Strategies to Enhance Colorectal Cancer Symptoms and Risk Factors Awareness
Received: 01-Jul-2023 / Manuscript No. ACP-23-107927 / Editor assigned: 05-Jul-2023 / PreQC No. ACP-23-107927 / Reviewed: 19-Jul-2023 / QC No. ACP-23-107927 / Revised: 24-Jul-2023 / Manuscript No. ACP-23-107927 / Published Date: 31-Jul-2023 DOI: 10.4172/2472-0429.1000171 QI No. / ACP-23-107927
Abstract
The post-colonoscopy colorectal cancers rate of a colonoscopy service determines its efficacy in detecting and preventing cancer and should therefore be considered as the principal measure of quality In colonoscopy, driving performance improvement Within the service
Keywords: Colonoscopy; Health care; Colorectal treatment; Faecal intubation; Colorectal carcinoma; Level of knowledge
Keywords
Colonoscopy; Health care; Colorectal treatment; Faecal intubation; Colorectal carcinoma; Level of knowledge
Introduction
For quality assurance purposes, a Standardized method to calculate an unadjusted post-colonoscopy colorectal cancers Rate may be used to permit the benchmarking of services. This unadjusted post-colonoscopy colorectal cancers rate should be calculated as the Number of post-colonoscopy colorectal cancers divided by the total of the number of Post-colonoscopy colorectal cancers plus the number of detected cancers, expressed as a percentage. The post-colonoscopy colorectal cancers rate is calculated based on the date the person had the colonoscopy, with the term Detected cancer being used to describe cancers diagnosed by the colonoscopy or within 6 months of the date of the colonoscopy, and the term post-colonoscopy colorectal cancers used to describe Cancers beyond 6 months of the date of the colonoscopy [1]. For consistency and to permit benchmarking it was suggested that as a minimum the post-colonoscopy colorectal cancers rate should be reported for an interval of 3 years. Ideally the post-colonoscopy colorectal cancers rate-1y, post-colonoscopy colorectal cancers-5y, and post-colonoscopy colorectal cancers-10y should also be calculated. The calculation of post-colonoscopy colorectal cancers rates is complex and Calculation requires theoretically a collaborative approach within a multidisciplinary health care system, including cancer registries. Here we propose our own data, without Data of official cancer registries [2]. However, we are quite sure about the near completeness of our data: our Hospital is a rather large regional centre with a minimal spontaneous transfer of patients to other hospitals for Colonoscopy and colorectal cancer treatment. Also, we included two patients where index colonoscopy was done in our hospital and post-colonoscopy colorectal cancers diagnosis was made in another hospital. During the 6 years of data collection 807 colorectal Cancers were diagnosed, of which were classified as post-colonoscopy colorectal cancers and 760 as detected cancer.
Methodology
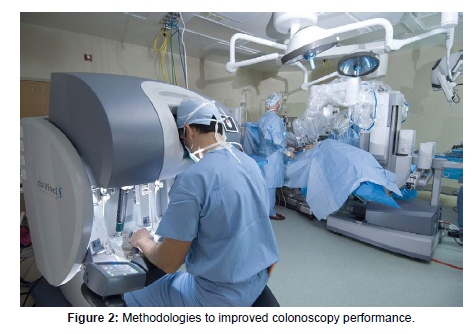
The report of the index colonoscopy was consulted retrospectively. This colonoscopy was completed with faecal intubation in 100% of the examinations. Preparation was mentioned as very bad in 4, Moderate in 6 and good in the remaining 37 Patients [3]. Boston bowel preparation scale was only registered systematically in our ward from 2016 onwards. A polyp or carcinoma was detected at index Colonoscopy in 36 patients, three patients had a malignant lesion and 33 patients had polyps. Four patients had already a colorectal carcinoma in their medical History. In the small proportion of patients were bbps was mentioned during the index colonoscopy, no relation at all could be detected between less prepared segment and location of the tumour during second colonoscopy. After a Positive test a colonoscopy was proposed [4]. However, till Now there is no centralized colonoscopy quality registry in Belgium. Faecal intubation rate, adenoma detection Rate and withdrawal time are traditionally considered as quality measures of colonoscopy. However, the above mentioned parameters are only surrogates of the True outcome that matters most to patients that is a post colonoscopy cancer [5]. The data of our centre are in line with the data in Literature: more right-sided post-colonoscopy colorectal cancers and more msi-Positive and b-raf mutated tumours as shown in (Figure 1). Although the majority of the patients had early stage cancer, Almost 40% of the post-colonoscopy colorectal cancers were advanced. Eighty % of the patients had polyps or a cancer at Index colonoscopy. The average period between index colonoscopy and Post-colonoscopy colorectal cancers was 4.2 years. As demonstrated previously, Intervals between colonoscopies in Belgium are shorter than suggested by guidelines [6]. Although minor differences between European and us guidelines, they agree that in case of a qualitative good bowel preparation and the presence of only small hyperplastic polyps In rectum or sigmoid, surveillance colonoscopy is Recommended after 10 years in the absence of a strong Genetic predisposition. If we proposed surveillance Colonoscopy after 5 years, most post-colonoscopy colorectal cancers would nevertheless be diagnosed earlier then the proposed date. Because 80% of the post-colonoscopy colorectal cancers had neoplastic Lesions at index