionally, results support mediation such that higher reports of emotional insecurity in the maternal-adolescent relationship may explain the transmission of depressive symptoms from mother to adolescent. These findings are consistent with past research suggesting that adolescence is a critical period for developing a sense of emotional security and add to the literature by documenting the important role that emotional security may have in depressive affect.
Findings from our study partially support that a higher ANS response and a higher negative affect response in adolescents may exacerbate the pathway through which depression is transmitted from mothers to adolescents. Multiple group analyses indicated that individuals with a higher ANS response were more vulnerable for the transmission of depressive symptoms through emotional insecurity than individuals with a lower ANS response. Specifically, we see that the pathway from maternal depressive symptoms to emotional security differs across the groups but do not see the entire mediation pathway moderated by stress response. This may suggest that adolescents’ stress response affects how they interpret their depressed mother’s lack of warmth such that the more stressed the adolescent is, the more likely they are to feel emotionally insecure in their relationship with their mother. Our findings also support the diathesis-stress model [16] and the theory of biological sensitivity to context [7] by suggesting that individuals who have a predisposed vulnerability to stress are more sensitive to contextual influences impacting adjustment. Unfortunately, we could not fully evaluate the theory of biological sensitivity to context because we did not examine if stress reactivity in youth may be helpful in more positive contexts.
In terms of our negative affect model, individuals with a higher negative affect were more vulnerable to the transmission of depressive symptoms through emotional insecurity. These findings are consistent with previous research examining emotional insecurity and children with negative emotions [11,39]. Children that report higher negative affect may have a difficult time coping with their negative emotions as a result of interactions with a mother exhibiting depressive symptoms. Children that have a difficult time managing negative emotions are more likely to develop emotional insecurity and thus are at an elevated risk for depressive symptoms. It is interesting to note that we find more pronounced differences across groups when we consider stress response as indicated by self-report as opposed to physiological indicators. It is possible that negative affect may be a better indicator in the transmission of depressive symptoms through emotional insecurity. Limited research has been conducted in this area but some research indicates that adolescents’ negative affect does play a role in the transmission of depressive symptoms [40,41]. It is important to note that adolescents who scored high in self-report of negative affect and adolescents who scored high in ANS stress reactivity were composed of different groups of youth and thus these differences across groups may also be due to differences in those participants not accounted for in the models. Future research should continue to examine differences in self-report and physiological indicators of stress response in larger samples.
Gender was significantly associated with adolescents’ depressive symptoms and this was more pronounced among youth that had a higher ANS response. Waugh et al. [22] study supports this finding with results indicating that girls with a higher stress response and mothers that were more depressed were at risk for developing depressive symptoms, indicating that dysregulation or a higher stress response acts as a vulnerability in the transmission of depressive symptoms, particularly for girls. Interestingly, in our negative affect model, gender seemed to be significantly related to adolescent depressive symptoms in cases of lower negative affect. These findings may be explained by previous research suggesting that children with depressive symptoms are less likely to report negative affect such as aggression or outward distress and are more likely to internalize their emotions [11]. There is also research that supports gender differences in self-report of affect; girls are more likely to report internalizing behaviors of negative affect whereas boys are more likely to report externalizing behaviors of negative affect [42]. Females that are depressed are less likely to report outward distress and are more likely to internalize their emotions which may suggest the lack of negative affect reported by females. However, it is also important to note here that our sample was unbalanced with 68% female.
This study is not without limitations. The sample size was small given the use of multiple group path models and may have contributed to the difficulty in finding significant associations within our mediating and moderating models. There were also potential limitations in how the ANS and negative affect variables were created for our moderating hypothesis. ANS and negative affect variables were dichotomized which may obscure individual differences [43], however, moderation can be difficult to detect when using small samples and continuous variables [44,45]. Furthermore, this study was interested in evaluating differences in the mediational pathway by group, making a multiple group model that can test for moderated mediation a necessity [46-51]. For practical reasons, all three physiological measures measure the ANS response in the body, so combining these measures into one holistic variable gives a better representation of the ANS response rather than running separate models for each indicator of stress. Research supports this method of creating a holistic ANS variable by taking the top 75% of each physiological measure [37].
Our sample also lacked diversity in that the sample was predominately female and upper-middle class. Furthermore, it is important to note that the data collected from this study is correlational, so the direction of effects cannot be determined. In future studies, larger populations should be looked at longitudinally with a more diverse sample. Future studies can also examine the effects of parental psychopathology and marital conflict as contributors to the transmission of depression. These implications can be important in understanding the intergenerational transmission of depressive symptoms and can be used to inform future programs that target adolescents experiencing depressive symptoms, where the quality of attachment and security, as well as how the adolescent copes with stressful situations will be the focus point for intervention.
