Research Article Open Access
Stories of Dying and Death as told by Family Members’ of Adolescents and Young Adults (AYAs) who have Died from Cancer
Janet Barling* and Kierrynn Davis
School of Health and Human Sciences, Southern Cross University, Australia
- *Corresponding Author:
- Janet Barling
RN, PhD, Adjunct Lecturer
School of Health and Human Sciences
Southern Cross University, PO Box 157
Lismore , NSW 2480, Australia
Tel: 61-2410599164
Fax: 61-266203307
E-mail: jan.barling@scu.edu.au
Received date: August 02, 2016; Accepted date: September 20, 2016; Published date: September 23, 2016
Citation: Barling J, Davis K (2016) Stories of Dying and Death as told by Family Members’ of Adolescents and Young Adults (AYAs) who have Died from Cancer. J Palliat Care Med 6:284. doi: 10.4172/2165-7386.1000284
Copyright: © 2016 Barling J. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Research of AYAs with cancer has developed significantly over the last 20 years. The research has demonstrated that AYAs with cancer are a forgotten population, who require closer study in order to understand their unique issues. This paper examines family members’ experiences of adolescents and young adults (AYAs) during the dying stage of their cancer trajectory. The results are drawn from a larger study titled ‘From Go to Woe; Family Members’ Stories of Adolescents and Young People Living with and Dying from Cancer, which storied the family members’ experience of the diagnosis, treatment, dying and death of an AYA family member, utilizing Armstrong-Coster’s (2004) four stages of the cancer trajectory. The principal researcher’s motivation to understand and story these experiences was related to her own isolation and lack of information when her 16 year old son Anthony, was diagnosed with and eventually died of cancer at 17 years of age. The significance of this study is the contribution made to the identification of issues that can inform health policy/ guidelines. The findings have the potential to increase understanding of, and prepare family members and AYAs with cancer, for the experience of the death and dying stage of the cancer trajectory.
Keywords
Adolescents and young adults; Cancer; Death and dying; End of life decision making
Literature Review
Research over the last 20 years has indicated that AYAs with cancer are a forgotten population who require closer study in order to understand their unique problems [1-9] prompting Michelagnoli, Pritchard and Phillip [3] to describe this group of people as a lost tribe. One factor identified to account for this disadvantage is the fragmentation of services [1,10-12].
The fragmentation of services is a result of AYAs being cared for in two systems of care, the paediatric and the adult [13] with different goals and philosophies of care.
The paediatric system has been described as mainly family focused and the adult system disease focused [14].
This has implications not only for medical treatment of AYAs with cancer, but also presents problems in providing targeted support services. O’Brien, et al., [15] identified the following issues that account for the lack of support services.
Support services vary across adult hospitals and are fewer than those provided by specialist paediatric hospitals; support services provided both in paediatric or adult hospitals are not designed for the AYA age group, and the lack of critical mass in either system prevents optimal support service. These issues are amplified during the dying stage of the cancer journey.
There is limited research on AYAs dying with cancer and their families. A review of literature found only four authors [16-19]. Wein, Pery and Zer [19] provided information specific to this group and their specific psychosocial needs whilst dying.
Bisset et al. [16] identified the following needs for AYAs, their parents and siblings for palliative care services: “involvement in decision making, attention to developmental needs, an appropriate setting of care, ambivalence about taking on an adult role, a desire for independent living, the importance of school, college and employment, opportunities to do things other young people do, symptom relief and emotional support, planning of care to ensure the best end of life care possible.”
The researcher could find no research that specifically focused on AYAs and the dying trajectory, with the majority of the articles relating to children and their families. This is confirmed by Mack et al [18], who emphasized that there is limited knowledge about the End of Life (EOL) care that AYAs receive.
She states: “the development of optimal tools for EOL care delivery in this population will depend on a better understanding of the care such patients receive.” This paper will provide a further insight into the care of AYAs during the dying stage.
Research Aim
The aim of this article is to uncover from the stories of family members the experience of the dying and death of an adolescent or young adult (AYA) family member (aged 13-23 years).
Methodology
Narrative Inquiry was considered the most appropriate methodology for this study. Narrative inquiry uses stories to describe human experience [20-22]. Through story-telling meaning is constructed from the experience [21,23].
In narrative inquiry, the interview should be approached with the intent of hearing stories. Narrative has a commitment to the value of giving voice to human feelings and experience [24], through the use of “imaginative reconstruction” or “empathy” [25].
Grinyer [26] believes narrative is an appropriate method for sensitive research as it allows family members to determine the content of the information they share which she sees as strength rather than a weakness.
Narrative inquiry also includes the concept of a shared reality [20]. Bruner [20] has said that “life stories must mesh tellers and listeners must share some ‘deep structures’ about the nature of a life.” If this does not occur, both the storyteller and the listener will fail to grasp what the other is telling or hearing.
Narrative Inquiry therefore is a suitable methodology for this research study. Within its epistemology, understanding is the development of knowledge through the telling of stories. These stories create meaning and a testament of the experience of suffering, giving voice to what might not be told.
