Research Article Open Access
Staging Issues in Cervical Cancer
Chhabra S*, Devi S, Chopra S and Singh A
Obstetrics Gynaecology, Mahatma Gandhi Institute of Medical Sciences, Maharashtra, India
- Corresponding Author:
- Chhabra S
Obstetrics Gynaecology, Mahatma Gandhi Institute of Medical Sciences
Sevagram- 442102, Wardha, Maharashtra, India
Tel: +917152284342
E-mail: chhabra_s@rediffmail.com
Received April 05, 2016; Accepted April 30, 2016; Published May 06, 2016
Citation: Chhabra S, Devi S, Chopra S, Singh A (2016) Staging Issues in Cervical Cancer . Can Surg 1:104.
Copyright: ©2016 Chhabra S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Cancer Surgery
Abstract
Background: Worldwide cervical cancer is third most common cancer, but diagnostic, therapeutic problems continue in developing countries where it is most common cancer in women. Very few women report at operable stage. For those subjected to surgery, intraoperative findings, histopathology provides information for continuing or abandoning surgery, adjuvant therapy after surgery and so on. However clinical investigative staging may not be correct, leading to avoidable morbidity of surgery.
Objective: Study was done to know relationship between clinical, intraoperative, postoperative staging in women who underwent surgery for cervical cancer.
Material methods: Analysis duration was divided into 4 yearly 7 blocks. During study period 266 women underwent abdominal radical hysterectomy, 15 were for endometrial cancer so, 251 (94.36% radical hysterectomies for cervical cancer, 13.05% of all cervical cancers cases (stage I A, I B1, II A1) were study subjects.
Results: Cervical cancer cases increased over the years and also operable cases of cervical cancer from 13.33% to 30.00%. However of 251cases taken for surgery, 28% would not have been for surgery if were known to be of stage which was found intraoperative (preoperative under staging), over staging was only in 2%. Correlating clinical, histopathological staging 36% would not have been for surgery if correct staging (after histopathology) was known pre-operatively. Clinical intraoperative staging had 72% agreement. Histopathological staging which helps in planning treatment agreed with clinical staging in 64%. Problem of under staging continued over years.
Conclusion: With present day techniques available to women with low resources, there is a lot of under staging of cervical cancer cases which leads to unnecessary surgery. Low cost modalities for better evaluation of cases preoperatively and will help in reducing morbidity, save resources also.
Keywords
Cervical cancer; Radical hysterectomy; Clinical; Final staging
Introduction
Worldwide cervical cancer is the third most common cancer affecting women, in terms of incidence and mortality rates [1,2]. However in some parts of the world including India, it is the most common cancer in women [3-5]. Around one sixth to one fifth worldwide cases of cervical cancer occur in India [2-6,7]. It accounts for 280,000 deaths every year [2,8-10]). When cervical cancer is diagnosed, attempts are made to know the right stage for planning best therapy for prevention of mortality and helping in quality life. This is especially important for countries where resources are limited with problems of availability of high cost diagnostics and therapeutics. Also cervical cancer is more in women from low resource countries. Very few women with cervical cancer report at operable stage [11,12] and for those subjected to surgery, intraoperative findings, provide information for continuing surgical therapy or abandoning the procedure or having adjuvant therapy after surgery. Histopathological evaluation of the surgical specimen provides information for determining the final treatment plans and prognosis for an individual patient. Node histopathology is considered to be the most important predictor, after FIGO staging [13-15]. However, sometimes even, nonmetastatic cancers with non-enlarged glands have poor outcome than would be expected in advanced stage disease for reasons not very well understood [13]. Also clinical early stage cases may actually turn out to be of advanced stage during surgery or after postoperative histopathology. So the research continues. An attempt was made to study the correlation between clinical, intraoperative and postoperative staging in cases of early stage cervical cancer in women who were planned for radical hysterectomy at the health facility with limited resources.