References
- Insel T (2012) Number of Suicides in 2007: National Institute of Mental Health.
- Hammen C, Brennan PA, Le Brocque R (2011) Youth depression and early childrearing: stress generation and intergenerational transmission of depression. J Consult Clin Psychol 79: 353-363.
- Nelson DR, Hammen C, Brennan PA, Ullman JB (2003) The impact of maternal depression on adolescent adjustment: the role of expressed emotion. J Consult Clin Psychol 71: 935-944.
- Teti DM, Gelfand DM, Messinger DS, Isabella R (1995) Maternal Depression and the Quality of Early Attachment: an examination of infants, preschoolers, and their mothers. Developmental Psychology 31: 364-376.
- Forman EM, Davies PT (2003) Family Instability and Young Adolescent adjustment: the mediating effects of parenting quality and adolescent appraisals of family security. Journal of Clinical Child and Adolescent Psychology 32: 94-105.
- Milan S, Snow S, Belay S (2009) Depressive symptoms in mothers and children: preschool attachment as a moderator of risk. Dev Psychol 45: 1019-1033.
- Ellis BJ, Boyce T (2008) Biological Sensitivity to Context. Current Directions in Psychological Science 17: 183-187.
- Cummings EM, Keller PS, Davies PT (2005) Towards a family process model of maternal and paternal depressive symptoms: exploring multiple relations with child and family functioning. Journal of Child Psychology and Psychiatry 46: 479-489.
- Muñoz RF, Beardslee WR, Leykin Y (2012) Major depression can be prevented. Am Psychol 67: 285-295.
- Robila M, Krishnakumar A (2006) The Impact of Maternal Depression and Parenting Behaviors on Adolescents’ Psychological Functioning in Romania. Journal of Child and Family Studies 15: 71-82.
- Davies PT, Cummings EM (1994) Marital conflict and child adjustment: an emotional security hypothesis. Psychol Bull 116: 387-411.
- Forehand R, Brody G, Slotkin J, Fauber R, McCombs A, et al. (1988) Young Adolescent and Maternal Depression: assessment, interrelations, and family predictors. Journal of Consulting and Clinical Psychology 56: 422-426.
- Davies PT, Sturge-Apple ML, Cicchetti D, Cummings EM (2007) The Role of Child Adrenocortical Functioning in Pathways Between Interparental Conflict and Child Maladjustment. Developmental Psychology 43: 918-930.
- Ebesutani C, Kim E, Young J (2014) The role of violence exposure and negative affect in understanding child and adolescent aggression. Child Psychiatry Hum Dev 45: 736-745.
- Schilling OK, Diehl M2 (2014) Reactivity to stressor pile-up in adulthood: effects on daily negative and positive affect. Psychol Aging 29: 72-83.
- Ingram RE, Luxton DD (2005) Vulnerability-stress models. Development of Psychopathology: A Vulnerable-Stress Perspective pp: 32-46.
- Lupien SJ, McEwen BS, Gunnar MR, Heim C (2009) Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat Rev Neurosci 10: 434-445.
- Compas BE, Orosan PG, Grant KE (1993) Adolescent stress and coping: implications for psychopathology during adolescence. J Adolesc 16: 331-349.
- Obradovic J, Bush NR, Stamperdahl J, Adler NE, Boyce WT (2010) Biological Sensitivity to Context: the interactive effects of stress reactivity and family adversity on socioemotional behavior and school readiness. Child Development 81: 270-289.
- ObradoviÄ J, Bush NR, Boyce WT (2011) The interactive effect of marital conflict and stress reactivity on externalizing and internalizing symptoms: the role of laboratory stressors. Dev Psychopathol 23: 101-114.
- Lewinsohn PM, Joiner TE Jr, Rohde P (2001) Evaluation of cognitive diathesis-stress models in predicting major depressive disorder in adolescents. J Abnorm Psychol 110: 203-215.
- Waugh CE, Muhtadie L, Thompson RJ, Joormann J, Gotlib IH (2012) Affective and physiological responses to stress in girls at elevated risk for depression. Dev Psychopathol 24: 661-675.
- US Bureau of the Census S (1901) Income in the past 12 months, 2013 American Community Survey 1-Year Estimates.
- Robin AL, Foster S (1989) Negotiating parent-adolescent conflict. New York: Guilford Press.
- Radloff LS (1977) The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement 1: 385-401.
- Sternberg KJ, Lamb ME, Guterman E, Abbott CB, Dawud-Noursi S (2005) Adolescents' perceptions of attachments to their mothers and fathers in families with histories of domestic violence: a longitudinal perspective. Child Abuse Negl 29: 853-869.
- Cook EC, Fletcher AC2 (2012) A Process Model of Parenting and Adolescents' Friendship Competence. Soc Dev 21: 461-481.