The methodology suggests my own experience, rather than hindering the research, creates the context for me as the researcher to grasp what the family member is saying and provide a richer understanding of what is being told.
Method
Ethics approval was obtained through the Southern Cross University Human Research Ethics Committee (Approval number ECN-05-146).
The family members in this study were a purposeful sample of 26 who had experienced the death of an AYA (aged 13 to 23) to cancer. Table 1 provides a representation of the family members relationship to the AYA, the interview type and time since death. The interviews were open-ended. All interviews were recorded on an iPod and professionally transcribed.
For the purpose of this study, family members preferred not to use pseudonyms and requested that their family member’s real names be used. Additional ethical approval was obtained from Southern Cross University’s Human Research Ethics Committee for this to be possible (approval number ECN-08-029).
The study utilised narrative analytic methods to create a configured plot of core stories and a configured meta-narrative from which commonalities and differences within the core stories were identified.
Guidance was obtained from the following narrative theorists: Mishler [27], Riessman [28,29], Polkinghorne [30], Lieblich, Tulval & Zilber [31], Emden [21,32], and Frank [33], to analyse these narratives.
In addition Taylor’s [34] computer-assisted method and the qualitative research software program NVivo8 provided a framework to configure and organise the stories into a meta-narrative.
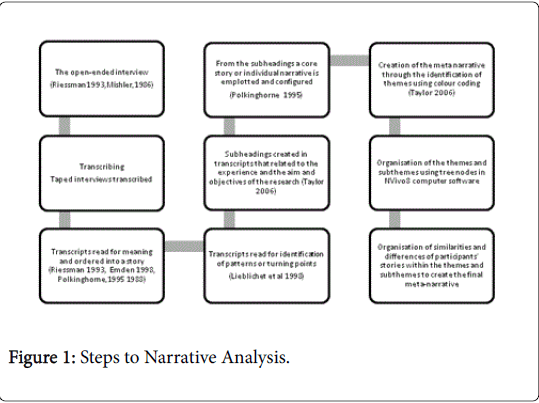
Figure 1 links the steps of the narrative analysis for this study with specific processes and relevant authors.Results
Results
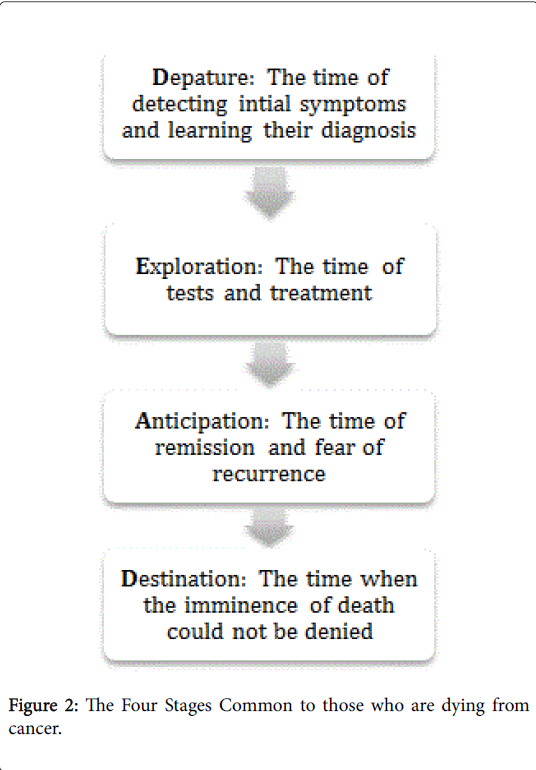
The narrative patterns within the stories identified transitional or turning points in the family members’ stories. These turning points related to the stages of the cancer journey identified by Armstrong- Coster: [35] departure, exploration, anticipation, and destination as represented in Figure 2.
Figure 2: The Four Stages Common to those who are dying from cancer.
This article provides insights into the experience of family members through themes identified within the destination stage. Table 1 provides a visual representation of the themes and subthemes.
| Narratives from the Dying Landscape Theme and subtheme | Number of stories | Number of references |
|---|---|---|
| Destination | ||
| Ending the Reprieve | 15 | 40 |
| The pronouncement of impending death | 17 | 37 |
| Being told Response to the pronouncement | ||
| Changing the Focus of care | 18 | 52 |
| Deciding where the care would be delivered How the care changed | ||
| Going downhill | 18 | 62 |
| The cancer has taken over Living with the symptoms Being overwhelmed with pain | ||
| Keeping a vigil | 18 | 37 |
| Being there Strengthening bonds | ||
| Experiencing Lack of Care | 12 | 37 |
| Lack of care in the hospital Non-support in the home Responses to non-support | ||
| Feeling overwhelmed | 10 | 25 |
| Burdened with suffering Enduring hard work Overcome with emotion | ||
| Witnessing heroism | 17 | 66 |
| Accepting reality Taking control Being grateful Protecting others Enjoying ordinary behaviours | ||
| Maintaining hope | 14 | 31 |
| Thinking of the future Having faith Not giving up Denying reality | ||
| Saying goodbye | 14 | 40 |
| Acknowledging feelings How much longer It’s OK to go | ||
| Recalling the moment | 17 | 46 |
| Waiting and watching Being present Missing the moment Sensing relief | ||
| Extending the living connection | 11 | 30 |
| Staying with the body Caring for the body Viewing the body | ||
Table 1: The Dying Landscape.
