Research Article Open Access
Staging Hepatocellular Carcinoma with Gadolinium-Ethoxybenzyl Diethylenetriaminepentaacetic Acid -Enhanced Magnetic Resonance Imaging: A Comparison with Multi-Detector Row Computed Tomography
Jingjing Fu1, Jun Zhao2, Xiaochun Zhang2, Xuesong Li3, Li Xiaoming2 and Lin Zhang2*
1College of Nursing, Third Military Medical University, Chongqing, China
2Department of Radiology, Southwest Hospital, Third Military Medical University, Chongqing, China
3Institute of Hepatobiliary Surgery, Southwest Hospital, Third Military Medical University, Chongqing, China
- *Corresponding Author:
- Lin Zhang
Department of Radiology
Southwest Hospital, Third Military Medical University
29 Gaotanyan St., District Shapingba
Chongqing, 400038, China
Tel: +86-23-6875-4425
Fax: +86-23-6546-3026
E-mail: linzhangswh@yahoo.com
Received Date: March 29, 2016; Accepted Date: May 17, 2016; Published Date: May 20, 2016
Citation: Fu J, Zhao J, Zhang X, Li X, Xiaoming L, et al. (2016) Staging Hepatocellular Carcinoma with Gadolinium-Ethoxybenzyl Diethylenetriaminepentaacetic Acid -Enhanced Magnetic Resonance Imaging: A Comparison with Multi-Detector Row Computed Tomography. OMICS J Radiol 5:222. doi:10.4172/2167-7964.1000222
Copyright: © 2016 Fu J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use,distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Radiology
Abstract
Aim: To explore if gadolinium-ethoxybenzyl-diethylenetriaminepentaacetic acid (Gd-EOB-DTPA)-enhanced MRI provides more accurate information than multi-detector row computed tomography (MDCT) for staging hepatocellular carcinoma (HCC).
Methods: We retrospectively investigated 112 patients with HCC who underwent MDCT and Gd-EOB-DTPA enhanced MRI within one month before treatment. Two experienced radiologists reviewed the size, number, and boundaries of the HCC lesions, portal invasion, and tumor metastasis on MDCT and MRI images in consensus. Then the performance of Gd-EOB-DTPA-enhanced MRI and MDCT on staging HCC lesions was compared through statistical analysis. The classification of the Barcelona Clinic Liver Cancer (BCLC) stage was also evaluated.
Results: HCC lesions in five patients were detected on Gd-EOB-DTPA-enhanced MRI only. Of the other 107 patients, 21 (19.6%) were in BCLC stage 0, 49 (45.8%) in BCLC stage A, 14 (13.1%) in BCLC stage B, and 23 (21.5%) in BCLC stage C on MDCT. On Gd-EOB-DTPA-enhanced MRI, 12 (11.2%), 48 (44.9%), 17 (15.9%), and 30 (28.0%) patients were classified as BCLC stages 0, A, B, and C, respectively. The two methods differed significantly in staging HCC patients (χ2=16.444, P=0.006).
Conclusion: This study suggests that Gd-EOB-DTPA-enhanced MRI provides more accurate information than MDCT for characterizing and staging HCC which will help to choose accurate treatment strategy.
Keywords
Hepatocellular carcinoma; Gadolinium-ethoxybenzyldiethylenetriaminepentaacetic acid; Multidetector row computed tomography; Barcelona clinic liver cancer stage
Abbreviations
BCLC: Barcelona Clinic Liver Cancer; MRI: Magnetic Resonance Imaging; HCC: Hepatocellular Carcinoma; LT: Liver Transplantation; MDCT: Multidetector Row Computed Tomography; RFA: Radiofrequency Ablation; TACE: Transarterial Chemoembolization
Introduction
Hepatocellular carcinoma (HCC) accounts for 85%–90% of primary liver cancers [1]. HCC-related mortality can be reduced by its early detection and the application of potentially curative treatments, including resection, liver transplantation (LT), and radiofrequency ablation (RFA) [2]. Various morphological factors need to be considered, including the type, nodular or infiltrative, the number of lesions, their size, their anatomical relationships and loco-regional and extra-hepatic extension [3]. Once HCC is diagnosed, the lesions are staged, together with the clinical condition of the patient, the most appropriate treatment strategy will be determined in each case [4].
