Stress Evaluation for the Prevention of Karoshi
Received: 09-Dec-2016 / Accepted Date: 28-Dec-2016 / Published Date: 31-Dec-2016 DOI: 10.4172/2329-6879.1000257
55728Karoshi in Japan
Recently, the tragic news of the suicide of a young woman who worked at an advertising giant company was widely reported in Japan. She was just 24 years old when she killed herself December 2015, and the death was ruled as death by "karoshi," after the woman was found to have logged around 105 hours of monthly overtime.
The first case of karoshi was reported in 1969 with the death from a stroke of a 29 year-old, male worker in the shipping department of Japan’s largest newspaper company. White paper on Karoshi published from the Health, Labor and Welfare Ministry of Japan mentions that compensation for work-related deaths caused by stroke or cardiovascular disease has increased in our country reporting 58 compensated case related to karoshi in 2001 and 121 in 2014, respectively; however, these cases seem to represent just the tip of the iceberg. As typical cases, a worker of a major snack food processing company for as long as 110 hours a week and died from heart attack at the age of 34. A 22-year-old nurse died from a heart attack after continuous 34 hours’ duty five times a month.
Karoshi, the term for death from overwork, also encompasses suicide related to overwork and is an extreme outcome of cardiovascular and cerebrovascular diseases. Stroke and cardiovascular diseases associated with overwork are extremely rare in Europe, Scandinavian nations, and the US because of very strict labor regulation. However, many deaths related to excessive occupational stress still occur in Japan despite the widespread recognition of the problem in the 1980s. White paper on karoshi says that 94.8% of compensation cases for work-related deaths caused by stroke or cardiovascular disease were associated with overtime work more than 80 hours every month.
Although the term karoshi originates in Japan, other Asian countries like China or Korea are also affected by it. Common issues for workers in these countries are prioritization of work over family, relatively long working hours, and a poor work-life balance. Kivimäki et al. demonstrated that employees working for long hours have a higher risk of stroke than those working standard hours [1]. Cases of karoshi are not only tragedy for the bereaved families, but also a serious loss for society. Karoshi is therefore a pressing societal issue in Japan, and its prevention is the responsibility of not only occupational health doctors but all physicians.
Several problems regarding with Japan’s work environment have been highlighted since the recognition of karoshi as a major societal problem in Japan from the 1980s. Historically, hard work and diligence have been considered necessary for rebuilding of Japan as it emerged from the devastation of World War II. These attributes are also thought of as characteristics of the work ethic of Japanese people, underlying the robust state of its workforce. In 1970, the Pakistan Foreign Minister Bhutto criticized the dedication and attitude of Japanese people for the pursuit of economic profit referring to them as “economic animal”. Although the workplace environment has been improved since then, recent news reports of "black enterprises" revealed that serious problems in the work environment remain prevalent in Japan.
Various national strategies have been implemented to prevent karoshi in Japan. The Industrial Safety and Health Act was revised in April 2006. This law mandates a medical interview and physician consultations for employees who work long hours. Nevertheless, despite these measures, karoshi has not been eradicated. A United Nations committee provided recommendations for preventing overwork to the Japanese government in 2013. In response, the Karoshi Prevention Council of the Ministry of Health, Labor and Welfare of Japan recently released a basic policy, which has set a goal of decreasing the percentage of people working 60 hours or more per week to less than 5% of the population by 2020. In addition, a mandatory stress check system was initiated at the end of 2015. This stress check system includes an evaluation of the stress status of workers and the provision to workers of the results. Results will be analyzed in each workplace to enable the identification of the stressors, thereby leading to improvements in the work environment. These comprehensive approaches might decrease the number of cases of karoshi and hopefully eliminate it in the future.
Karoshi and Psychological and Occupational Stresses
Cerebrovascular or cardiovascular diseases responsible for karoshi include intra-cerebral hemorrhage, subarachnoid hemorrhage, cerebral infarction, hypertensive encephalopathy, myocardial infarction, angina pectoris, cardiac arrest including sudden cardiac death, and dissecting aortic aneurysms. Although lifestyle factors are involved in the pathogenesis of these diseases, occupational stress is considered the major cause in cases of karoshi. Oxidative stress and psychological stresses are also involved in the development of cerebrovascular and cardiovascular diseases.
Growing evidences indicate that depression is closely associated with atherosclerotic cardiovascular disease. For example, a metaanalysis including 11 studies to investigate the impact of depression on the development of coronary heart disease in subjects who were healthy at baseline shows that the overall relative risk of coronary heart disease in subjects with depression was 1.64 [2]. Furthermore, depression exerts a significantly negative impact on the prognosis of patients with coronary artery disease [3]. These investigations clearly demonstrated that depression is a pivotal factor linking occupational stress and karoshi.
