Case Report Open Access
Stereotactic Transsphenoidal Hypophysectomy by Radiofrequency for Chronic Pain from Hormone-Independent Metastatic Tumors: A New Perspective
Joao Gustavo Rocha Peixoto dos Santos*
Department of Neurosurgery, Sao Paulo University, School of Medicine, Brazil
- *Corresponding Author:
- Joao Gustavo Rocha Peixoto dos Santos
Department of Neurosurgery
Sao Paulo University, School of Medicine
Av. Doutor Arnaldo-455,Cerqueira Cesar
Sao Paulo-01246903, Brazil
Tel: 5511941989876
E-mail: joao_gustavo@icloud.com
Received date: August 08, 2016; Accepted date: September 14, 2016; Published date: September 19, 2016
Citation: Peixoto dos Santos JGR (2016) Stereotactic Transsphenoidal Hypophysectomy by Radiofrequency for Chronic Pain from Hormone-Independent Metastatic Tumors: A New Perspective. J Pain Relief 5:262. doi: 10.4172/2167-0846.1000262
Copyright: © 2016 Peixoto dos Santos JGR. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Pain & Relief
Abstract
Introduction: In 1953, Luft and Olivecrona described surgical ablation of the pituitary gland in the treatment of metastases from hormone-dependent tumors, with a view to reduce the spread of the disease rather than specifically for analgesia. The mechanism of hypophysectomy remains uncertain, but it has been suggested that part of the effect may be a result of the spread of physical-chemical agent through the pituitary stalk into the hypothalamus, thereby directly causing fixation, or indirectly causing thrombosis and infarction. The possibility of treating the pain in independent-hormonal tumors was tested, and presented satisfactory results. Based on that, we performed a stereotaxic transsphenoidal hypophysectomy by radiofrequency in a palliative patient.
Case Report: 54 year-old female patient, who was a smoker. In december, 2015, she started presenting dorsal back pain, radiating to the lower back, hip and medial thighs bilaterally, in distress, continuous, progressive, without triggering factors for worsening or improvement, which got worse on palpation. In March 2016, she was investigated at Hospital das Clinicas, School of Medicine, USP. Computed tomography of chest, abdomen and pelvis (03/14/2016): Multiple osteolytic lesions, lung mass in the left lower lobe base of 4.7 cm, diffuse injury in thoracic, lumbar and sacral-iliac spine. Iliac Biopsy (03/15/2016): mucinous adenocarcinoma. After staging, Oncology opted for palliative treatment. Pain treatment showed unsatisfactory analgesia. Due to that, it was proposed stereotactic transsphenoidal hypophysectomy by radiofrequency. Procedure was performed in April 14th, 2016, uneventfully Patient had considerable improvement in bone pain in the immediate postoperative day (VAS=0), getting back to walking. She kept hospitalizated until the fourth postoperative day. She was discharged on April 18th, 2016.
Conclusion: The procedure rises as an interesting option for refractory metastatic bone pain, presenting the advantage of fast resolution of intense pain and low rate of complications, diminishing hospitalization days, which is a fundamental aspect to be observed in these palliative patients
Keywords
Chronic pain; Hypophysectomy; Stereotactic; Radiofrequency; Bone metastasis; Oncology; Functional neurosurgery
Introduction
In 1953, Luft and Olivecrona described surgical ablation of the pituitary gland in the treatment of metastases from hormonedependent tumors, with a view to reduce the spread of the disease rather than specifically for analgesia [1]. Stereotaxic Trans-sphenoidal Microsurgical Hypophysectomy by Radiofrequency, by chemical agents or by ioning radiation is indicated for the treatment of pain due to endocrinological tumors (mainly bone metastasis) and deafferentation pain [2].
The mechanism of pain relief following hypophysectomy remains uncertain, but it has been suggested that part of the effect may be a result of the spread of physical-chemical agent through the pituitary stalk into the hypothalamus, thereby directly causing fixationl, or indirectly causing thrombosis and infarction [3]. The possible role of the pituitary, the hypothalamus, and endogenous opiates in mediating the pain relief associated with hypophysectomy was examined. There is significant evidence that this relief is not related directly to the expected fall in the levels of known pituitary hormones. Evidence is provided that pain relief is the result of a hypothalamic pain-suppressing capability triggered by hypophysectomy [4].