Gd-EOB-DTPA is a liver-specific hepatocyte magnetic resonance (MR) T1-enhanced agent that allows lesion characterization and the definition of the tumor–vascular relationship [5]. To date, Gd-EOBDTPA- enhanced MR imaging (MRI) has been shown to be largely superior to unenhanced MRI, computed tomography (CT), and other types of contrast agents for the detection and characterization of liver lesions [6,7], especially small HCCs [8]. However, little research has compared the effects of Gd-EOB-DTPA-enhanced MRI and multidetector row computed tomography (MDCT) in staging HCC [9,10], with few data available on the differences between Gd-EOB-DTPA enhanced MRI and MDCT in identifying BCLC stages B and C. In this article, we will explore the difference in staging of HCC between Gd- EOB-DTPA-enhanced MRI and MDCT according to BCLC stages.
Patients and Methods
Patients
This study was conducted with the approval of The Institutional Review Board of southwest hospital. Informed consent was not required for this retrospective study. Patient records/information was anonymized and de-identified prior to analysis. Between January 2012 and November 2013, 119 patients who were initially diagnosed with HCC at our hospital were consecutively enrolled in this study. All lesions in the patients’ livers were evaluated with MDCT and Gd-EOBDTPA- enhanced MRI (Figure 1).
Of these 119 HCC patients, two were excluded because the interval between the two examinations exceeded one month. Five patients were excluded because there were no results for the pathological examination or adequate follow-up. Finally, 41 patients (92 HCC lesions) with follow-up results and 71 HCC patients (165 HCC lesions) with pathological examination results were enrolled in the study. The follow-up period was between 6 months and 2 years. 92 lesions seen in follow up met the American Association for the Study of Liver Diseases (AASLD) guideline in follow up examination [11,12]. All the HCC lesions were confirmed to correspond to identify by previous CT or MRI.
MDCT Image Acquisition
Multiphase CT scanning was acquired with a MDCT scanner (Somatom Sensation 16, Siemens, Munich, Germany). The scanning parameters were as follows: 120 kVp, 240 mAs, 5 mm slice thickness with an increment (overlap) of 2.5 mm, table speed of 26.5–39.37 mm/ rotation (pitch, 0.828–1.07), and a single-breath-hold helical acquisition of 14–16 s. Hepatic arterial phase scanning began 30–40 s after the injection of 80– 100 mL of a nonionic iodinated contrast agent (iopromide injection 370 mgl/ml; Bayer Schering Pharma AG, Berlin, Germany) at a rate of 3–5 mL/s with a bolus-triggered technique (120 kVp; 40–60 mA; monitoring frequency from 12 s after the injection of 100 HU of contrast agent into the abdominal aorta; delay from trigger to initiation of scan, 18 s). The contrast agent was administered through the antecubital vein with a power injector (ulrich medical USA® Missouri editon 094). The portal and equilibrium phases of scanning began 70 s and 180 s after the injection of the contrast agent, respectively.
MR Image Acquisition
Gd-EOB-DTPA-enhanced MRI (3.0 tesla MRI; Trio Tim, Siemens, Munich, Germany) was performed using the liver-specific hepatocytedirected MRI contrast agent Gd-EOB-DTPA (Primovist; Bayer Schering Pharma AG, Berlin, Germany). Briefly, Gd-EOB-DTPA solution (0.1 mL/kg bodyweight) was injected at a speed of 1–2 mL/s through an intravenous line placed in the antecubital vein with a power injector (Medrad®, Indianola, PA, USA), followed by a flush with 20–30 mL of 0.9% normal saline. A multiphasic dynamic study was performed using three-dimensional T1-weighted gradient-echo (TR/TE/FA: 3.42 ms/1.25 ms/9°; matrix size: 224 × 168; field of view: 400 mm). Care bolus was used for the dynamic enhancement of MRI in the arterial phase. When the contrast agent reached the level of the aorta abdominalis segment, each patient was asked to hold breath and arterial phase scanning was conducted. Portal- and equilibrium-phase images were also obtained at 50–80 s and 180 s after injection, respectively. T1-weighted images with fat suppression were repeated 20 min after injection, as the hepatobiliary-phase images.