colonoscopy, the risk of postcolonoscopy colorectal cancers with a Normal colonoscopy is very small [7]. Twenty-five % of the post-colonoscopy colorectal cancers were type b, in which the post-colonoscopy colorectal cancer was diagnosed after the proposed Surveillance interval. The question arises how we can improve the follow-up of proposed surveillance. Our results are similar to previous studies, from which can be concluded that most post-colonoscopy colorectal Cancers are preventable [8]. In our study 68% of all post-colonoscopy colorectal cancers could be explained by procedural factors and 32% by Biology-related factors. Macken calculated the Post-colonoscopy colorectal cancers rate in Belgium for the period 2002-2010, also using the recommendations. The mean postcolonoscopy colorectal cancers rate was 7.4%. Benchmarks need to be set for Minimum acceptable standards and aspirational targets [9]. These benchmarks have not been defined for post-colonoscopy colorectal cancers-3y Rates. In an English cohort study the 25% centile from the Range of unadjusted post-colonoscopy colorectal cancers-3y was 5.5%. A minimum Standard of up to 5.5% and an aspirational target of up to 3.6% could be applied as quality standards. The Mean post-colonoscopy colorectal cancers-3y of our department was 2.46%. A limitation of our study is that no direct statistical comparison could be made between the 47 identified Post-colonoscopy colorectal cancers and the other 760 detected cancers [10]. Withdrawal Time and bowel cleansing using the bbps score were not systematically registered. It is also nearly impossible, if there is no link with cancer registries and registrations of colonoscopies, to identify all post-colonoscopy colorectal cancers cases and to notify The service where the index colonoscopy was performed. There are opportunities for improved colonoscopy Performance, for using cancer appearing after a negative Colonoscopy as an important benchmark for quality, And for standardizing methodologies to allow more Direct comparisons between services as shown in (Figure 2).
Discussion
The post-colonoscopy colorectal cancers-3y, as proposed in the consensus statements, is probably a good quality indicator. However to implement this and make comparison between services possible with reliable data, a national colonoscopy registry is necessary [11]. Nearly seven years after the start of the colorectal Screening program, it is time for the implementation of such a colonoscopy registry. The respondent recall of symptoms and risk Factors was found to be quite variable among the Reviewed studies. For example, in the study conducted by gimeno-garcia, rectal bleeding as Warning sign, and low fibre diet as a risk factor were most frequently reported. Our present study found that changes in bowel habits and family history were most often reported [12]. Our present study also found that 13% of the sample recalled lack of physical Activity as a factor which is a remarkable contrast when compared with 47% of respondents who identified this as a factor, in a study by sessa and colleagues in 2008. Furthermore, more similar to the findings in sessa was the Fact that 20% of the sample in our study recalled high fat Intake as a risk factor for colorectal cancer compared with the 24% Identified by sessa. The findings from our study revealed that there was an association between gender and family history linked to a better level of knowledge [13]. Additionally, Participants with a history of colorectal cancer had a higher score of the level of knowledge in the current study. Females had better knowledge than males although the disease affects Men more than women. Previous studies reported similar Findings. Although participants with a higher education scored higher than other groups, in our study knowledge is still considered low, and the Difference in education was not statistically significant [14]. In Contrast, several studies reported a statistically significant association between the level of education and awareness of colorectal cancer symptoms and risk factors. Furthermore, our study found that participants above age forty-six had better knowledge compared with other Age groups. This finding was consistent with the results of another study conducted in Jordon with 600 participants, and also a study in Iran with 1,557 participants. One study in the United States of America found that the 20 to 29 years old were less likely to know the relationship between Family, history, diet and colorectal cancer. In conclusion, our present study focused only on the Knowledge regarding symptoms and risk factors. However, it is vital to further explore through additional Research the barriers, facilitators, and the willingness to participate in colorectal cancer screening among the general public. To determine the actual barriers and facilitators will allow for the development of strategies that will inform a range of professional healthcare workers of ways to encourage Individuals at risk to participate in a screening program. Furthermore, the findings from this study represent a solid foundation for the policymakers and educators to direct their efforts firmly toward the establishment of Preventive measures and disease early detection strategies.
