Static Foot Posture - Predictor of Dynamic Foot Motion
Received: 21-Aug-2015 / Accepted Date: 21-Sep-2015 / Published Date: 28-Sep-2015 DOI: 10.4172/2165-7025.1000272
Keywords: Static foot posture; Cartilage; Synovium; Physiotherapy
360993Introduction
Osteoarthritis is a as an illness commonly affecting the middle age to elderly population. It is the most common disease of arthritis and can occur together with other types of arthritis. It is a disease of the entire joint, involving not only the joint lining but also cartilage, ligaments, and bone. It is characterized by breakdown of the cartilage, bony changes of the joints, deterioration of tendons and ligaments, and various degrees of inflammation of the synovium [1].
Our bones contain collagen (protein), calcium salts and other minerals. Each bone is made up of a thick outer shell known as cortical bone and a strong inner mesh of trabecular bone which looks like a honeycomb, with blood and bone marrow between the struts of bone. Osteoporosis occurs when the struts that make up this structure become thin causing bones to become fragile and break easily. Osteoporosis is commonly linked to post menopausal women. However men, younger women, children and pregnant women can also be affected [2].
Osteoarthritis symptoms can vary greatly among patients. Symptoms include joint pain and stiffness, swelling, decreased function, and cracking or grinding noise with joint movement [3]. Symptoms usually start gradually in a prolonged history of discomfort associated with exacerbation [4]. Symptoms are often variable in severity and change slowly.Based on the European League Against Rheumatism (EULAR) evidence-based recommendations, typical symptoms of knee osteoarthritis are pain, often worse towards the end of the day, relieved by rest; feeling of ‘giving way’; only mild morning or inactivity stiffness and impaired function. In advanced cases, more persistent rest and night pain may occur. In adults aged >40 years with knee pain, there are only short-lived morning stiffness, functional limitation and one or more typical examination findings (crepitus, restricted movement, bony enlargement).Typically, the patient may grasp around the knee, indicating deep pain in the joint or bone [5].
Bone mineral density -2.5 or below is suspected with osteoporosis. Clinical features of postmenopausal osteoporosis include low bone mass, fracture-vertebral compression fractures, hip fracture, increased risk of falls. Complications of fractrure leads to pain, disability, deformity and physical deconditioning [2].
In both the conditions weight bearing joints are in stress. Weight bearing joints include spine, hip, knee and ankle. Thus disorders related to foot and ankle is most common as it is first most joint in contact with the ground. The foot is a biomechanical marvel made up of 26 bones, 58 joints, 7 ligaments, 19 intrinsic muscles, and 13 extrinsic muscles all working together in concert to provide balance, stability, and locomotion. The ankle and foot complex play a critical role in maintaining erect posture, as also in adaptation to supporting surfaces, in correcting postural sway in single limb stance, in shock absorption and in transition of ground reaction force (GRF) in order to aid the push off during normal gait [6]. Functional variance and minimal biomechanical alterations in the ankle and foot complex in turn alters the contact with the surface area and the peripheral sensory input in weight bearing posture. Changes in neuromuscular strategies alter the ability to maintain a stable and upright posture, and anticipatory postural control is reduced, increasingly predisposing the individual to falls and associated injuries. Structural deviations in the ankle and foot complex predispose the individual to changes in weight bearing, muscle imbalance static as well as dynamic balance in ambulation resulting in compensatory strategies which often predispose the individual to overuse injuries [7].
Various deformities of foot are rearfoot varus, forefoot varus, equines, plantar flexed 1 st ray, Forefoot valgus, rearfoot valgus. Mostly two types are observed-compensated and uncompensated. Compensated refers to a change in structural alignment or position of one part of the foot to neutralize the effect of a structural problem in another part of foot. Uncompensated refers to the structural position of the whole foot or one part of the foot in nonweight bearing situation. Orthosis are devised to correct the foot position, reduces the excess movement before the cutaneous receptors under foot sense the motion.
Variations in foot posture are thought to influence the function of lower limb and therefore play a role in predisposition to overuse injury. Various static measures are investigated as predictors of dynamic rear foot motion like rearfoot angle, medial arch angle, arch ht. But till date no accurate predictors of dynamic rear foot motion has been established. Benefits of having static measures predicting dynamic rearfoot motion assist in improved accuracy of clinical screening, orthotic advice and standardization of foot type [8].
Methods
Its is a critical narrative review. The Foot Posture Index (FPI-8) is a novel method of rating foot posture using set criteria and a simple scale [9]. It is a measure of standing foot posture and so is not a replacement for gait assessment where time and facilities exist.
It is however a more valid approach than many of the static weightbearing and non-weightbearing goniometric measures currently used in clinic. FPI-6 is derived from FPI-8 where two items were removed due to lack of unidemensionality. Foot posture index is an easy tool yielding quantifiable data with good face validity and can be performed with no special equipments.
Psychometric properties of outcome measure are validity (64%), reliability-inter rater reliability—0.62 to 0.91, intra-rater reliability-0.81 to 0.91 of FPI and clinical utility [10].