Methods and Materials
Study was done after taking institute’s ethics committee’s approval. The analysis of records of cervical cancer cases that were planned for radical hysterectomy over a period of almost 3 decades was done. During the period from April 1984- March 2012, a total 266 women underwent abdominal radical hysterectomy, 15 were for endometrial cancer so, 251 (94.36% of all radical hysterectomies) operable cases (Revised FIGO stage I A to I B1, II A1 [16]) of cervical cancer were the study subjects.
During the period of analysis, of 5, 62,740 admissions at the rural institute in central India (study site), 10,122 (1.79%) cases were of various cancers. Of cancer cases 5734 (56.64%) were in women, 1042 (18.20%) had cancer breast and 2516 (43.87%) had gynecological cancers. A total of 1923 had cervical cancer, (33.54% of cancers in women, 76.43% of all gynecological cancers). Of all cases of cervical cancer 13.05% were planned for radical hysterectomy, study subjects (Table 1).
| Block | Overall GYN. Cancer |
Cervical cancer | Radical hysterectomy | Total Radical hysterectomy for cervical cancer | Stage With Planned Radical Hysterectomy | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | % | % | IA | IB1 | IIA1 | ||||||
| No. | % | No. | % | No. | % | ||||||
| A | 133 | 110 | 82.70 | 31( 30+1*) | 96.77 | 4 | 13.33 | 5 | 16.66 | 21 | 70 |
| B | 170 | 135 | 79.41 | 19 | 100.00 | 5 | 26.31 | 4 | 21.05 | 10 | 52.63 |
| C | 182 | 130 | 71.42 | 19 | 100.00 | 5 | 26.31 | 6 | 31.57 | 8 | 42.10 |
| D | 351 | 286 | 81.48 | 40 (39+1*) | 97.50 | 11 | 28.20 | 10 | 25.64 | 18 | 46.15 |
| E | 428 | 326 | 76.16 | 41(38+3*) | 92.68 | 6 | 15.78 | 10 | 26.31 | 22 | 57.89 |
| F | 604 | 461 | 76.32 | 52 (46+6*) | 88.46 | 12 | 26.08 | 13 | 28.26 | 21 | 45.65 |
| G | 648 | 475 | 73.33 | 64(60+4*) | 93.75 | 18 | 30.00 | 20 | 33.33 | 22 | 36.66 |
| Total | 2516 | 1923 | 76.43 | 266(251+15*) | 94.36 | 61 | 24.30 | 68 | 27.09 | 122 | 48.60 |
| *Were done for endometrial cancer so were excluded | |||||||||||
Table 1: Block wise radical hysterectomy.
For analysis, these 251 cases were divided into 7 blocks of 4 years each (April to March), Block A 1984-1988(30) , Block B 1988-1992(19), Block C 1992-1996 (19), Block D 1996-2000 (39), Block E 2000-2004 (38) , Block F2004-2008(46) and Block G 2008-2012(64).
Results
There was an overall increase in cervical cancer cases. Operable cases also gradually increased (Table 1). The number of planned radical hysterectomies for stage IA increased from 13.33% (4 of the total 31 cases in Block A) to 30.00% (18 of 64 of all radical hysterectomies for stage IA in Block G) (significant difference, p<0.005).