There are several methods to evaluate the extent of occupational stress, including the effort-reward imbalance model and the demandcontrol model. Regarding the demand-control model, the job content questionnaire (JCQ) developed by Karasek is one of the most commonly used scales to assess environmental job stressors [4]. Occupational stress can be measured by qualitative constructs such as job control, job demands and worksite social support. Job strain refers to a situation where job control, which is a person’s ability to make decisions and use his or her skills at work, is low and the job demands, which include the pace and psychological intensity of the work, are high. The job strain index measured by the ratio of job demands to job control was used as an indicator of the occupational stress.
Recently, the relationship between occupational and psychological stresses in outpatients with lifestyle-related diseases was examined [5]. In our recent investigation, the job strain index by the JCQ was used as an indicator of the occupational stress, and depression was evaluated by the Self-Rating Depression Scale (SDS).
We demonstrated that a univariate linear regression analysis showed that the SDS scores were positively correlated with job demands and the job strain index and negatively correlated with job control and worksite social support [5].
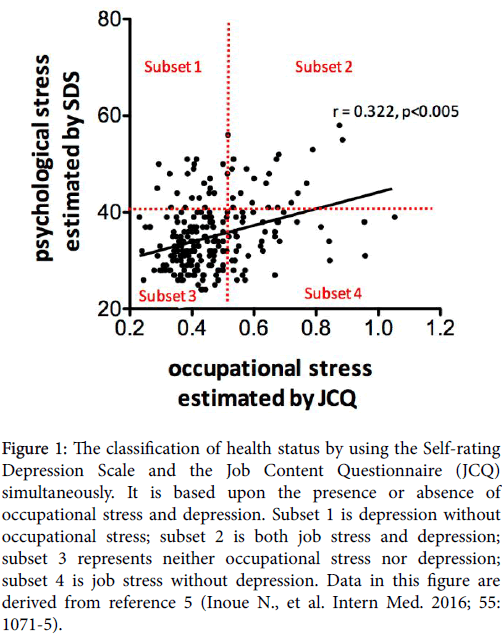
Multiple regression analyses to predict SDS scores demonstrated that job demands were positively associated with SDS scores and job control and worksite social support were negatively associated with SDS scores after controlling for other variables. The job strain index was positively related to SDS scores (Figure 1).
Figure 1: The classification of health status by using the Self-rating Depression Scale and the Job Content Questionnaire (JCQ) simultaneously. It is based upon the presence or absence of occupational stress and depression. Subset 1 is depression without occupational stress; subset 2 is both job stress and depression; subset 3 represents neither occupational stress nor depression; subset 4 is job stress without depression. Data in this figure are derived from reference 5 (Inoue N., et al. Intern Med. 2016; 55: 1071-5).
These findings confirm that the occupational stress is closely related to depression. Our research is a cross-sectional study, and thus provides no information regarding the causal relationship between depression and occupational stress. We speculate that the occupational stress leads to depression.
Alternatively, depression may also leads to inefficient work, which may induce greater self-evaluated job stress. Taken together, these findings suggest the possible existence of a vicious cycle consisting of the occupational stress and depression might exist.
On the basis of our results, we propose a classification system of occupational stress and depression by simultaneously using the SDS and JCQ. As shown in the Figure 1, all subjects were divided into four subsets by defining subjects with SDS scores over 40 points as depressed, and those with a job strain index over 0.50 were defined as having occupational stress.
This classification is based on the presence or absence of occupational stress and depression. Subset 1 consists of subjects with depression but no occupational stress, subset 2 consists of subjects with both occupational stress and depression, subset 3 consists of those with neither occupational stress nor depression, and subset 4 consists of subjects with occupational stress, but without depression.
The depression experienced by subjects in the subset 2 is likely to be caused by excessive occupational stress whereas the subjects in subset 1 might suffer from stressors other than occupational stress, such as those arising from family matters or personal reasons.
The subjects in the subset 4 might be doing well because they are able to cope with occupational stress. Thus, this classification system could contribute to promoting a healthy workplace and serve as a detailed guide for individual workers.
Karoshi and Oxidative Stress
The pathogenesis of cerebrovascular and cardiovascular diseases is complex and is related to atherosclerosis. Previous research–both clinical and experimental–has indicated that all traditional risk factors for atherosclerosis including diabetes, hyperlipidemia, hypertension and smoking, induce oxidative stress in the vasculature.