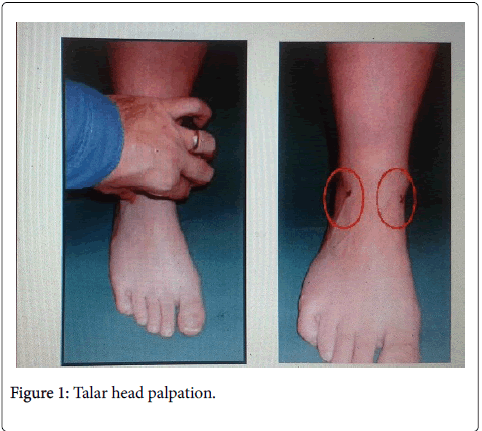
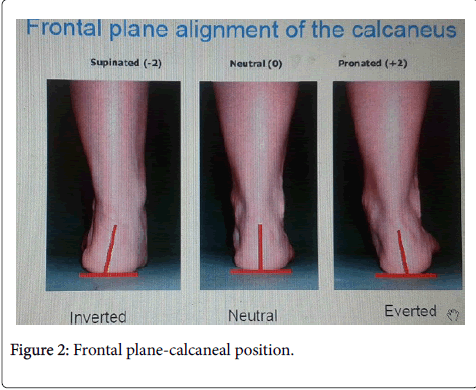
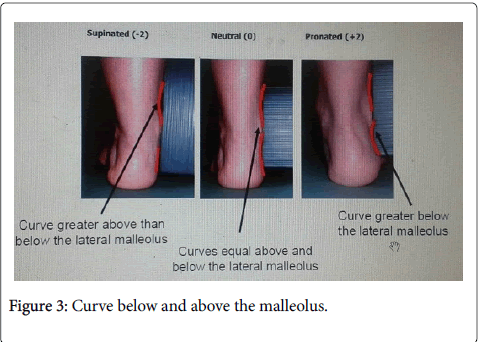
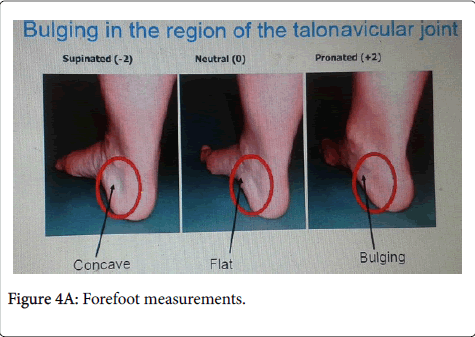
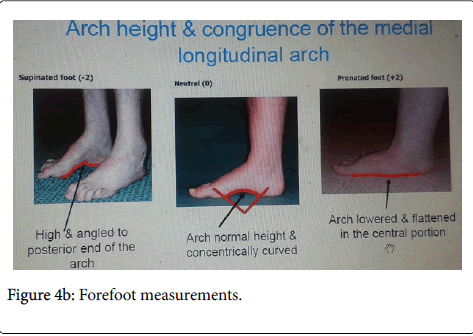
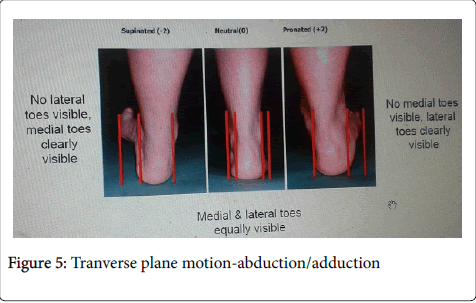
FPI consists of rearfoot and forefoot measurements. Rearfoot includes a combination of transverse and frontal plane assessments including talar head palpation, curvature above and below the malleolus, frontal plane calcaneal position. Forefoot includes a combination of sagittal plane assessments including prominence of talonavicular buldge, congruence of medial longitudinal arch and transverse plane motion (abtn/addtn).
FPI scoring rated from -2 to +2,0 for neutral,-2 for clear signs of supination and +2 for clear signs of pronation.Patient should stand in their relaxed stance position with double limb support (Figure 1).
a) Rearfoot measurements
Ask the patient to spot on march, take few steps prior taking a comfortable stance position.The assessor needs to be able to move around the patient during assessment to have no disturbances when it comes to observe the posterior leg and foot. Final FPI score between -12 to +12. Result is there is dominance of motion occurring in one of the three body planes or a difference between the function of forefoot and rearfoot.Score 0 to+4- normal,+5to+9- pronated, 10+-highly pronated,-1 to -4- supinated,-5 to -12 –highly supinated.
Discussion and Conclusion
Foot posture index allows monitoring the outcome of rehabilitation process in foot impairments and monitoring the progress with intervention (Figure 2). Applicaions of FPI include to identify biomechanical risk factors for neuropathic ulceration in diabetes, Identifying foot type as a basis for screening subjects as inclusion or exclusion criteria in clinical research, investigating relationship between foot types and risk factors for sports and training injuries, investigating whether foot posture is associated with falls in older people [11].