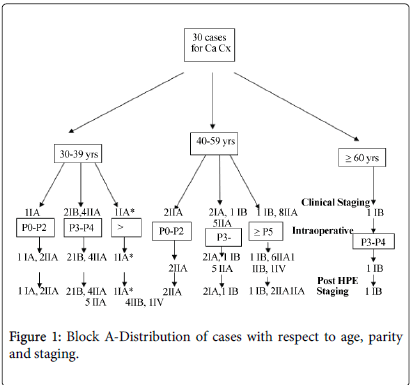
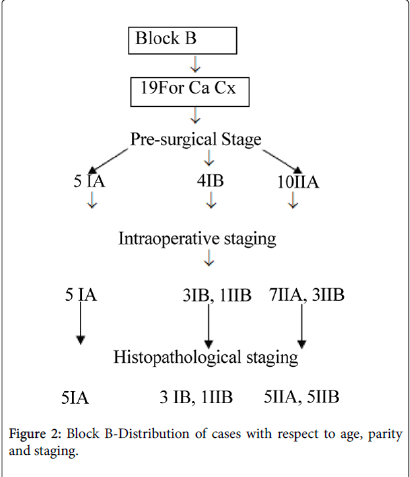
In Block A, all 4 women operated for stage IA, (A1,A2) continued to be of the same stage intraoperative and after histopathology of surgical specimen also, 5 cases operated for stage IB1, continued to be of the same stage intraoperative and postoperatively. Of 21 women operated for stage II A1, 19 (90.5%) remained II A1, one was IIB and one was IVA intraoperative. In Block B, 19 cases were planned for radical hysterectomy, of which 5 (26.31%) were for stage IA (A1,A2) remained IA, 4 for IB1, one was IIB intraoperative, confirmed histopathologically also and 10 (52.63%) were for stage IIA1, 3 (30%) were IIB during surgery, confirmed by histopathology also and in 2 other cases parametrial infiltration was not diagnosed during surgery but histopathology of surgical specimen revealed presence of disease, so in 5 of 10 (50% ) cases of IIA1, it was under staging .
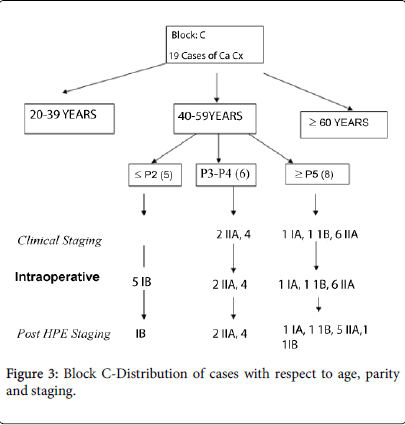
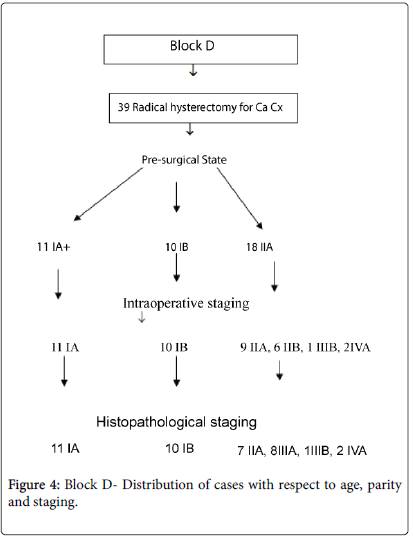
In Block C, 19 were for radical hysterectomy. Of 8 with IIA1, one had parametrial infiltration on histopathology, (staged IIB). In Block D, of 39 cases planned for surgery with stage IIA1, in two cases bladder involvement was diagnosed intraoperative (stage IV A) and hence procedure was abandoned. In Block E, of total 38 women planned, 22 (57.89%) were for stage IIA1, 11 (50.00%) of them continued to be of the same stage histopathologically and in 10 (45.50%) parametrial involvement was diagnosed histopathologically (IIB). (8 (36.40%) IIB, 2 (9.1%) IIIB) and in one (4.5%) of stage IIA1 intraoperative bladder involvement was detected (stage IVA) and hence procedure was abandoned. Of forty six cases planned for radical hysterectomy in Block F, of 12 (26.08%) of stage IA1, one (8.3%) turned out to be insitu cancer after postoperative histopathology. Of 13 (28.3%) operated for IB1, one (7.7%) had malignant mixed mullerian tumour (MMMT) and of 21 (45.60%) operated for IIA1 also, one (4.8%) was having MMMT on histopathology of operative specimen (Figures 1-4).
