Stable versus Unstable Grade 2 High Ankle Sprains in Athletes: A Noninvasive Tool to Predict the Need for Surgical Fixation
Received: 25-Oct-2017 / Accepted Date: 12-Dec-2017 / Published Date: 09-Jan-2018 DOI: 10.4172/2329-910X.1000252
Abstract
There are no standardized criteria for the diagnosis and management of syndesmotic injuries, creating great ambiguity regarding optimal treatment. Traditionally, individuals with clinical and/or radiological suspicion of syndesmotic instability warrant an examination under anaesthesia and/or diagnostic arthroscopy to confirm and treat. Our purpose was to identify clinical syndesmotic instability without the need of invasive arthroscopic procedures. However, the invasive process of this has inherent risks to the patient. We developed a device to dynamically evaluate the distal tibiofibular stability during external rotation of the ankle as an extension to the available clinical tests. We compared the results of this device with intra-operative arthroscopic findings in 15 athlete cases with isolated grade 2 syndesmotic instability and found very good correlation, especially when tested in dorsiflexion. We consider this syndhoo device very helpful as part of the available options in the clinical diagnosis of syndesmotic instability.
Keywords: Ankle sprains; Arthroscopy; Syndesmotic injuries; Chronic syndesmotic instability
Introduction
Syndesmotic injuries, or high ankle sprains, comprise 10% of all ankle sprains [1]. These injuries are frequently sustained during athletic competition, particularly soccer [1,2]. However, as imaging studies suggest that up to 20% of acute ankle sprains involve the syndesmosis, the prevalence of syndesmotic injuries may be underestimated [3,4]. Syndesmotic injuries often require twice as long to return to sport as compared to isolated lateral ligament sprains and can lead to prolonged pain and disability [5-8]. Further, the most common cause of chronic ankle dysfunction 6 months from an ankle trauma, is related to syndesmotic injuries [7]. Recurrent and undiagnosed ankle instability is known to ensue and eventually lead to premature ankle arthritis [9]. Therefore, a timely diagnosis of unstable syndesmotic injuries is essential.
A rapid pivoting and forced ankle dorsiflexion of the ankle with a forceful external rotation and pronation of the foot, is the most common mechanism of a high ankle sprain [10]. Planovalgus foot alignment, high competitive sports level and male gender are potential risk factors [9,11,12].
As the talus rotates in the mortise, the fibula rotates externally and moves posteriorly and laterally. This mechanism then separates the distal tibia and fibula and sequentially tears the AITFL, deep deltoid ligament (or causes a malleolar fracture), the Inferior Oblique Ligament (IOL), and finally the Posterior Inferior Talo-fibular Ligament (PITFL) [10,13]. When there is a combined syndesmotic injury with a deltoid ligament disruption, talar instability occurs [14].
Less commonly, the injury may occur in forced dorsiflexion without rotation since the anterior part of the talus is wider than the posterior part. The magnitude and duration of force application appear to be predictive factors of lesion severity [9].
Syndesmotic injuries are classified in 3 grades, ranging from a partially torn AITFL to a complete disruption of all ligaments with mortise widening [15].
Purpose
There are no standardized criteria for the diagnosis and management of syndesmotic injuries, creating great ambiguity regarding optimal treatment. Our purpose is to identify clinical syndesmotic instability without the need of invasive arthroscopic procedures.
Methods
The described device is developed in close collaboration between our Center’s surgery and physiotherapy departments to identify syndesmotic instability necessitating (mini) open reduction and internal fixation. In our study, a grade 2 isolated syndesmotic injury is defined as a lesion to the antero-inferior tibiofibular ligament and the interosseous ligament of the ankle with involvement of the deltoid ligament on Magnetic Resonance scanning (MRI). We tested 15 registered athletes between the age of 18-36 years old, who presented with a grade 2 isolated syndesmotic injury (confirmed on MRI) between 1 january 2015 and 1 May 2017. All 15 athletes were independently tested by an experienced physiotherapist with the syndhoo device that we developed. They all had a grade 2 isolated syndesmotic injury with clinical and radiological signs of potential instability and therefore all were indicated for arthroscopy [15]. For every syndhoo-tested athlete, an arthroscopy was performed by 1 experienced ankle surgeon at our Center between January 2017 and September 2017. During arthroscopy, the syndesmosis was considered positive (unstable) if a 4.5 mm arthroscopic shaver could be pushed through the distal syndesmosis, 1 cm proximal from the tibitiotalar joint. The physiotherapist and surgeon were blinded to the other one’s results. All patients were tested and treated between 1 and 4 weeks from the initial injury.