Previously, we demonstrated the enhanced production of reactive oxygen species (ROS) in atherosclerotic coronary arteries of patients with coronary artery diseases [6]. Oxidative stress is implicated in the formation of atherosclerotic vascular diseases via various processes. Under enhanced oxidative stress, low-density lipoprotein (LDL) is oxidatively modified.
The formed oxidized LDL induces various biological activities that are related to atherosclerotic processes including endothelial dysfunction, promotion of the proliferation of vascular smooth muscle cells, and induction of the expression of adhesion molecules and chemokines [7,8]. Because atherosclerosis-based cardiovascular and cerebrovascular diseases underlie karoshi, oxidative stress is one of the contributors to this problem.
LOX-index, a novel biomarker for cardiovascular disease and stroke from a view point of oxidative stress
The pathophysiological effects of oxidized LDL are mainly mediated via the lectin-like oxidized low-density lipoprotein receptor-1 (LOX-1) [9]. LOX-1 was identified as the receptor for oxidized LDL (oxLDL) on endothelial cells. LOX-1 expressed on the cell surface can be proteolytically cleaved by an undetermined enzymatic system in the membrane-proximal extracellular domain and released into the bloodstream as a soluble form [10,11].
Recently, we reported the significance of LOX-index, which is calculated by multiplying the level of the LOX-1 ligands containing apo-lipoprotein B (LAB) and soluble LOX-1 (sLOX-1) as a predictive marker for stroke and cardiovascular disease. Data from the Suita cohort study revealed that a higher LOX-index was associated with an increased risk of cardiovascular diseases and stroke [12].
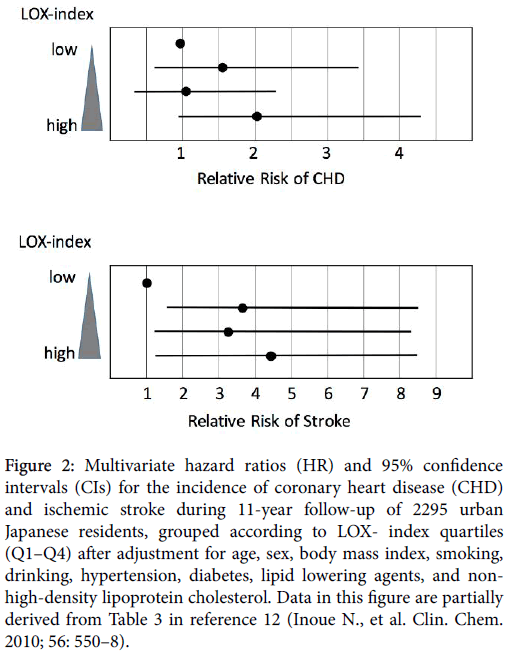
It has been reported that the multivariable-adjusted hazard ratio for ischemic stroke and myocardial infarction from the second to top quartile of LOX-index was three-fold and two-fold higher, respectively, than that for the bottom quartile after multivariable adjustment in a community-based cohort study (Figure 2).
Figure 2: Multivariate hazard ratios (HR) and 95% confidence intervals (CIs) for the incidence of coronary heart disease (CHD) and ischemic stroke during 11-year follow-up of 2295 urban Japanese residents, grouped according to LOX- index quartiles (Q1–Q4) after adjustment for age, sex, body mass index, smoking, drinking, hypertension, diabetes, lipid lowering agents, and nonhigh- density lipoprotein cholesterol. Data in this figure are partially derived from Table 3 in reference 12 (Inoue N., et al. Clin. Chem. 2010; 56: 550–8).
Thus, the LOX-index might be a novel predictive marker for these diseases from the standpoint of oxidative stress.
Relationship of Oxidative stress and Psychological Stress
There is some evidence indicating the interaction of psychological and oxidative stresses. For example, depressive symptoms have been correlated with lipid peroxidation in human blood [13].
Andersson et al. investigated the effects of psychological stress on LOX-1 expression in rats [14]. Psychological stress upregulated LOX-1 levels in the vessel walls through the formation of ROS. Their experimental observations suggested the possibility that LOX-1 might be a key molecule that links oxidative stress and mental stress.