Otherwise, total pituitary function is not lost. Trans-ethmoidal/ trans-sphenoidal hypophysectomy may not totally ablate pituitary endocrine function; effective relief of bone pain in patients with metastic breast cancer can follow this procedure despite residual pituitary function and the lack of objective tumor remission [3]. The function was tested by measuring base-line values of follicle-stimulating hormone and luteinizing hormone, thyrotropin-relasing-factor-stimulated thyrotropin and prolactin, and levodopa-stimulated growth hormone after hypophysectomy in 15 menopausal women with metastatic breast cancer. In all 15, bone pain diminished or disappeared within 24 hours of operation. Pituitary-function testing identified only one patient as having had an endocrinologically complete hypophysectomy. Baseline gonadotropin levels and thyrotropin-releasing-factor-stimulated prolactin were the most reliable measures of residual pituitary function [3].
The main complications related to the procedure are temporary diabetes insipidus (17%), loss of visual field (10%), temporary ophtalmoplegia (4%), cerebral spinal fluid (CSF) leakage (6%) [5- 7]. Stereotaxic approach to the hypophysectomy was introduced by Levin and Katz because of a desire to improve the technique, reducing the ratio of CSF leakage compared to the surgical approaches with a precise ablation of pituitary gland [8]. As the technology has improved stereotaxic techniques, percutaneous methods for lesion, using radiofrequency termal were created and perfomed more often [9].
The possibility of treating the pain in independent-hormonal tumors was tested, and presented satisfactory results. In 10 series, involving 334 patients with breast or prostate cancer, surgical hypophysectomy produced pain relief in 70% of the patients afflicted with either tumor, including some with no evidence of hormone dependence. This procedure was performed in 3 series involving 533 patients, of whom 24% had cancer other than breast or prostate. Chemical hypophysectomy produced pain relief in over 75% of the patients, regardless of tumor type or hormonal dependence [4].
Based on the reports of good results for treatment of refractory pain in bone metastatic independent-hormonal cancer, we performed a stereotaxic trans-sphenoidal hypophysectomy by radiofrequency in a patient, presenting intractable pain secondary to bone metastastic disease in follow-up at Instituto do Cancer do estado de São Paulo Dr. Octavio Frias.
Case Report
The case is about a 54 year-old female patient, who was a smoker (42 pack-year) and presented no other relevant past medical history. In December, 2015, she started presenting back pain, radiating to the lower back, hip and medial thighs bilaterally, in distress, continuous, progressive, without triggering factors for worsening or improvement, which got worse on palpation. The pain was intense (She could not being able to walk because of the pain. VAS 10/10), and presented also night time awakenings due to pain.
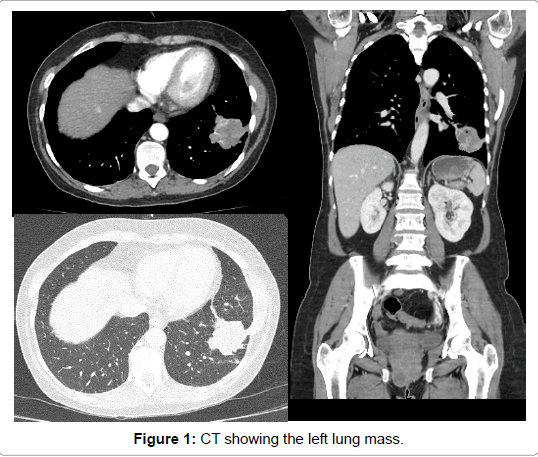
In March 2016, she was investigated at Hospital das Clinicas, Faculty of Medicine, USP. Computed tomography of chest, abdomen and pelvis (03/14/2016) (Figure 1). Multiple osteolytic lesions, nodules in the retroperitoneal fat, lung mass in the left lower lobe base of 4.7 cm, diffuse injury in thoracic, lumbar and sacral - iliac spine.