Image Analysis and BCLC staging
The size, number, and boundaries of the HCC lesions, portal invasion, and tumor metastasis on the MDCT, Gd-EOB-DTPAenhanced MRI images were all reviewed by two radiologists followed by a consensus reading. Both (L.Z. and X.Z.) had at least ten years of professional experience at interpreting abdominal CT and MR images, and both were blinded to the clinical histories and final diagnoses. Image interpretation was conducted in two sessions: During session 1, the CT images of all patients were analyzed. During session 2, the MRI images of all patients were analyzed. More than 1 week of time interval was set between the reading sessions of CT and MR images to reduce recall bias. The sizes of the tumor lesions detected with MDCT or Gd- EOB-DTPA-enhanced MRI were recorded as the literature reports [13]. The diagnostic criteria for HCC on MDCT were applied according to the most recent AASLD guideline, updated in 2011 [14]. The diagnostic criteria for HCC on Gd-EOB-DTPA-enhanced MRI were any three of four imaging findings (arterial-phase hyperintensity, portal or delayed washout, hyperintensity on T2-weighted images, and hepatobiliary-phase hypointensity) proposed in a previous study [15].
All patients were staged carefully according to the BCLC staging system, which has been approved by the European Association for the Study of the Liver and the AASLD [16,17]. After MDCT images analysis was performed, two radiologists and one surgeon (X.L. with ten years’ clinical HCC surgeon experience) assessed the stage of each HCC patient accorded with the BCLC staging system. The second decision was made in the same way after Gd-EOB-DTPA-enhanced MRI [18-20]. More than 1 week of time interval was set between the reading sessions of CT and MR images to reduce recall bias.
Statistical Analysis
Differences between categorical variables and staging methods were analyzed with a paired χ2 test. The differences in the total lesion numbers, lesion sizes, and single or multiple lesions were analyzed statistically with a χ2 test (means of the Wilcoxon signed-rank test, Fisher’s exact test, or a paired χ2 test). A value of P<0.05 was considered statistically significant. The software used for all analyses was SPSS (version 13; SPSS, Inc., Chicago, IL, USA).
Results
Baseline characteristics of patients
The baseline characteristics of the 112 patients were summarized in Table 1. There were 100 (89.3%) males and 12 (10.7%) females in the study. The median patient age was 50.5 years (range, 27–74 years). Of the 112 patients enrolled, 93 patients (83.0%) were Child–Pugh class A, 18 (16.1%) were Child–Pugh class B, and only one (0.9%) patient was Child–Pugh class C. The median α-fetoprotein concentration in the cohort was 58.0 ng/mL (range, 1.1–16.7 × 104 ng/mL). Fourteen (12.5%) patients had no history of hepatitis, 95 (84.8%) patients had hepatitis B, and three (2.7%) patients had hepatitis C. Half the 112 patients had a history of liver cirrhosis.