Foot posture index shows good association with age, gender, pathological disease and BMI as it it identifies the foot type.Vijaya et al. stated that the age and presence of pathology influences foot posture while gender and BMI (body mass index) does not have any effect [7]. Target et al. established normative values in UK and suggested there is an increased occurrence of flat foot in 3 year-old children and a gradual decrease of flat foot with increasing age (Figure 3). The pronated foot in younger children is said to get corrected itself with increasing age [12]. Scott et al. proved older adults tend to show pronated foot than younger adults [11].
FPI showed no association between males and females. Staheli et al. showed minimal difference between males and females with FPI which can be considered negligible [13].Thus FPI shows no relation with gender.
External factors like anthropometry and BMI varies among different ethninc groups are said to have effect on foot posture in developing children [7]. Previous studies undertaken using measures such as the footprint angle (FA) and the Chippaux-Smirak index (CSI) have reported lowered longitudinal arches, a broader midfoot area and subsequently flatter feet in people with high BMI values. Foot print measures are a measure of Fat feet rather than flat feet (Figure 4a and b). Thus the arch height is interfered with adipose tissue. Otherwise FPI shows no relation with BMI [11].
Previous studies proved foot posture differences may be encountered in association with underlying disease process or functional pathology [14-16]. Redmond et al. stated and proved that FPI data is sensitive related to disease related postural changes and assist in clinical decision making process [11]. Limitations of studies regarding FPI it was not performed with dynamic activities like walking, stair climbing accoreding to each stance and stike phase so that it can solely show FPI is a predictor of dynamic foot motion. Future studies should be performed with FPI association with pathology related dynamic activities dysfunction.
Based on the analyses, it is concluded that foot posture is influenced by age and presence of pathology, but is not influenced by sex or BMI. Thus FPI as a static foot posture is a predictor of dynamic foot motion.
References
- Alshami AM (2014) Knee osteoarthritis related pain: a narrative review of diagnosis and treatment. Int J Health Sci (Qassim) 8: 85-104.
- Nelson Watts,Steven Harris,Micheal.M et al.National Osteoporosis society. March 2015.
- Srikulmontree T. Osteoarthritis [Internet]. 2012 [updated 2012; cited 2012 Dec 03]. Available from:http://www.rheumatology.org/practice/clinical/patients/diseases_and_conditions/osteoarthritis.asp.
- Banks K, Hengeveld E (2010) Maitland's clinical companion: an essential guide for students. Edinburgh: Churchill Livingstone
- Zhang W, Doherty M, Peat G, Bierma-Zeinstra MA, Arden NK, et al. (2010) EULAR evidence-based recommendations for the diagnosis of knee osteoarthritis. Ann Rheum Dis 69: 483-489.
- Mueller MJ (2005) The ankle and foot complex. IN:Levangie PK, Norkin CC. Joint structure and function, a comprehensive analysis. 4th ed. Philadelphia: F. A. Davis Company; 437-477
- Vijaya K, Das B, Narayan A et al. (2014) Normative Data for Foot Posture Index (FPI-6) and Association of Foot Posture with Anthropometric Parameters in School Children from Mangalore: A Cross Sectional Study. International Journal of Research and Development of Health 2: 107-115.
- Chuter VH (2010) Relationships between foot type and dynamic rearfoot frontal plane motion. J Foot Ankle Res 3: 9.
- Morrison SC, Ferrari J (2009) Inter-rater reliability of the Foot Posture Index (FPI-6) in the assessment of the paediatric foot. J Foot Ankle Res 2: 26.
- Redmond AC, Crane YZ, Menz HB (2008) Normative values for the Foot Posture Index. J Foot Ankle Res 1: 6.
- Target R, Mathieson I (2010) Evaluation of foot posture development in children between three and eleven years of age using the foot posture index. J Foot Ankle Res 3: 17.
- Staheli LT, Chew DE, Corbett M (1987) The longitudinal arch. A survey of eight hundred and eighty-two feet in normal children and adults. J Bone Joint Surg Am 69: 426-428.
- Murley GS, Landorf KB, Menz HB, Bird AR (2009) Effect of foot posture, foot orthoses and footwear on lower limb muscle activity during walking and running: a systematic review. Gait Posture 29: 172-187.
- Cobb SC, Bazett-Jones DM,Joshi MN, Earl-Boehm JE, James RC (2014) The relationship among foot posture,Core and lower extremity muscle function and postural stability. Journal of athletic training 49: 173-180
- Barton CJ, Levinger P, Crossley KM, Webster KE, Menz HB (2011) Relationships between the Foot Posture Index and foot kinematics during gait in individuals with and without patellofemoral pain syndrome. J Foot Ankle Res 4: 10.
Citation: Telegbal VS (2015) Static Foot Posture - Predictor of Dynamic Foot Motion . J Nov Physiother 5: 272 DOI: 10.4172/2165-7025.1000272
Copyright: © 2015 Telegbal. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 16025
- [From(publication date): 10-2015 - Jul 02, 2025]
- Breakdown by view type
- HTML page views: 11295
- PDF downloads: 4730