The results are a summary of the family members’ stories within the themes. Direct quotes from the participants stories are represented by quotation marks and italics.
Destination Stage
Ending the reprieve
The death and dying stage for the AYAs and family members in this study commenced when the AYA exhibited signs and symptoms that alerted the AYA and the family members that things were not getting better or the cancer had returned. Denise was shocked when Brenton James’s melanoma reoccurred in the liver as they had been told he was fine. She said “You know we got through this shocking period of him losing his eye and we’d been given the all clear. We’d got through this, we’d escaped.” Lauren noticed that Grant was not getting any better which was frustrating “then in the April he started coughing and we called the Oncologist and they said it is probably just a virus … but we will get an x-ray just in case and that is when we found the tumours in his lungs, So that was pretty devastating.” For most, tests and investigations were quick to confirm the return of the cancer. For Tamina who had transitioned from the paediatric to the adult system there was evidence of lack of communication within these two systems, as was seen in one story that resulted in a delay in diagnosis. Pam said “we’ve been coming back and forth, or Tamina had been for a few months with this cough … She was told she had a lung infection … and nobody cottoned on to actually send her for a chest x-ray.” When a Chest X-ray was finally ordered they found she had relapsed.
The pronouncement of impending death
The way that the family members were told of the impending death was not always satisfactory. Denise spoke of the frustration she felt when a young doctor tried to tell her Brenton James was dying: “the intern doctors … a lot of them are still finding their feet with how to deal with these things … especially the one that was trying to tell me that my son was critical and that he would die, he rambled on and on and on and on, and I wanted to shake him. To say … just say it … [I] know what you’re trying to say, but I didn’t.”
There was no evidence of a plan as to when, where, and how the family members were told, added to this there was little support for the AYA and the family member after the pronouncement. This is seen in Jenny’s story, she said the doctor rang her at work and said: “I'm sorry, but Brenton is going to die, we can't do anything about it. He has got metastasis everywhere”. Jenny then had the responsibility of telling her son, Brenton Duncan that he was going to die. For Pam, Tamina was told she was going to die with no support from family. Pam said “she (Tamina) was in there for a while [the doctors surgery] and he told her she was going to die … and they knew I was out in the waiting room.” Understandably the response for most was shock and devastation. Lauren recounted “the fact that that’s it, there is nothing more we can do for you was horrible.” For Fulvia the pronouncement of impending death did not occur until the AYA was near death. For example Fulvia recalled a doctor describing the dying process. She says doctor said: “Jadye’s condition has deteriorated, Jadye’s now unconscious and soon she’s going to start cheyne stoking, she’s going to start breathing different and so on and I don’t want you all to be distressed, it’s just the normal way of dying, there’s no pain and she’s not in any distress.”
Changing the focus of care
The family members noticed that with the pronouncement of impending death the focus of care changed both in how and where the care was delivered. Lauren spoke of how this quality of care changed: “whereas in the first time it was, well it doesn’t matter how sick he gets because in the end … he’ll be alive. … and so that really changed … it definitely didn’t feel that the medical profession treated him as a possibility, it was more a matter of when he died and how are we going to make from now to when he dies better than trying to prevent him dying.” Val’s story revealed the changing focus of care by deciding not to give Anthony Charles any more treatment. She said: “it was an easy decision, because why put the poor kid through so much more turmoil and hell than what he’d already been through, and who was it for, me or him? If I kept him alive it’d be for me.”
In some of the stories it is not evident if families were provided with alternative care delivery choices. There was an underlying assumption that the AYA would die in hospital. Deborah who had to insist that Matthew Anthony be allowed to go home to die, Deborah said: “… and when Matthew said he wanted to die at home and not in hospital, the doctor almost laughed at him, and said “well, that’s just ridiculous.” Deborah recalled Mathew saying, “I’m not going to die in hospital. If I’ve only got a week to live, I want to be at home,” Deborah insisted he die at home saying: “You said he’s going to die, there’s nothing more you can do for him, we’ve got scripts for his morphine and … all his medications. We’ve got the stuff, we’re going home and he will die at home.” For others there appeared to be a choice. For example Thomas was cared for at home. Irene said: “they told us then there was nothing else they could do. He stayed home. … he wouldn’t stay in hospital for the last… I think it was better for him to be at home. I think if any kid’s going to go through this, stay at home if you can get treatment at home rather than be in a hospital.”
Staying home for the last moments was not always a choice that the family member wanted. They had a sense that there was no alternative. Jenny spoke of how she felt deserted by the paediatric system because of Brenton Duncan’s age and that there was nowhere else for her to go but home. She said: “they did offer the hospice around the corner here but I went around to see it and it was just full of old people and I couldn't put my son there.” Only one of the AYAs died in a hospice (Ben), which Sue described as a caring and compassionate place.