Scintigraphy (3/22/2016): hyperconcentration radiopharmaceutical in skullcap, upper arms, right scapula, pelvis, right femur, left femur, right ankle suggestive of bone involvement by infiltrative process secondary to the underlying disease (osteoblastic and osteolytic activity). Iliac biopsy (03/15/2016) was performed: mucinous adenocarcinoma (GATA3 napsin NEGATIVE NEGATIVE NEGATIVE 8 PAX-TTF-1 NEGATIVE cytokeratin 7 POSITIVE NEGATIVE cytokeratin 20 CDX-2 NEGATIVE NEGATIVE CA19.9)
In March 26th, 2016, the patient was transferred to ICESP. She was submitted to Palliative Radiotherapy for pain in pelvis starting in March 27th, 2016 (total dose 10 × 300 cGy).
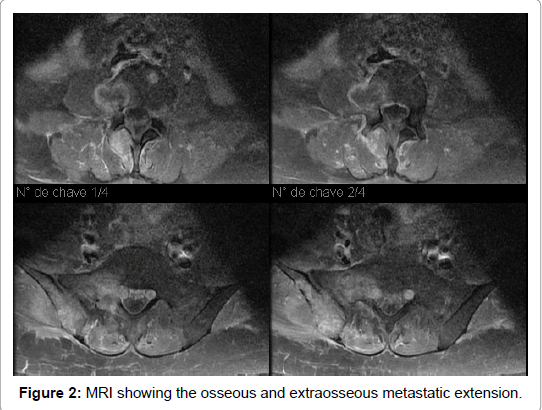
Spine MRI (03/31/2016) (Figure 2), multiple bone lesions, some of them with areas of rupture of cortical and soft tissue components associated. C5 vertebral body, and right transverse process of D5, with extraosseous soft tissue component extending to the paraspinal muscles. Lesion with soft tissue component in the posterior aspect of the sixth right costal arch. Body, right pedicle, lamina of the right posterior arch and spinous process of L4 with extraosseous soft tissue component to the adjacent paraspinal muscles without involvement of the spinal canal. Side of the right S1, with foraminal soft tissue components (S1-S2) compressing and inferior-medially displacing the ipsilateral S1 root. Right Sacroiliac region with soft tissue components to the adjacent muscles.
After completed staging, presenting a disease in an advanced stage and added to the performance status of the patient, Oncology opted for palliative treatment, being the patient not being a candidate for resuscitation or invasive treatment. Pain group started following up with gradual increases in medications (Table 1), but with unsatisfactory analgesia.
| MEDICATION | DOSE/ROUTE |
|---|---|
| Fentanil Patch | 25 ucg/h |
| Gabapentin 400 mg | 400/400/400/800 Oral |
| Dipyrone 2g | 2g/2g/2g/2g IV |
| Venlafaxin150mg 1 × /dia | 1×d Oral |
| Ciclobenzaprin 10mg | 10/10 Oral |
| Lorazepam 1mg | 1×d Oral |
| Metadon 15mg | 15/15/15 Oral |
| Morfin 7mg | 2/2h IV If necessary |
| Dexametason 4mg | 4/4 IV |
| CIB Cetamin | 0.1 mcg/Kg IV |
Table 1: Medication and dose/route relationship.