Overall of 251 women who were planned for radical hysterectomy, 61 (21.91%) were operated for stage IA, 68 (27.09%) stage IB1, 122 (48.60%) stage IIA1.On correlating clinical and intraoperative staging, of 55 cases clinically diagnosed as stage IA(A1+A2), 41 (74.54%) remained stage IA intraoperative also, 7 (12.72%) turned out to be IIA1 and 7 (12.72%) IIB. Of 68 women with clinical stage IB1, 53 (77.94%) remained of same stage intraoperative, 11 (16.17%) were IIA1 and 6(8.82%) IIB. Of 122 cases operated with clinical stage IIA1, intraoperative staging was IA in 3(2.45%), IB1 in 2 (1.63%), IIA1 in 88 (72.13%), IIB in 24 (19.67%), IIIB in 7 (5.73%) and 8 (6.55%) had stage IV A disease. So 28% women would not have been posted for surgery if they were known to be, of the stage they were found intraoperative, (clinical under staging of disease), over staging was only in 2% cases. On correlating clinical, surgical specimen histopathological staging it was revealed that of 55 clinical stage IA, 42 (76.36%)were confirmed as stage IA (A1,A2) , 7 (12.72%) were IIA1, 3 (5.45%) were IIB and three were in situ disease (5.45%). Of 68 with clinical stage IB1, 51 (75.00%) were confirmed as IB1, 11 (16.17%) IIA1 and 6 (8.82%) were of stage IIB. Of 122 cases with clinical stage IIA1, the staging was IA (A1,A2) in one, IB1 in two, 74 remained IIA1, 32 were IIB, 4 IIIB, 7 were IV A and two were MMMT. So over all 36% women would not have been opened up for surgery if their staging was known preoperatively.
Discussion
Cervical cancer is seventh in the frequency amongst overall cancers, third most common cancer among women worldwide, with an estimated 500,000 new cases diagnosed every year [9,10]. Attempts continue to be made for prevention and if cancer occurs, to provide the best of therapy for quality life and to prevent death for which appropriate staging is critical. Patients considered poor surgical candidates, because of their comorbidities like cardiac, pulmonary, and renal diseases, coagulopathy etc. are not operated even if these are in operable stage for obvious reasons. Many gynaecologic oncologists favour non-operative treatment in elderly patients also. Sixty-five years of age is cited as the limit for consideration of radical hysterectomy by some [17], however others have found morbidity and survival of older patients comparable to younger ones [18]. Thus, it seems prudent to determine whether a surgical approach is appropriate and safe, based on stage and risk factors independent of chronologic age. Diagnostic evaluation needs to be accurate. The International Federation of Gynecology and Obstetrics (FIGO) advocates clinical staging of cervical cancer based on physical examination and select, widely available diagnostic studies, such as cystoscopy, proctoscopy, intravenous urography, and X-ray of lungs and skeleton. It is also well known that clinical staging is frequently inaccurate. A substantial number of patients who undergo surgical treatment are found to have metastasis that upstage their disease [19,20] or occasionally downstage also. Years back Lapolla et al. [21] in their study involving ninety-six patients with cervical cancer with surgical staging, had reported that, 52% correlation existed between clinical and surgical staging. Winter et al. [22] report rate of parametrial involvement 18% even with FIGO staging IA and 28.5% in IIB. The researchers conclude that 18% of the so called stage I and 34% of the stage IIB had parametrial involvement histopathologically. In a retrospective study, Özsarlak et al. [23] have reported overall accuracy of clinical staging 47% in surgically– pathologically proven primary cases where study parameters for preoperative staging were the presence of tumour, extension into the parametrial tissue, pelvic wall, adjacent organs and lymph nodes and results were compared with histopathological findings. In the present study of women who were planned for radical hysterectomy on the basis of clinical staging, in 36%, the plans of surgical therapy could have been abandoned if their staging was known pre operatively. Whitney et al. [24] have reported that of 1127 