Going downhill
It became evident to the family members in this study that their AYA was dying when they noticed their health was deteriorating. For some this was evident when they became aware that the cancer had taken over other parts of the body. Denise noticed that Brenton James’s “stomach become bloated his legs were full of fluid the rest of him was fading away and he was having increasingly that look of someone that has not got long to live.” Fulvia spoke of how quickly the cancer spread in Jadye “Within a week it was in her liver, in her lungs, in her back, in her shoulder and in her bone marrow, horrible cancer. It’s cruel.” For others it was associated with having to deal with the symptoms associated with the cancer spread, such as blindness and deafness, seizures and behaviours associated with neurological deterioration. Cheryl spoke of Paul becoming “blind and deaf and very, very frail” whilst Helen and Geoff spoke of Mick’s epileptic seizures “and he had … 2 or 3 really bad nights … like an epileptic seizure, … [he] broke a couple of his vertebrae in his back.” While Kerry described Alinta’s neurological deterioration, “ You have brain things … you might have fits … there’s agitation and fidgets.”
For others it was the AYA being overwhelmed by severe pain. Fulvia explains Jadye’s experience, “we sat up for night after night with her screaming… and she didn’t want to move, and she just begged me, … no leave me at home, leave me at home” and I yelled at her and made her go to the hospital and she never came home.” As with Jade, pain was the beginning of the end for Brenton Duncan as Jenny describes, “he was screaming in agony and we got the district nurse to come around and give him morphine … they put a driver into him … and we put him to bed and we will be able to look after him.”
Keeping a vigil
Throughout the cancer trajectory the family members sought to stay with the AYA as much as possible and continued to care for the AYA as their condition deteriorated. For many this involved lack of sleep, being at the hospital 24/7 and being concerned that the AYA might die without them being present. Arlene said: “I discovered you can actually go five days without sleeping … I kept thinking what if he dies [while I’m asleep].” Shane spoke of the admiration he had for his ex wife “she was up there like 24/7 at the hospital, [I] admired her for just being able to keep going … constant.” There was evidence that the adult hospital system was not equipped to support the vigil with many family members spending their time sleeping in hospital chairs as Shane explained: “she had one of these chairs, like a recliner, she’d sleep in those.”
Keeping vigil provided the opportunity to strengthen existing family relationships tempered by the understanding that the AYA was going to die. Denise explains: “we were on a journey that neither of us wanted to go on but nevertheless we were going to go on this journey together and we were going to support each other along the way.” Deborah spoke of the relationship between Matthew Anthony and Lauren (his sister): “and just watching that develop between the two of them was just beautiful … even more, it just moved onto a much deeper level … it was just beautiful, absolutely beautiful.”
Experiencing lack of care
Throughout this experience, the family members occasionally felt unsupported which made keeping a vigil difficult. This was evident in the lack of care and acknowledgment, by some hospital staff, that the AYA was dying. Rebekah described an incident: “and the nurse [said] come on we’ve got you get in bed and just grabs her legs and swings her up onto the bed and Naomi was crying in pain and then she, … pulled the blankets up and left. I was sitting there thinking … all she had to do was wait a minute so Naomi could catch her breath and get ready because she knew it was going to hurt.” For others there was the sense that there were not enough resources to support the family members in their home. Jenny said “he wanted to die at home so I wanted him to be with me but I just needed a respite every so often because it was very hard work when you don't know how long it is going to take, it's just all really really hard.” Kerry reinforced this: “so as far as I could see, … someone had given me a 24 hour watch, with no help … It’s just so hard and you get more and more isolated.”
An aspect of the lack of care was the lack of coordination, particularly if the AYA was at home. Jenny described the care as “higgledy-piggledy” whilst Kerry believed it would “have helped to have some-one oversee our whole care.” For Sue this lack of support required the AYA to be admitted to a hospice. She said: “Ben came home and he was home I think, two days, and he had a fall, his legs gave way, and I knew then he had to go back to hospital because I couldn’t lift him.”
Feeling overwhelmed
The lack of support whilst the family members maintained a vigil resulted in the family member at times feeling overwhelmed with the burden of care. The extent of the burden is exemplified by Deborah’s personal battle with herself about ending the pain. She said: “he actually begged me to kill him … but that kept playing over and over in my head and I thought my God, what sort of a person am I, he’s begging me to end his suffering and I’m saying no.” The majority spoke of how exhausting and hard this vigil was, and they just wanted the AYA to die to end the suffering. As expressed by Josephine, “this sounds really awful, but I’d had enough. I couldn’t cope with it any more, I could not cope with watching him going through what he was going through, … and it was just too much, and I just wanted him to die.” The hard work and witnessing the suffering caused some family members to become overwhelmed by emotions. For example, Lauren described a panic attack the day Grant died. She recalled “everything was just sort of blurry and hazy … I think that really it was just made by me needing to release that stress … It wasn't real easy … I guess we were just surviving.