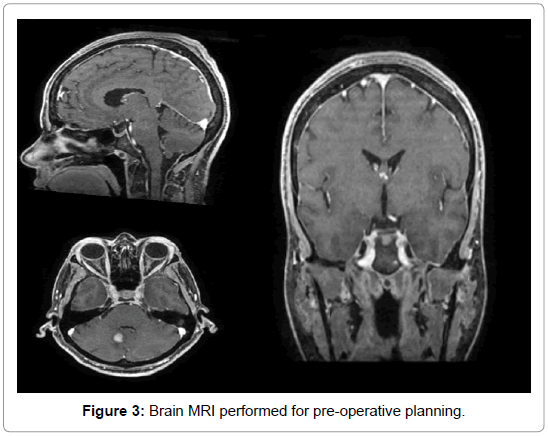
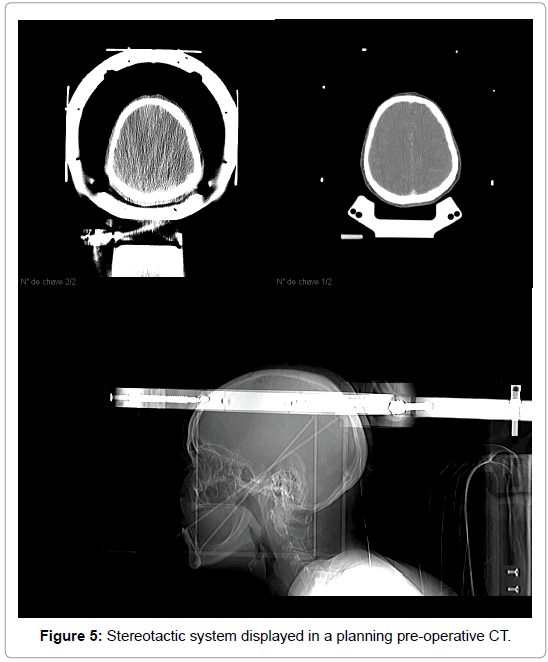
Due to the treatment resistance in control of the pain, it was proposed stereotactic transsphenoidal hypophysectomy by radiofrequency. A brain magnetic resonance was performed before the surgery for planing (Figure 3). The stereotactic procedure was performed in April 14th, 2016, uneventfully (Figures 4 and 5). After correct identification and pituitary punction, three radiofrequency lesions were performed, using 60, 70 and 80ºC, respectively. Patient had considerable improvement in bone pain in the immediate postoperative day (VAS=0), getting back to walking. She kept hospitalizated until the fourth postoperative day, which followed in weaning from intravenous medications and remain painless, without CSF leak or other complications. The weaning is described in (Table 2).
| MEDICATION | DOSE/ROUTE | WEANING |
|---|---|---|
| Fentanil patch | 25 mcg/h | Suspended in POi |
| Gabapentin 400 mg | 400/400/400/800 Oral | Mainted |
| Dipyrone 2g | 2g/2g/2g/2g IV | Changed for oral in PO1 |
| Venlafaxin 150mg 1 × dia | 1×d Oral | Mainted |
| Ciclobenzaprin 10mg | 10/10 Oral | Mainted |
| Lorazepam 1mg | 1×d Oral | Mainted |
| Metadon 15mg | 15/15/15 Oral | Mainted |
| Morfin 7mg | 2/2h IV If necessary | Suspended |
| Dexametason 4mg | 4/4 IV | Changed for oral in PO1 |
| BIC de Cetamina | 0.1mcg/kg IV | Suspended in 17/04 (PO3) |
Table 2: Analgesic Weaning strategy.
The post-operative hormonal profile presented was unchanged (Table 3). Due to good clinical course of the painful condition posthypophysectomy, the patient was discharged on April 18th, 2016. After one month of discharge, the patient was hospitalized for pneumonia and evolved to death in this hospitalization in May 20th, 2016.
Discussion
Hypophysectomy was described for pain treatment since 1953 for Luft and Olivercrona [5], otherwise, first intention was hormonedependent metastatic cancer treatment. Other authors tried different strategies of surgical pituitary ablation, using chemical and physical ways and finding the same effective results [1-4]. Thus, despite of an unknown, but only hypothesized pathophysiology so far, the procedure could be added to the therapeutical plan of oncology patients presenting bone and diffuse pain secondary to metastatic disease in homonedependent tumors [1]. As it is known this procedure was only tried for hormone-dependent bone metastatic tumors, however, interesting results were found when authors tried for different primary etiologies of bone metastasis and found satisfactory improvement of pain [4]. The efficiency of the hypophysectomy for these non-hormonal metastatic tumors is consistent with the post-operative unchanged hormonal pituitary profile [3]. It makes to question the true pathophysiology which is still unclear.