- El-Sheikh M, Elmore-Staton L (2004) The link between marital conflict and child adjustment: parent-child conflict and perceived attachments as mediators, potentiators, and mitigators of risk. Dev Psychopathol 16: 631-648.
- Duan B (1999) The robustness of trimming and Winsorization when the population distribution is skewed. Dissertation Abstracts International 59: 4907.
- Calkins SD, Graziano PA, Keane SP (2007) Cardiac vagal regulation differentiates among children at risk for behavior problems. Biol Psychol 74: 144-153.
- Achenbach TM (1991b) Manual for the Child Behavior Checklist/418 and 1991 Profile. Burlington, VT: University of Vermont Department of Psychiatry.
- Byrne BM (2001) Structural equation modeling with AMOS: Basic concepts, applications, and programming. Mahwah, NJ: Lawrence Erlbaum Associates.
- Iacobucci D (2009) Structural equations modeling: Fit Indices, sample size, and advanced topics. Journal of Consumer Psychology 20: 90-98.
- Thompson B (2000) Ten commandments of structural equation modeling reading and Understanding more multivariate statistics. Washington, DC: American Psychological Association pp: 261-285.
- Lin T (2013) Effects of Gender and Game Type on Autonomic Nervous System Physiological Parameters in Long-Hour Online Game Players, Cyberpsychology, Behavior, and Social Networking 16: 820-827.
- Ellis BJ, Essex MJ, Boyce WT (2005) Biological sensitivity to context: II. Empirical explorations of an evolutionary-developmental theory. Dev Psychopathol 17: 303-328.
- Goldman N, Glei DA, Seplaki C, Liu IW, Weinstein M (2005) Perceived stress and physiological dysregulation in older adults. Stress 8: 95-105.
- Byrne BM (2013) Structural Equation Modeling with AMOS: Basic concepts, applications and programming, (2nd edn). Hoboken: Taylor and Francis.
- Eisenberg N, Fabes RA, Murphy BC (1996) Parents' reactions to children's negative emotions: relations to children's social competence and comforting behavior. Child Dev 67: 2227-2247.
- Luebbe AM, Fussner LM, Kiel EJ, Early MC, Bell DJ (2013) Role of adolescent and maternal depressive symptoms on transactional emotion recognition: context and state affect matter. Emotion 13: 1160-1172.
- Riskind JH, Kleiman EM, Schafer KE (2013) “Undoing†Effects of Positive Affect: does it buffer the effects of negative affect in predicting changes in depression? Journal of Social and Clinical Psychology 32: 363-380.
- Fujita F, Diener E, Sandvik E (1991) Gender differences in negative affect and well-being: the case for emotional intensity. J Pers Soc Psychol 61: 427-434.
- Kline RB (2009) Becoming A Behavioral Science Researcher: A Guide to Producing Research That Matters. The Guildford Press.
- Champoux JE, Peters WS (1987) Form, effect size and power in moderated regression analysis. Journal of Occupational Psychology 60: 243-255.
- Fan X, Thompson B, Wang L (1999) Effects of sample size, estimation methods, and model specification on structural equation modeling fit indexes. Structural Equation Modeling 6: 56-83.
- Little TD, Card NA, Bovaird JA, Preacher KJ, Crandall CS (2007) Structural Equation Modeling of Mediation and Moderation With Contextual Factors. Modeling contextual effects in longitudinal studies 1: 207-230.
- Preacher KJ, Rucker DD, Hayes AF (2007) Addressing Moderated Mediation Hypothesis: Theory, Methods, and Prescriptions. Multivariate Behavioral Research, 42: 185-227.
- Alegre A, Benson MJ, Perez-Escoda N (2014) Maternal Warmth and Early Adolescents’ Internalizing Symptoms and Externalizing Behavior: mediation via emotional insecurity. Journal of Early Adolescence 34: 712-735.
- Allen JP, Hauser ST, Eickholt C, Bell KL, O’Conner TG (1994) Autonomy and Relatedness in Family Interactions as Predictors of Expressions of Negative Adolescent Affect. Journal of Research on Adolescence 4: 535-552.
- American Psychiatric Association (2013) Diagnostic and statistical manual of mental health disorders: DSM-5 (5th edn.) Washington, D.C.: American Psychiatric Publishing.
- Cummings EM, Davies PT (1994) Maternal depression and child development. J Child Psychol Psychiatry 35: 73-112.
Citation: Wilkinson K and Cook E (2016) Stress Response and Emotional Security in the Intergenerational Transmission of Depressive Symptoms. J Child Adolesc Behav 4: 283. DOI: 10.4172/2375-4494.1000283
Copyright: © 2016 Wilkinson K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 13085
- [From(publication date): 2-2016 - Nov 25, 2024]
- Breakdown by view type
- HTML page views: 12272
- PDF downloads: 813