| Variable | Total |
|---|---|
| Sex (male/female), n (%) | 100/12 (89.3/10.7) |
| Age (years)a | 50.5 (27–74) |
| History of hepatitis, n (%) | |
| No/B/C | 14/95/3 (12.5/84.8/2.7) |
| Liver cirrhosis (yes/no), n (%) | 56/56 (50.0/50.0) |
| a-Fetoprotein (ng/mL)a | 58.0 (1.1–16.7 ´ 104) |
| ALT (IU/L)a | 43 (10–624) |
| AST(IU/L)a | 44 (19–898) |
| Albumin (g/L)a | 43 (23.5–87.7) |
| Total bilirubin (mmol/l)a | 18 (6.7–516.6) |
| Creatinine (mg/dL)a | 73 (14.2–146.0) |
| Prothrombin time (INR)a | 12.6 (10.5–17.7) |
| Child-Pugh Class, n (%) | |
| A/B/C | 93/18/1 (83.0/16.1/0.9) |
| PST, n (%) | |
| 0/1/2 | 34/70/8(30.4/62.5/7.1) |
| ALT: Alanine Transaminase; AST: Aspartate Transaminase; INR: International Normalized Ratio; PST: performance status. aMedian (range) | |
Table 1: Baseline clinical characteristics of 112 patients with HCC.
Characteristic HCC lesions detected with MDCT and Gd- EOB-DTPA-enhanced MRI
According to the statistical analysis, the total numbers of HCC lesions detected by the two imaging tests were significantly different (χ2=59.093, P<0.001). The two imaging methods differed significantly in the size of the HCC lesions detected (χ2=17.429, P<0.001). They also differed significantly in detecting whether the lesions were single or multiple (χ2=17.152, P<0.001). The enhancement patterns of the HCC lesions detected with the two imaging methods were also significantly different (χ2=53.706, P<0.001, Table 2). Six HCC lesions in five patients were detected with MRI but not with MDCT, and the mean diameter of these six lesions was 12.4 mm (range, 7–15 mm).
| Variable | MDCT | Gd-EOB-DTPA-enhanced MRI | χ2 | P value |
|---|---|---|---|---|
| Lesion number (n) | 204 | 257 | 59.093 | 0.000* |
| Lesion number in each patient (n) | 21.333 (17.152) | 0.000* (0.000*) | ||
| Single lesions | 70 (70) | 45 (45) | ||
| Multiple lesions | 37 (134) | 62 (212) | ||
| Size (lesions, n) | 9.577 (17.429) | 0.002* (0.000*) | ||
| <15 mm | 22 (26) | 53 (74) | ||
| ≥ 15 mm | 106 (178) | 106 (182) | ||
| Enhancement pattern (lesions, n) | 53.706 | 0.000* | ||
| Wash in/out | 204 | 198 | ||
| No wash in/out | 0 | 59 | ||
| *Statistically significant results (P<0.05).(The five patients without HCC lesions on MDCT were notincluded in Table 2). | ||||
Table 2: Characteristics of HCC lesions detected with MDCT and Gd- EOB-DTPA-enhanced MRI.
Changes in BCLC stages after Gd-EOB-DTPA-enhanced MRI versus MDCT
The five (4.46%) patients who were not diagnosed with HCC on MDCT were found to have HCC on Gd-EOB-DTPA-enhanced MRI; four of them were classified as BCLC stage 0 and one as BCLC stage A on MRI. Of the remaining 107 patients, 21 (19.6%) were classified with BCLC stage 0, 49 (45.8%) with BCLC stage A, 14 (13.1%) with BCLC stage B, and 23 (21.5%) with BCLC stage C on MDCT. However, after they were evaluated with Gd-EOB-DTPA-enhanced MRI, 12 (11.2%), 48 (44.9%), 17 (15.9%), and 30 (28.0%) patients were classified with BCLC stages 0, A, B, and C, respectively. The staging of HCC with the two imaging methods differed significantly on paired χ2 test (χ2=16.444, P=0.006; five patients without HCC on MDCT were not included).