These authors tried the procedure for main types of metastatic disease. First results showed satisfactory improvement of pain in different types of cancer (overall improvement of pain of 70-75%, independently of primary cancer hormone-dependency). However prospective randomized clinical trials were not performed to formally test this hypothesis of pain improvement after procedure, the follow-up of this patients, including date about time free of pain, types of primary tumors from which could benefit, complications (Cerebral Spine Fluid leakage, blindness, worsening of pain) remains missing. Incidentally, since the beginning of 90’s, no relevant clinical studies were perfomed to try to emphasize the role of this technique in the therapeutical arsenal of pain improvement.
Hypophysectomy for pain was forgotten for almost a decade, resurfacing in the present days. In this view, it was proposed for the patient presented in this case as a strategy for refractory bone diffuse bone pain. There were no complications during or after the surgery. Temporary diabetes insipidus (17%), loss of visual field (10%), temporary ophtalmoplegia (4%), cerebral spinal fluid (CSF) leakage (6%) are the typical complication that can happen [6,7,9]. After completion, the pain disappeared (VAS=0), and maintained this way until the day of discharge (5 days after surgery). There was such a considerable improvement of pain, that it was possible to wean intravenous painkillers, shortening hospitalization.
Conclusion
Despite hypophysectomy having been forgotten for about a decade, the procedure rises now as an interesting option for refractory metastatic bone pain, presenting the advantage of fast resolution of intense pain and low rate of complications, diminishing hospitalization days, which is a fundamental aspect to be observed in these palliative patients.
References
- Luft R, Olivecrona H (1953) Experiences with hypophysectomy in man. J Neurosurg 10: 301-316
- Teixeira MJ, Hamani C, Teixeira WGJ (2001) functional surgical treatment of pain. Rev Med 80:276-289
- Lloyd JW, Rawlinson WAL, Evans PJD (1981) Selective hypophysectomy for metastatic pain A review of ethyl alcohol ablation of the anterior pituitary in a Regional Pain Relief Unit. Br J Anaesth 53: 1129-1133
- Ramirez LF, Levin AB (1984) Pain relief after hypophysectomy.Neurosurgery 14:499-504
- LaRossa JT, Strong MS, Melby JC (1978) Endocrinologically incomplete transethmoidal trans-sphenoidal hypophysectomy with relief of bone pain inbreast cancer.N Engl J Med 298: 1332-1335.
- Luft, R, Olivecrona H, Ikkos D, Kornerup T, Ljungggren H (1955) Hypophysectomy in man. Br Med J 2: 752-756
- Kandel EI (1989) Functional and Stereotactic Neurosurgery: Pain, Springer US, New York.
- Bruera E, Higginson IF, von Gunten C, Morita T (2015) Textbook of Palliative Medicine: Epidural and intrathectal analgesia and neurosurgical techniques. Taylor & Francis CRC Press.
- Levin AB (1988) Stereotactic Chemical Hypophysectomy. Modern Stereotactic Neurosurgery. Springer US Book, New York.
Relevant Topics
- Acupuncture
- Acute Pain
- Analgesics
- Anesthesia
- Arthroscopy
- Chronic Back Pain
- Chronic Pain
- Hypnosis
- Low Back Pain
- Meditation
- Musculoskeletal pain
- Natural Pain Relievers
- Nociceptive Pain
- Opioid
- Orthopedics
- Pain and Mental Health
- Pain killer drugs
- Pain Mechanisms and Pathophysiology
- Pain Medication
- Pain Medicine
- Pain Relief and Traditional Medicine
- Pain Sensation
- Pain Tolerance
- Post-Operative Pain
- Reaction to Pain
Recommended Journals
Article Tools
Article Usage
- Total views: 11568
- [From(publication date):
September-2016 - Mar 31, 2025] - Breakdown by view type
- HTML page views : 10648
- PDF downloads : 920