Despite all the suffering and all the hard work that the family members had to endure, the journey was made easier by the courage and strength of the AYA who, rather than engage in self-pity, displayed heroic behaviours that made the journey easier for the family members. The family members spoke of the AYAs accepting the reality of their death, taking control of the dying, being grateful, protecting others and enjoying ordinary behaviours. Arlene told how Mathew James “made the decision that he would stay in hospital, keep the chest tube in, say his goodbyes and then we would take the tube out and he would be gone within 3 or 4 hours.” Deborah spoke of how Matthew Anthony planned his own funeral “picked his own casket, told me what he was going to wear, chose his own songs … He chose the funeral director chose the flowers that he wanted on his casket … we actually sat down and figured out the wording on the plaque, together.” The gratitude was expressed even at the end stage of dying. Lauren remembered Grant saying thank you to the nurse on the day he died “the nurse was giving him some morphine and he looked at her and he said thank you for everything.”
The AYAs protected and supported others as they were dying. Sue spoke of how Ben’s lack of complaining enabled her to manage this part of the journey. She said: “he never complained and that’s what everyone said to me, no matter how much pain he was in, no matter what he was feeling, he never complained. He never said, why me? Never, he never complained to the nurses, the doctors, he never wallowed in self pity, and that’s I think, how I got through, I kept thinking he was very strong.” Wherever possible, the AYAs sought to maintain and engage in normal behaviours. For example, Cameron recounted how he went to ‘schoolies’ with Kristie the month before she died: “so we got her to schoolies in 2000 … I went up there with her … she thought just come up and to be with her, to come up and have fun with her. We went up [the coast] and we had a great week together and stuff like that, and with her friends also.”
Maintaining hope
It is evident from the stories that the family members knew their AYA was going to die. Despite this it was important for many of them to hang on to some hope that things might change. This hope was evident in the AYAs still focusing on the future or to having faith that God would intervene. Cheryl described Paul Malcom’s attitude at the time “we were trying to get on with life, he was trying to do his year 12. He was very much thinking into the future…he was saying he wanted to be a physiotherapist.” This attitude was reinforced by Paul Malcolm’s faith in God. Throughout the journey he stated he wanted “to be healed and to glorify God.” Others maintained hope by continuing to believe that the treatment might make a difference. When Mathew Anthony’s cancer returned Deborah recalled he said: “ well, when do I start chemo? When can I start working on this?” Deborah said: “he fought it, even though it really wasn’t any point.” Similarly Grant said: “well if they give me two years…there maybe new clinical trials or there maybe a breakthrough.” While some sought alternative therapies, others maintained hope by denial. This is expressed by Irene who said: “I didn’t realise he was going to die…right up to the end I didn’t realise …probably pushed it to the back of my mind.”
Saying goodbye
Towards the end of the dying process, the family members spoke of the different ways they said goodbye. Some of the family members knew that the AYA was saying goodbye by the way they communicated their feelings. For example, Kristy said: “oh look Cameron I really love you.” Cameron said: “ it was if she knew that I knew that this wasn’t going to last any longer.” During this time the family members and some AYAs wanted to know how much longer the AYA had to live, because they wanted to say goodbye and for the suffering to end. Lauren said: “the day he died I didn’t believe it was happening … it wasn’t until Ian (nurse) said it will be within an hour and it just hit …It is like this is really happening and I couldn’t not want it to happen.” Mathew Anthony said to his mother (Deborah) “I’m very close, I’m going to die soon aren’t I?” and Deborah said “yes I think so, and he goes “good … that was the last thing he ever said.” Added to this many thought it was important to give permission for the AYA die. Lauren remembered, “I didn’t want him to be living he wasn't living he was existing and he was suffering … I said to him we’re not leaving, when you are ready to go I will be right here with you.” Arlene said, “dear God, he’s not mine anymore he’s yours,” and Mathew went, haah huh [deep breath in, then out], and … God was waiting for me to say, he’s yours not mine.”
Recalling the moment
For all the family members in this study the moment of death and being connected with the body after death were an important part of the Destination stage. For some the final moment of death was associated with waiting and watching for the last breath. Lauren recounted, “it was … kind of morbid because each breath was so far apart and so slight and we weren’t’ sure when he stopped…and then he kind of took this little gasp and then we were like waiting and waiting and waiting and another one didn't come. I just started crying.”
For most waiting for the last breath was not painful it was almost like just waiting for the end of the journey. For example, Pam watching Tamina’s breathing, she said: “but I just sat on the lounge and watched her breathing and I thought … afterwards of all the wonderful people, like my friends, that I would’ve wanted to share that with me.”
All wanted to be present when the AYA died. For those who were present, many felt lucky, some interpreting it as a beautiful spiritual experience. This is explained by Deborah, “we were all sitting around him and we were all with him when he died and it was beautiful, that’s really probably the only way I can describe it, it was just a beautiful experience, sad and hard but beautiful at the same time, if that makes sense.” Those who missed the moment felt disappointed that they couldn’t say a last goodbye. Irene described the experience: “I knew then that was it, he’d gone … … and in I went to see him and I laid by his side and I kissed him, I was sad because he’d gone and I’d never said goodbye.” For some who had missed the death there was a sense of disbelief that the AYA had died. Denise explained, “I walked into the room … and I could tell that he’d gone because the life had gone from his eyes and that was the biggest shock.“ The majority of the family members spoke of a sense of relief that the AYA’s suffering was over. For example, Deborah said: “I felt guilty afterwards, a few days after he died because I actually felt relieved when he died … relieved because his suffering was over.”