After combining the characteristics and staging of the patients (Table 3), we found that MDCT and Gd-EOB-DTPA-enhanced MRI differed significantly in evaluating BCLC B patients with multiple lesions (χ2=9.464, P=0.002). They also differed significantly in staging BCLC B patients with lesions of <15 mm (χ2=5.783, P=0.016) and BCLC C patients with lesions of 15 mm (P=0.034). However, the two imaging methods did not differ significantly in evaluating HCC patients with single lesions (P>0.05).
| Variable | MDCT | Gd-EOB-DTPA-enhanced MRI | χ2 | P value |
|---|---|---|---|---|
| Single | ||||
| BCLC 0 | 21 | 12 | 0.149 | 0.700 |
| BCLC A | 42 | 28 | 0.057 | 0.812 |
| BCLC C | 7 | 5 | 0.000 | 1.000 |
| Multiple | ||||
| BCLC A | 8 (18) | 20 (43) | 1.292 (2.653) | 0.256 (0.103) |
| BCLC B | 13 (56) | 17 (55) | 0.653 (9.464) | 0.419 (0.002*) |
| BCLC C | 16 (60) | 25 (114) | 0.081 (2.659) | 0.775 (0.103) |
| < 15 mm | ||||
| BCLC 0 | 1 (1) | 1 (1) | — | 0.503 (0.454) |
| BCLC A | 1 (1) | 12 (12) | 2.402 (1.624) | 0.121 (0.203) |
| BCLC B | 11 (15) | 15 (23) | 3.232 (5.783) | 0.072 (0.016*) |
| BCLC C | 9 (9) | 25 (38) | 0.246 (2.163) | 0.620 (0.141) |
| ≥15 mm | ||||
| BCLC 0 | 20 (20) | 11 (11) | 3.060 (3.083) | 0.080 (0.079) |
| BCLC A | 48 (55) | 48 (59) | 0.000 (0.096) | 1.000 (0.757) |
| BCLC B | 15 (45) | 17 (33) | 0.147 (2.710) | 0.701 (0.100) |
| BCLC C | 23 (58) | 30 (79) | 1.233 (4.471) | 0.267 (0.034*) |
| *Statistically significant results (P<0.05). | ||||
Table 3: HCC stages according to MDCT and Gd-EOB-DTPAenhanced MRI. The treatments
Changes in therapeutic decisions after Gd-EOB-DTPAenhanced MRI
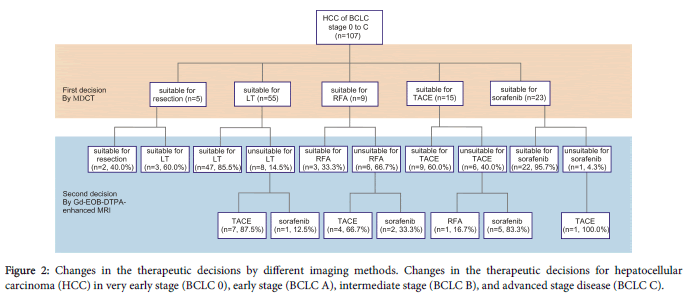
After MDCT (Figure 2), five (4.7%) of the 107 HCC patients were considered eligible for surgical resection, 55 (51.4%) for LT, nine (8.4%) for RFA, 15 (14.0%) for TACE, and 23 (21.5%) for sorafenib. However, the second round of imaging with Gd-EOB-DTPA-enhanced MRI resulted in marked changes in the therapeutic decisions.
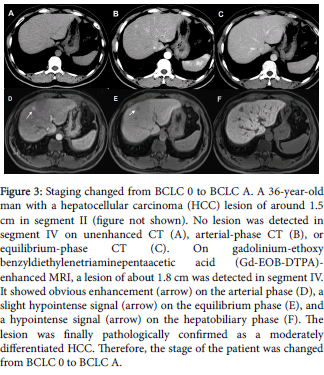
Three (60.0%) of the five patients eligible for surgical resection became eligible for LT because additional HCC lesions were detected in these patients (Figure 3). Fifty-five patients were considered eligible for LT on MDCT, but the therapy recommended was altered for eight (14.5%) of them after the second round of imaging: seven (87.5%) for TACE, one (12.5%) for sorafenib because portal invasion or extrahepatic metastasis was detected.