Conclusion
In conclusion, there is a need for educational initiatives and awareness campaigns to enhance the general public’s Awareness of colorectal cancer symptoms and risk factors in the Kingdom of Bahrain. Findings from the literature revealed that a lack of knowledge concerning the risk factors and the recognition of the early symptoms influenced the participation in screening programs, and late disease diagnosis. As such, awareness of the disease contributes positively to the participation in the screening programs.
Acknowledgement
None
Conflict of Interest
None
References
- Saarinen R (2006) Weakness of will in the Renaissance and the Reformation. OSO UK : 29-257
- Rovner MH (2005) Likely consequences of increased patient choice. HealthExpect US8: 1-3.
- Marc EL, Chris B, Arul C, David F, Adrian H, et al. (2005) Consensus statement: Expedition Inspiration 2004 Breast Cancer Symposium : Breast Cancer – the Development and Validation of New Therapeutics. Breast Cancer Res Treat EU 90: 1-3.
- Casamayou MH (2001) The politics of breast cancer. GUP US: 1-208.
- Baralt L,Weitz TA (2012) The Komen–planned parenthood controversy: Bringing the politics of breast cancer advocacy to the forefront. WHI EU 22: 509-512.
- Kline KN (1999) Reading and Reforming Breast Self-Examination Discourse: Claiming Missed Opportunities for Empowerment, J Health Commun UK: 119-141.
- Keller C (1994) The Breast, the Apocalypse, and the Colonial Journey.J Fem Stud Relig USA 10: 53-72.
- Hamashima C, Shibuya D, Yamazaki H, Inoue K, Fukao A, et al. (2008) The Japanese guidelines for gastric cancer screening. Jpn J Clin Oncol UK 38:259-267.
- Sabatino SA, White MC, Thompson TD (2015) Cancer screening test use: United States, 2013. MMWR US 64:464-468.
- Brawley OW, Kramer BS (2005) Cancer screening in theory and in practice. J Clin Oncol US 23:293-300.
- Warner E (2011) Breast-cancer screening. N Engl J Med US 365: 1025-1032.
- Berwick DM (1998) Developing and Testing Changes in Delivery of Care. Ann Intern Med US 128: 651-656.
- Connor BO (2000) Conceptions of the body in complementary and alternative medicine. Routledge UK: 1-279.
- Lynch K (2019) The Man within the Breast and the Kingdom of Apollo. Society 56: 550-554.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Sepulveda I (2023) Strategies to Enhance Colorectal Cancer Symptomsand Risk Factors Awareness. Adv Cancer Prev 7: 171. DOI: 10.4172/2472-0429.1000171
Copyright: © 2023 Sepulveda I. This is an open-access article distributed underthe terms of the Creative Commons Attribution License, which permits unrestricteduse, distribution, and reproduction in any medium, provided the original author andsource are credited.
Share This Article
Recommended Conferences
42nd Global Conference on Nursing Care & Patient Safety
Toronto, CanadaRecommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 702
- [From(publication date): 0-2023 - Apr 04, 2025]
- Breakdown by view type
- HTML page views: 490
- PDF downloads: 212