patients with stage IB1 cervical cancer, ninety eight (8.7%) were found to have extra uterine disease at operation and the proposed radical operation was abandoned. The Cartwright Inquiry in New Zealand, in which research by two feminist journalists revealed that women with cervical abnormalities were not receiving treatment, as part of an experiment. The women were not told of the abnormalities and several later died. Improved imaging studies such as high-resolution computed tomography (CT), Magnetic Resonance Imaging (MRI), lymphangiography, and Positron Emission. Tomography (PET) may reveal extra uterine disease that cannot be cured with standard surgical techniques. However these radiographic studies are imperfect because they fail to detect micro metastasis which affect prognosis for surgical patients. A very important aspect is also that cervical cancer occurs in poor women, the cost of diagnostic techniques is very high, and it is essential to save the resources for the best therapy necessary. The nodal status is vitally important, both for prognosis and guiding adjuvant therapy. Various studies reveal an overall sensitivity of detecting metastatic disease 92% and a negative predictive value 97%. Results of large, multi-institutional studies in Europe and the United States should help guide the future direction for sentinel node technologies in the treatment of cervical cancer [25].
All said histopathology of the surgical specimen continues to provide information that is central for final treatment planning and prognosis for an individual patient.
The diagnostic aids make treatment costly which at times is not possible in rural settings like ours and also no diagnostic test today helps in diagnosis of micro metastasis. It was observed that between clinical staging and intraoperative staging, there was agreement in 72%. Histopathological staging which helps in planning the course of treatment agreed with clinical staging in around 64%. Low cost modalities for evaluation will help reducing morbidity and save resources.
Declaration of Interest
The authors report no declaration of interest
References
- Allen D, Narayan K (2005) Managing advanced stage cervical cancer. Best Practice and Research Clinical Obstetrics and Gynaecology, 19: 591-609.
- Kahesa C, Mwaiselage J, Wabinga HR, Ngoma T, KalyangoJN, et al (2008). Association between invasive cancer of the cervix and HIV 1 infection in Tanzania: the need for dual screening. BMC Public Health 8: 262.
- Sankaranarayanan R, Nair MK, Jayprakash PG (1995) Cervical cancer in Kerala: a hospital registry based study on survival and prognostic factors. British Journal of Cancer 72:1039-1042.
- Dasgupta S, Chakraborty SB, Roy A, Roychowdhury S, Panda CK (2003) Differential deletions of chromosome 3p are associated with the development of uterine cervical carcinoma in Indian patients. Molecular Pathology 56: 263-269.
- Nandakumar A, Ramnath T, Chaturvedi M (2009) The magnitude of cancer cervix in India. Indian Journal of Medical Research 130: 219-221.
- Murthy NS, Mathew A (1999) Screening for cancer of the uterine cervix and approaches adopted in India. Indian Journal of Cancer 36:154-162.
- Ananth R (2000) Downstaging of cervical cancer. Journal of Indian Medical Association 98:41-44.
- McGoogan E, Payne N, Chilcott J (2000) Liquid based cytology in cervical screening: a rapid and systematic review. Health Technology Assessment 4:1-73.
- Sobti RC, Shekari M, KordiTamandani DM, Kaur P, Suri V, et al. (2008) Effect of NBS1 gene polymorphism on the risk of cervix carcinoma in a northern Indian population. International Journal of Biological Markers 23: 133-139.
- Shekari M, Sobti RC, Tamandani DM, Malekzadeh K, Kaur P, et al. (2008) Association of genetic polymorphism of the DNA base excision repair gene (APE-1 Asp/148 Glu) and HPV type (16/18) with the risk of cervix cancer in north Indian population. Cancer Biomark 4:63-71.
- Chirenje ZM, Rusakaniko S, Kirumbi L, Ngwalle EW, Makuta-Tlebere P, et al. (2001) Situation analysis for cervical cancer diagnosis and treatment in east, central and southern African countries. Bull World Health Organ 79:127-132.