Figure 3: Staging changed from BCLC 0 to BCLC A. A 36-year-old man with a hepatocellular carcinoma (HCC) lesion of around 1.5 cm in segment II (figure not shown). No lesion was detected in segment IV on unenhanced CT (A), arterial-phase CT (B), or equilibrium-phase CT (C). On gadolinium-ethoxy benzyldiethylenetriaminepentaacetic acid (Gd-EOB-DTPA)- enhanced MRI, a lesion of about 1.8 cm was detected in segment IV. It showed obvious enhancement (arrow) on the arterial phase (D), a slight hypointense signal (arrow) on the equilibrium phase (E), and a hypointense signal (arrow) on the hepatobiliary phase (F). The lesion was finally pathologically confirmed as a moderately differentiated HCC. Therefore, the stage of the patient was changed from BCLC 0 to BCLC A.
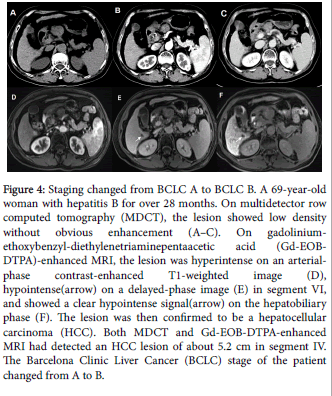
The number of patients who were eligible for RFA on MDCT decreased from nine to three (33.3%) after the second round of imaging; of the six (66.7%) remaining patients, four (66.7%) became eligible for TACE (Figure 4) and two (33.3%) for sorafenib. The 15 patients eligible for TACE on MDCT decreased to nine (60.0%) after the second round of imaging; RFA was suitable for one (16.7%) patient and sorafenib for five (83.3%) patients. Of the 23 patients considered eligible for sorafenib on MDCT, only one (4.3%) became eligible for TACE after Gd-EOB-DTPA-enhanced MRI. On paired χ2 tests, the therapeutic decisions made after each detection method differed significantly (χ2=17.467, P=0.015).
Figure 4: Staging changed from BCLC A to BCLC B. A 69-year-old woman with hepatitis B for over 28 months. On multidetector row computed tomography (MDCT), the lesion showed low density without obvious enhancement (A–C). On gadoliniumethoxybenzyl- diethylenetriaminepentaacetic acid (Gd-EOBDTPA)- enhanced MRI, the lesion was hyperintense on an arterialphase contrast-enhanced T1-weighted image (D), hypointense(arrow) on a delayed-phase image (E) in segment VI, and showed a clear hypointense signal(arrow) on the hepatobiliary phase (F). The lesion was then confirmed to be a hepatocellular carcinoma (HCC). Both MDCT and Gd-EOB-DTPA-enhanced MRI had detected an HCC lesion of about 5.2 cm in segment IV. The Barcelona Clinic Liver Cancer (BCLC) stage of the patient changed from A to B.
The treatments for the five patients without HCC on MDCT were altered to accord with the change in their BCLC stages after Gd-EOBDTPA- enhanced MRI: three were eligible for resection and two for LT. Though the actual treatment therapy differed with the BCLC therapeutic decisions to some extent.
Discussion
Our study showed that MDCT and Gd-EOB-DTPA-enhanced MRI differ significantly in the staging of HCCs. For patients with multiple lesions, more lesions were detected with Gd-EOB-DTPA-enhanced MRI than with MDCT in nearly all stages, especially in BCLC stage B, in which the difference was significant. This may be because Gd-EOBDTPA- enhanced MRI detected more lesions in most patients. Consequently, early- or very-early-stage patients with single lesions were reclassified as intermediate- or advanced-stage patients with multiple lesions. For patients with lesions of <15 mm, there was also a significant difference between the two imaging methods in correctly evaluating BCLC stage B. For patients with lesions >15 mm, the staging of BCLC stage C differed significantly with the two imaging methods. Gd-EOB-DTPA-enhanced MRI tended to find more small and multiple lesions, therefore classifying the patients to a later stage.