Extending the living connection
It was important that after the AYA died that the family members were given the opportunity to extend the living connection with the body after death. For some this meant spending time with the body. Lauren explained, “we went back in with Grant and spent some time there … I think I had the hardest time leaving … I guess I realised it is time to go when he started not looking like himself any more I didn't want to keep seeing him like that. So I hugged him and walked out.” Others found it important to care for the body in more physical ways such as washing and dressing the body. Deborah provided an explanation concerning the importance of caring for Mathew Anthony’s body. She said: “I was the first person to put clothes on him and I’m damn well going to be the last person. So I did, I dressed him and silly little things [is] I put 2 pairs of socks on his feet because he always got cold feet and I … put his blanket over him so he didn’t get cold … I’m glad I did it, even though technically I guess he couldn’t feel the cold, it made me feel better that I had rugged him up and he was nice and warm.” Others viewed the body, which helped them say goodbye. Sue recalled, “so we went to see him that afternoon … he looked very peaceful and very calm, and it was very, very hard … I just wanted to pick him up.”
Discussion
This summary of the themes created in the meta-narrative of the dying stage of the cancer journey provides insights into the dying of an AYA as experienced by family members. Wein [19] identified the psychosocial developmental phase and an AYA facing death, as unique for AYAs with cancer. An overarching issue associated with the Destination stage was the management of the dying for AYAs. De Jong and Clarke [36] described a good death as dying where one wishes, not dying alone, having a sense of a life well lived, having a long life, having the opportunity to say goodbye and prepare for death and a death free from pain and suffering. A bad death was associated with loss of control and independence. The stories in this research suggest that some of the AYAs were not given the opportunity for a good death. For example, it is not known whether all the AYAs died where they wished with only five of the 18 AYAs dying at home. This is despite research that demonstrates the best place for an AYA to die is at home [7,37-42], a place in which Williams [42] describes as an authentic place in which the AYA and the family are psychologically rooted. Brown et al [43] comment that home death facilitated being there, sustaining relationships, normalcy, self-direction and reciprocity which are all important elements for the AYA and the AYA’s family members’ journey. The stories did not speak of a life well lived compounded by the fact the AYA did not have the opportunity to live a long life. The stories do speak of pain and suffering and a sense of release when the AYA died. On the other hand family members’ maintained some form of control by maintaining a constant vigil to ensure the AYA did not die alone and was always supported. A semblance of control was also witnessed with the AYAs displays of heroism such as controlling the way they died, determining their funeral arrangements, and in simple ways such as maintaining their identity with friends and others.
A good death, is also facilitated by people being involved in EOL decisions early in the dying journey. Stillion & Papadatou [41] and Palmer & Thomas [7] recommend that palliative care be introduced concurrently with the diagnosis. Clayton, Hancock, Butow, Tattersall and Currow [44] in their clinical practice guidelines for communicating end-of-life issues with adults, believe health care professionals are uncomfortable discussing these end of life options. Reasons cited are “perceived lack of training, stress, no time to attend to the patients emotional needs, fear of upsetting the patients and a feeling of inadequacy or hopelessness regarding the unavailability of further curative treatment” [44]. Given these reasons for not initiating end of life discussions with adult patients, issues associated with AYAs and their families would be even more complex and confounded. The majority of family members in this study did not engage in EOL discussions and rarely was palliative care mentioned in the stories with 12 AYAs dying in the curative hospital system and only one AYA dying in a hospice. For most the pronouncement of impending death was at the end of the destination stage with little time to prepare for death or enter into EOL discussions.
The research studies have demonstrated that dying in a curative system results in EOL discussion occurring too late in the dying journey for adequate end of life decisions to occur [18,37,45,46]. Mack’s 2015 [18] study to evaluate the intensity of EOL care among AYA with cancer found 68% received at least one medically intensive treatment measure within the last 30 days of life, with 11% receiving chemotherapy within the last 14 days of life. Added to this is McGrath’s [46,47] study that reported carers in the curative system were not provided with information about alternative places to care for the patient when dying. Wittenberg-Lyles, Goldsmith & Ragan [48] describe this as the isolated journey occurring within a curative, biomedical structure limiting opportunities to discuss end of life care. This is in contrast to the comfort journey in which palliative care is introduced on diagnosis enabling life prolonging treatment and comfort care. The comfort journey provides opportunities for open communication on advanced care planning and end of life decision making [48].
It is not known if the AYA or the family members in this study were engaged in any EOL discussions. That there was no reference to this in the stories suggests that this did not occur. Supporting this is the fact that only one AYA died in a Hospice and of the five who died at home only Irene appeared to have seen this as a choice. Jenny and Kerry felt they had no choice and Deborah had to fight for her choice for Matthew Anthony to die at home. Jenny described the care as higgledy-piggledy with no plan or coordination. This supports the idea that palliative care be introduced early in order for patients and family members to plan their model of care [7,40,41,47,49], which is timely and integrated [50] and structured and coordinated [7].