- Anorlu R (2008) Cervical cancer: the sub Saharan african perspective. Reproductive Health Matters 16: 41-49.
- Lukaszuk K, Liss J, Wozniak I, Sliwinski W, EmerichJ, et al. (2004) HPV and histological status of pelvic lymph node metastases in cervical cancer: a prospective study. Journal of Clinical Pathology 57: 472-476.
- Denschlag D, Gabriel B, Mueller Lantzsch C, Tempfer C, Henne K, et al. (2005) Evaluation of patients after extraperitoneal lymph node dissection for cervical cancer. Gynaecologic Oncology 96: 658-664.
- Ferrandina G, Distefano M, LudovisiM, Morganti A, SmaniottoD, et al. (2007) Lymph node involvement in locally advanced cervical cancer patients administered preoperative chemo radiation versus chemotherapy annals of surgical oncology. Society of Surgical Oncology 14:1129-1135.
- Pecorelli S (2009) Revised FIGO staging for carcinoma of the vulva cervix and endometrium. International Journal of Gynaecology& Obstetrics 105:103-104.
- Kleinberg MJ,Alvarrez RW (2004) Radical hysterectomy for carcinoma of uterine cervix.
- Mousavi A, KarimiZarchi M, Gilani MM (2008) Radical hysterectomy in the elderly.World Journal Surgical Oncology 6: 38.
- Shingleton HM,Bell MC, Fremgen A, Chmiel JS, Russell AH, et al. (1995) Is there really a difference in survival of women with squamous cell carcinoma adenocarcinoma and adenosquamous cell carcinoma of the cervix? International Journal of the American Cancer Society. 76: 1948-1955.
- Jain P,Goel A (2008) Clinical staging in carcinoma cervix:Does it correlate with pathological staging? Journal Clinical Oncology 26:16570
- LaPolla JP, Schlaerth JB, Gaddis O (1986) The influence of surgical staging on the evaluation and treatment of patients with cervical carcinoma. Gynecologic Oncology 24:194-206.
- Winter R (2001) Prognostic Factors in Surgically Treated Stage Ib-IIb Cervical Carcinomas with Special Emphasis on the Importance of Tumor. Gynaecologic Oncology 82: 11-16.
- Ozsarlak O. Tjalma. W, SchepensE,Corthouts B, Op de Beeck B, Van MarckE, et al. (2003) The correlation of preoperative CT MR imaging, and clinical staging(FIGO) with histopathology findings in primary cervical carcinoma . European Radiology 13:2338-2345.
- Whitney CW, Sause W, Bundy BN, Malfetano (1999) Randomized comparison of fluorouracil plus cisplatin versus hydroxyl urea as an adjunct to radiation therapy in stage IIB-IVA carcinoma of the cervix with negative para-aortic lymph nodes: a Gynecologic Oncology Group and Southwest Oncology Group study. Journal of Clinical Oncology 17: 1339-1348.
- Frumovitz M, Ramirez PT, Levenback CF (2008) Lymphatic mapping and sentinel lymph node detection in women with cervical cancer.Gynaecologic Oncology 110: S17-20.
Relevant Topics
- Breast Cancer Surgery
- Colon Cancer Surgery
- Dermatologic Surgery
- Kidney Cancer Surgery
- Leukemia Surgery
- Lung Cancer Surgery
- Lymphoma Surgery
- Oesophageal Cancer Surgery
- Pancreatic Cancer Surgery
- Prostate Cancer Surgery
- Radiation Therapy
- Skin Cancer Surgery
- Stomach Cancer Surgery
- Throat Cancer Surgery
- Thyroid Cancer Surgery
Recommended Journals
Article Tools
Article Usage
- Total views: 12355
- [From(publication date):
June-2016 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 11410
- PDF downloads : 945