Disease staging is particularly important in the management of HCC because it helps to predict prognosis and determine appropriate treatment options [21]. Several recent studies [9,10] have considered whether Gd-EOB-DTPA-enhanced MRI is better than MDCT in differentiating stages BCLC 0 and BCLC A in HCC patients eligible for curative treatments. In this study, patients with stages BCLC B and BCLC C were also included. The addition of Gd-EOB-DTPA-enhanced MRI after MDCT was also essential for the accurate evaluation of patients with BCLC stage B and BCLC stage C.
The current European Guidelines endorse the BCLC algorithm for treatment decisions [22]. Generally speaking, surgical treatment is the gold standard for tumors of small dimensions and patients with a good functional liver reserve while liver transplantation is indicated for patients with a compromised hepatic function [23]. Patients who are inoperable due to the presence of comorbidities and insufficient liver function reserve can be considered candidates for percutaneous ablation [24]. The treatment therapy of HCC depends on the tumor stage, patient performance status, liver function reserve, life expectancy and other realistic factors. So the final treatment decisions for the individual patient should be reached by an interdisciplinary team [22]. In China, patients develop HCC mainly on the basis of hepatitis B cirrhosis with poor liver function, and the degree of liver cirrhosis is high. Besides, HCC patients often drop out the treatment of liver transplantation due to the scarcity of donors. Therefore, the treatment therapy for HCC patients may not strictly follow the BCLC algorithm, RFA or TACE may be chosen more frequently instead.
This study had some limitations. Although the BCLC system obviously offers guidelines, the final decision must be made based on each patient’s specific clinical condition [25]. So we didn’t care for the final treatment decisions compared with the two imaging methods. Another limitation is that the number of the patients enrolled in the study was small and it was performed retrospectively, which was likely to contain bias. Besides, further study of the long term outcome/ follow-up of the patients that had changed in staging is also limited. To our knowledge, there has been no predictive study comparing the efficacy of Gd-EOB-DTPA-enhanced MRI and MDCT in staging HCC. Therefore, a prospective study with a larger number of patients is required to verify our results.
This study suggests that Gd-EOB-DTPA-enhanced MRI not only evaluates the stages of early HCC more reliably than MDCT, but also differed in the staging of intermediate and advanced HCC which will help the clinical to choose more accurate therapeutic decisions for HCC patients.
References
- El-Serag HB, Rudolph KL (2007) Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology 132: 2557-2576.
- Tremosini S, Bruix J (2011) Diagnosis of Early Hepatocellular Carcinoma_ Ideal Goal, But Not Yet There. Gstroenterology 140: 358-360.
- Aubé C, Bouvier A, Lebigot J, Vervueren L, Cartier V, et al. (2015) Radiological treatment of HCC: Interventional radiology at the heart of management. DiagnInterv Imaging 96: 625-636.
- Vilana R, Forner A, García Á, Ayuso C, Bru C (2010) Hepatocellular Carcinoma: Diagnosis, staging, and treatment strategy. Radiología 52: 385-398.
- Huppertz A, Balzer T, Blakeborough A, Breuer J, Giovagnoni A, et al. (2004) Improved detection of focal liver lesions at MR imaging: multicenter comparison of gadoxetic acid-enhanced MR images with intraoperative findings. Radiology 230: 266-275.
- Akai H, Kiryu S, Matsuda I, Satou J, Takao H, et al. (2011) Detection of hepatocellular carcinoma by Gd-EOB-DTPA-enhanced liver MRI: comparison with triple phase 64 detector row helical CT. Eur J Radiol 80: 310-315.
- Chanyaputhipong J, Low SC, Chow PK (2011) Gadoxetate Acid-Enhanced MR Imaging for HCC: A Review for Clinicians. Int J Hepatol 2011: 489342.
- Sano K, Ichikawa T, Motosugi U, Sou H, Muhi AM, et al. (2011) Imaging study of early hepatocellular carcinoma: usefulness of gadoxetic acid-enhanced MR imaging. Radiology 261: 834-844.
- Jin YJ, Nah SY, Lee JW, Lee JI, Jeong S, et al. (2013) Utility of adding Primovist magnetic resonance imaging to analysis of hepatocellular carcinoma by liver dynamic computed tomography. ClinGastroenterolHepatol 11: 187-192.