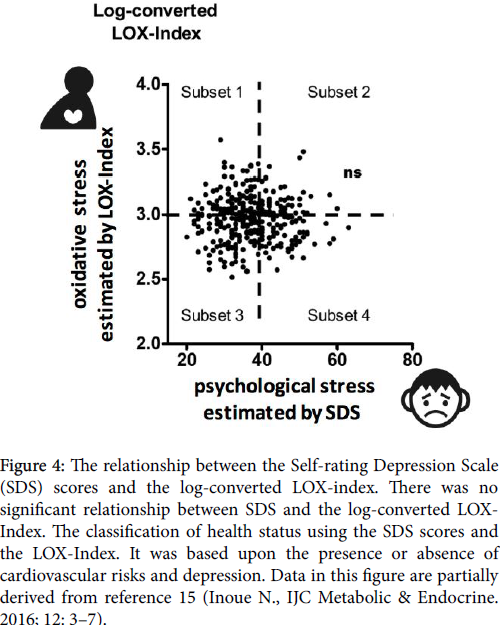
Considering this close relationship of LOX-1 with stress, the relationship between the LOX-index and psychological stress was evaluated in 331 consecutive outpatients with lifestyle-related diseases such as diabetes, hyperlipidemia, and hypertension [15]. The results showed no significant association between the LOX-index and SDS sores in outpatients with lifestyle-related diseases as shown in Figure 3.
However, a simultaneous evaluation of the LOX-index and SDS could be used to classify the subjects on the basis of two different aspects - oxidative and psychological stresses. The subjects with SDS scores over 40 points were defined as being depressed and those with the log-converted LOX-index over 3.0 were defined as having cardiovascular risk because of oxidative stress according to the previous investigation.
Therefore, all subjects were divided into four subsets as shown in Figure 4. This classification is based on the presence or absence of depression and oxidative stress. Subset 1 consisted of subjects with oxidative stress but without psychological stress; subset 2 consisted of subjects with oxidative stress and psychological stress; subset 3 consisted of subjects with neither oxidative stress nor psychological stress; and subset 4 consisted of subjects with psychological stress but without oxidative stress.
Figure 4: The relationship between the Self-rating Depression Scale (SDS) scores and the log-converted LOX-index. There was no significant relationship between SDS and the log-converted LOXIndex. The classification of health status using the SDS scores and the LOX-Index. It was based upon the presence or absence of cardiovascular risks and depression. Data in this figure are partially derived from reference 15 (Inoue N., IJC Metabolic & Endocrine. 2016; 12: 3–7).
Subjects in subsets 2 and 4 may need psychosocial intervention whereas a lifestyle modification program is likely necessary in those in the subsets 1 and 2. Thus, this classification system could contribute to the risk evaluation for cardiovascular diseases and could help guide individual subjects.
Multifaceted approach for the Prevention of Karoshi
The workplace environment is rapidly changing because of various factors such as the globalization of economic activity and technological innovation. However, the prolonged economic downturn has prompted corporate restructuring and pushed workers into early retirement. Furthermore, information technology has reshaped the society. Computer-based working places that require long sitting times alleviate physical burden, but adversely affect mental health.
On the contrary, a low birthrate and an aging population are the challenges that are confronting many developed countries, including the United States and Japan. The population of Japan in particular is aging at an unprecedented rate. Therefore, the overburden on the working population has markedly increased in this country. Furthermore, the Japanese lifestyle including dietary habits has been changing for the last few decades. The traditional Japanese diet containing vegetables, seafood, soy, clear broth, rice, green tea and seaweed, is originally healthy and well balanced.
However, the recent replacement of these natural fresh foods with unhealthy fast food has adversely affected rates of cardiovascular disease occurrence. These lifestyle alterations might enhance the oxidative stress.
Because the circumstances at workplace are worsening, the prevention of karoshi is an urgent issue that should be addressed by Japanese society as a whole. The most crucial issue in the prevention of karoshi is the improvement in work environment including the adjustment of working hours, reduction of occupational stress, and enhancement of welfare programs and social support. Furthermore, lifestyle-related diseases such as hypertension, dyslipidemia, and diabetes are closely associated with the pathogenesis of cerebrovascular and cardiovascular diseases, which are responsible for karoshi.
Therefore, the management of lifestyle-related diseases is also crucial for the prevention of karoshi. Because the LOX-index is a marker of these diseases, it might be useful in risk stratification of these diseases. Furthermore, as described above, a simultaneous evaluation of psychological and occupational stresses could help identify stressed and overburdened employees who are at a high risk for karoshi.