Overlaying what appeared to be little opportunity for EOL discussions is the family members keeping a vigil with the AYA throughout the destination stage which involved many sacrifices. This keeping a vigil resulted in many feeling overwhelmed with the day-today care of a loved one who was dying. Added to this was the experience of feeling unsupported in the delivery of care. Despite this there was no mention of counseling being provided for either the AYA or the family members. The OnTrac Practice Framework states that access to supportive care is essential for young people facing death [7]. The National Service Delivery Framework mentions the profound effects on families when witnessing the cancer journey or death of a young person. The Framework recommends that service delivery should be mindful of these relationships and recommends grief and loss support is needed for AYAs and their families [50]. This is supported by the OnTrac Practice framework which recommends supportive care be available to family members and partners [7].
The destination stage culminates in the end stage of dying in which the AYA becomes increasingly dependent on the care of others. Palliative Care Australia stresses the importance of loved ones being informed about what to expect, how to respond and who is available to assist them. This information should include “the physical process of dying (i.e. changes in breathing patterns), psycho-education, and looking for signs of symptom relief ” [7]. It is not evident in Deborah’s story if she had been provided with information about dying and how to manage the pain associated with Matthew Anthony’s dying. There is the possibility that with adequate information she may not have experienced her dilemma of how to end his suffering.
It was only at the time that death was imminent that the family members were free to let the AYA go and end their suffering. It was important to say goodbye and to be there at the moment of death. After the death the family members continued their connection with the AYA with body caring rituals. The importance of this for the family members was evident in that they wished to describe in detail the moment of death and what occurred after the death. This highlights the need for health care professionals to be cognizant of the family’s needs during and after the death and to see the person as not just a body. Whilst there was a sense of relief at the moment of death, this moment augurs the transition to another stage incorporating the loved one into their life with memories and rituals.
Conclusion
Barling [8] sought to understand the experience of the AYA cancer journey from the perspective of family members. This article presents selected findings from the Barling [8] study that explained family members’ experience of during the destinations stage of the cancer journey.
The summary of the meta-narrative provides acknowledgment that the destination stage is difficult for the family members and the AYA. The stories reveal a lack of support and being overwhelmed with the burden of care as the family members maintained their vigil. Despite this the family members found it important to talk about the death and how they continued their living connection with their loved one after death. In addition, the absence of EOL discussions within the majority of the meta–narratives suggests that AYAs and family members are often not provided with the opportunity to consider EOL choices during the destination stage.
This article has therefore highlighted the need to continue research into the needs of AYAs and their families during the destination stage to further increase understanding and assist in the implementation of the National and OnTrack Framework recommendations, with particular emphasis on specific issues associated with the destination stage of the cancer journey.
Anthony’s words:
Mortality is a blessing taken without recognition.
We all walk the same tightrope.
Only some dare to look down, whereas others have to.
There is only one thing we can do: try not to walk the rope alone.
References
- (2005) CanTeen, Submission from CanTeen Australia, in Inquiry into services and treatment options for persons with cancer, S.C.A.R. Committee, Australian Government Printing Services, Canberra.
- Ewing J (2005) Cancer Inquiry Senate: Submission from Jane Ewing, in Inquiry into services and treatment options for person with cancer. S.C.A.R. Committee, AGPS Canberra.
- Michelagnoli M, Pritchard J, Phillips M (2003) Adolescent oncology- a homeland for the "Lost Tribe".Eur J Cancer39: 2571-2572.
- O'Connor (2006) On being treated as a person: A review of nonphysical interventions to improve the outcomes for adolescents and young adults with cancer.Sydney.
- Zebrack B (2008) Information and service needs for young adult cancer patients. Support Care Cancer 16: 1353-1360.
- Zebrack B, Chelser M, KaplaS (2010) To foster healing among adolescents and young adults with cancer: What helps? What hurts?Support Care Cancer 18: 131-135.
- Palmer S, Thomas C (2008) A practice framework for working with 15-25 year old cancer patients treated within the adult health sector.onTrac@PeterMac Victorian Adolescent & Young Adult Cancer Service, Melbourne.
- Barling J (2012) From go the woe: Family members' stories of adolescents living with and dying from cancer. Health and Human Sciences, Southern Cross University, Lismore.
- Palmer S (2007) Unmet needs among adolescent cancer patients: A pilot study. Palliat Support Care 5: 127-134.
- Albritton K, Bleyer W (2003) The management of cancer in the older adolescent. Eur J Cancer39: 2584-2599.
- Bleyer A (2002) Cancer in older adolescents and young adults : Epidemiology, diagnosis, treatment, survival and importance of clinical trials. Med PediatrOncol38: 1-10.
- Burke M, Albritton K, Marina N (2007) Challenges in the recruitment of adolescents and young adults to cancer clinical trials. Cancer110: 2385-2393.
- McTiernan A (2003) Issues surrounding the participation of adolescents with cancer in clinical trials in the UK. Eur J Cancer Care 12: 233-239.
- Ferrari A, Thomas D, Franklin AR, Hayes-Lattin BM, Mascarin M, et al. (2010) Starting an adolescent and young adult program: Some success stories and some obstacles to overcome. J ClinOncol28: 4850-4857.