- Yoo SH, Choi JY, Jang JW, Bae SH, Yoon SK, et al. (2013) Gd-EOB-DTPA-enhanced MRI is better than MDCT in decision making of curative treatment for hepatocellular carcinoma. Ann SurgOncol 20: 2893-2900.
- Forner A, Llovet JM, Bruix J (2012) Hepatocellular carcinoma. The Lancet 379: 1245-1255.
- Hennedige T, Venkatesh SK (2013) Imaging of hepatocellular carcinoma: diagnosis, staging and treatment monitoring. Cancer Imaging 12: 530-547.
- An C, Choi GH, Lee HS, Kim MJ (2012) Assessment of preoperative magnetic resonance imaging staging in patients with hepatocellular carcinoma undergoing resection compared with the seventh American Joint Committee on Cancer System. Invest Radiol 47: 634-641.
- Bruix J, Sherman M (2011) Management of hepatocellular carcinoma: an update. Hepatology 53: 1020-1022.
- Kim TK, Lee KH, Jang HJ, Haider MA, Jacks LM, et al. (2011) Analysis of gadobenatedimeglumine-enhanced MR findings for characterizing small (1-2-cm) hepatic nodules in patients at high risk for hepatocellular carcinoma. Radiology 259: 730-738.
- Bruix J, Sherman M, Llovet JM, Beaugrand M, Lencioni R, et al. (2001) Clinical management of hepatocellular carcinoma. Conclusions of the Barcelona-2000 EASL conference. European Association for the Study of the Liver. J Hepatol 35: 421-430.
- Bruix J, Sherman M, Practice Guidelines Committee AAftSoLD (2005) Management of hepatocellular carcinoma. Hepatology 42: 1208-1236.
- Bargellini I (2012) Hepatocellular carcinoma: MR staging and therapeutic decisions. Abdom Imaging 37: 231-238.
- de Lope CR, Tremosini S, Forner A, Reig M, Bruix J (2012) Management of HCC. J Hepatol 56: S75-S87.
- Jihye C, Jinsil S (2012) Application of Radiotherapeutic Strategies in the BCLC-Defined Stages of Hepatocellular Carcinoma. Liver Cancer 1: 216-225.
- Wong R, Frenette C (2011) Updates in the management of hepatocellular carcinoma. GastroenterolHepatol (N Y) 7: 16-24.
- Schutte K, Schulz C, Malfertheiner P (2014) Hepatocellular Carcinoma: Current Concepts in Diagnosis, Staging and Treatment. GastrointestTumors 1: 84-92.
- Llovet JM, Bruix J (2008) Novel advancements in the management of hepatocellular carcinoma in 2008. J Hepatol 48: S20-S37
- Rossi L, Zoratto F, Papa A, Iodice F, Minozzi M, et al. (2010) Current approach in the treatment of hepatocellular carcinoma. World J GastrointestOncol 2: 348-359.
- Forner A, Reig ME, de Lope CR, Bruix J (2010) Current strategy for staging and treatment: the BCLC update and future prospects. Semin Liver Dis 30: 61-74.
Relevant Topics
- Abdominal Radiology
- AI in Radiology
- Breast Imaging
- Cardiovascular Radiology
- Chest Radiology
- Clinical Radiology
- CT Imaging
- Diagnostic Radiology
- Emergency Radiology
- Fluoroscopy Radiology
- General Radiology
- Genitourinary Radiology
- Interventional Radiology Techniques
- Mammography
- Minimal Invasive surgery
- Musculoskeletal Radiology
- Neuroradiology
- Neuroradiology Advances
- Oral and Maxillofacial Radiology
- Radiography
- Radiology Imaging
- Surgical Radiology
- Tele Radiology
- Therapeutic Radiology
Recommended Journals
Article Tools
Article Usage
- Total views: 11341
- [From(publication date):
June-2016 - Jul 12, 2025] - Breakdown by view type
- HTML page views : 10434
- PDF downloads : 907