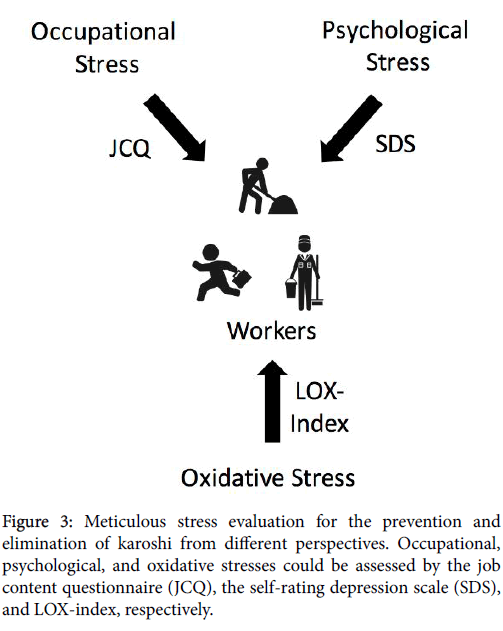
Thus, all workers should undergo meticulous stress evaluation from the perspectives of preventing and eliminating karoshi (Figure 3). More importantly, prospective studies are needed to assess whether workload reduction and improvements in social environment and lifestyle might improve the results indicated by these markers including LOX-Index, SDS, and JCQ.
References
- Kivimäki M, Jokela M, Nyberg, ST, Singh-Manoux A, Fransson EI, et al. (2015) Long working hours and risk of coronary heart disease and stroke: a systematic review and meta-analysis of published and unpublished data for 603,838 individuals. Lancet 386:1739-1746.
- Rugulies R (2002) Depression as a predictor for coronary heart disease. a review and meta-analysis. Am J Prev Med 23:51-61.
- van Melle JP, de Jonge P, Spijkerman TA, Tijssen JG, Ormel J, et al. (2004) Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysis. Psychosom Med 66:814-822.
- Karasek R, Baker D, Marxer F, Ahlbom A, Theorell T (1981) Job decision latitude, job demands, and cardiovascular disease: a prospective study of Swedish men. Am J Public Health 71:694-705.
- Inoue N, Otsui K, Yoshioka T, Suzuki A, Ozawa T, et al. (2016) A simultaneous evaluation of occupational stress and depression in patients with lifestyle-related diseases. Intern Med 55:1071-1075.
- Azumi H, Inoue N, Ohashi Y, Terashima M, Mori T, et al. (2002) Superoxide generation in directional coronary atherectomy specimens of patients with angina pectoris: important role of NAD(P)H oxidase. Arterioscler Thromb Vasc Biol 22:1838-1844.
- Yokoyama M, Hirata K, Miyake R, Akita H, Ishikawa Y, et al. (1990) Lysophosphatidylcholine: essential role in the inhibition of endothelium-dependent vasorelaxation by oxidized low density lipoprotein. Biochem Biophys Res Commun168:301-308.
- Mitra S, Deshmukh A, Sachdeva R, Lu J, Mehta JL (2011) Oxidized low-density lipoprotein and atherosclerosis implications in antioxidant therapy. Am J Med Sci 342:135-142.
- Inoue N, Sawamura T (2007) Lectin-like oxidized LDL receptor-1 as extracellular chaperone receptor: its versatile functions and human diseases. Methods 43:218-222.
- Sawamura T, Kume N, Aoyama T, Moriwaki H, Hoshikawa H, et al. (1997) An endothelial receptor for oxidized low-density lipoprotein. Nature 386:73-77.
- Murase T, Kume N, Kataoka H, Minami M, Sawamura T, et al. (2000) Identification of soluble forms of lectin-like oxidized LDL receptor-1. Arterioscler Thromb Vasc Biol 20:715-720.
- Inoue N, Okamura T, Kokubo Y, Fujita Y, Sato Y, et al. (2010) LOX index, a novel predictive biochemical marker for coronary heart disease and stroke. Clin Chem 56:550-558.
- Forlenza MJ, Miller GE (2006) Increased serum levels of 8-hydroxy-2'-deoxyguanosine in clinical depression. Psychosom Med 68:1-7.
- Andersson IJ, Sankaralingam S, Davidge ST (2010) Restraint stress up-regulates lectin-like oxidized low-density lipoprotein receptor-1 in aorta of apolipoprotein E-deficient mice. Stress 13:454-460.
- Inoue N, Fukuyama K, Hirayama S, Yoshioka T, Ozawa T, et al. (2016) Cardiovascular risk assessment using LOX-index and self-rating depression scale. IJC Metabolic & Endocrine 12: 3-7.
Citation: Inoue N (2016) Stress Evaluation for the Prevention of Karoshi. Occup Med Health Aff 4:257. DOI: 10.4172/2329-6879.1000257
Copyright: © 2016 Inoue N. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 7728
- [From(publication date): 0-2016 - Dec 04, 2024]
- Breakdown by view type
- HTML page views: 6927
- PDF downloads: 801