- O'Brien T (2006) The need for change: Why we need a new model of care for adolescents & young adults with cancer. Management of Cancer Services,Melbourne.
- Bisset M, Hutton S, Kelly D (2008) Palliation and end of life issues, in Cancer Care for Adolescents and Young Adults. In: Kelly D, Gibson F (eds) Blackwell Publishing, Carlton.
- Hain R (2005) Whose dying is it anyway? Palliative care in adolescents, in Cancer and the adolescent. In: Eden T, Barr R, Whiteson M (eds) Blackwell Publishing, Carlton.
- Mack J (2015) End- of -Life Care Intensity Among Adolescents and Young Adult Patients with Cancer in Kaiser Permanente Southern California. JAMA Oncology 1: 592-600.
- Wein S, Pery S, Zer A (2010) Role of Palliative care in adolescent and young adult oncology. Journal of Clinical Oncology 28: 4819-4824.
- Bruner J (1987) Life as narrative. Social Research 54: 11-32.
- Emden C (1998) Theoretical perspectives on narrative inquiry. Collegian 5: 30-35.
- Polkinghorne D (1988) Narrative knowing and human sciences. Albany, State University of New York Press.
- Frank A (1997) The wounded story teller. University of Chicago Press.
- Kleinman A (1988) The illness narratives: Suffering, healing & the human condition. U.S.A.: Basic Books.
- Redwood R (1999) Information point: Narrative and narrative analysis. JCliniNurs8: 674.
- Elliot J (2005) Using narrative in social research : Qualitative and quantitative Approaches. Sage Publications Ltd
- Grinyer A (2002) Cancer in young adults : Through parents' eyes. Facing Death Series, ed. D. Clarke. Buckingham: Open University Press.
- Mishler E (1986) The analysis of interview narratives, in Narrative psychology: The storied nature of human conduct. In: Sarbin T (eds) Praeger Special Studies, London.
- Riessman C (1993) Narrative analysis. Qualitative Research Methods Series
- Riessman C (2004) Narrative interviewing, in The Sage encyclopedia of social science research methods. In: Lewis-Beck M, Bryman A, Liao T (eds) Sage Publications, London.
- Polkinghorne D (1995) Narrative configuration in qualitative analysis. International Journal of Qualitative Studies in Education 8: 5-23.
- Lieblich AR, Mashiach T, Zilber T (1998) Narrative research : Reading analysis and interpretation. Applied Social Research Methods Series. Sage publications.
- Emden C (1998) Conducting a narrative analysis. Collegian 5: 34.
- Taylor B (2006a) Qualitative data analysis, in Research in nursing and health care: Evidence for practice.In: Taylor B, Kermode S, Roberts K (eds) Thomson South Melbourne.
- Armstrong-Coster A (2004) Living and dying with cancer. Cambridge: Cambridge University Press.
- De Jong J, Clarke L (2009) What is a good death? Stories from palliative care. J Palliat Care 25: 61-64.
- Bell C (2010) End of life experiences in adolescents dying with cancer. Support Care Cancer 18: 827-835.
- Foreman L (2006) Factors predictive of preferred place of death in the general population of South Australia.Palliat Med 20: 447-453.
- Grinyer A, Thomas C (2004) The importance of place of death in young adults with terminal cancer. Mortality 9: 114-131.
- Hinds P, Pritchard M, Harper J (2004) End of life research as a priority for pediatric oncology. J PediatrOncolNurs21: 175-179.
- Stillion J, Papadatou D (2002) Suffer the children: An examination of psychosocial issues in children and adolescents with terminal illness. American Behavioural Scientist 46: 299-315.
- Williams A (1998) Therapeutic landscapes in holistic medicine. SocSci Med 46: 1193-1203.
- Brown P, Davies B, Martens N (1991) Families in supportive care - Part 1: Palliative care at home a viable care setting. J Palliat Care 6: 21-27.
- Clayton J (2007) Clinical practice guidelines for communicating prognosis and end -of life issues with adults in the advanced stages of a life-limiting illness, and their caregivers.Med J Aust186: 77-108.
- McGrath P (2002) End of life care for hematological malignancies : Technological imperative and palliative care. J Palliat Care 18: 39-47.
- Wolfe J (2000) Symptoms and suffering at the end of life in children with cancer. N Engl J Med 342: 326-333.
- McGrath P (2001) Dying in the curative system: The haematology/oncology dilemma. Part 1. Aust J Holist Nurs 8: 22-30.
- McGrath P (2002) Dying in the curative system: The haematology/oncology dilemma. Part 2. Aust J Holist Nurs9: 14-21.
- Wittenberg-Lyles E, Goldsmith J, Ragan S (2011) The shift to early palliative care: : a typology of illness journeys and the role of nursing. Clin J OncolNurs15: 304-310.
- (2009) CanTeen and Cancer Australia National Service Delivery Framework for Adolescents and Young Adults with Cancer.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 12371
- [From(publication date):
September-2016 - Jul 03, 2025] - Breakdown by view type
- HTML page views : 11456
- PDF downloads : 915