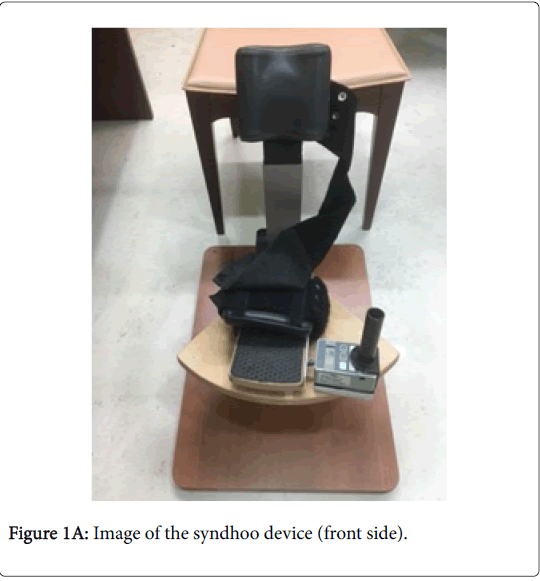
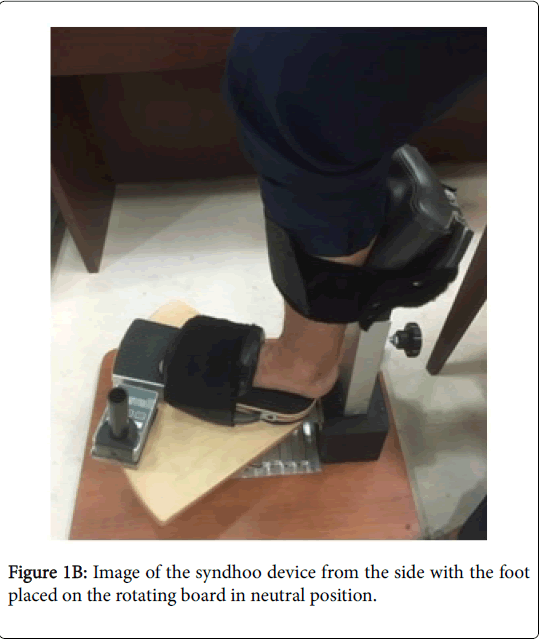
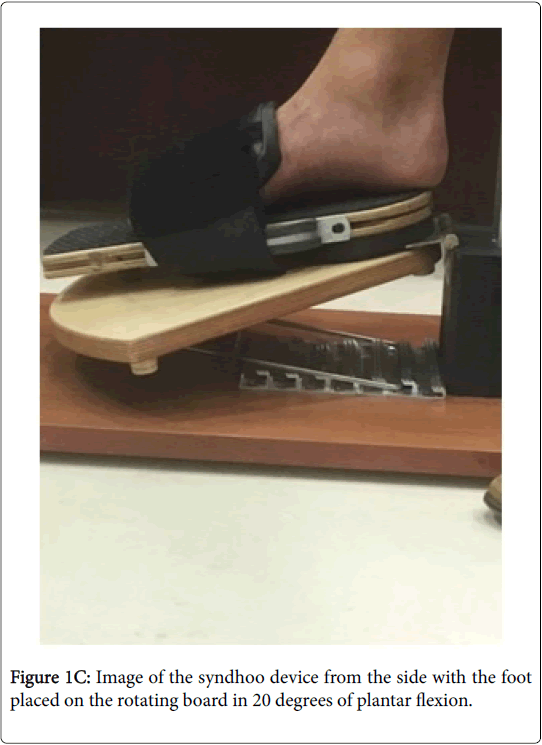
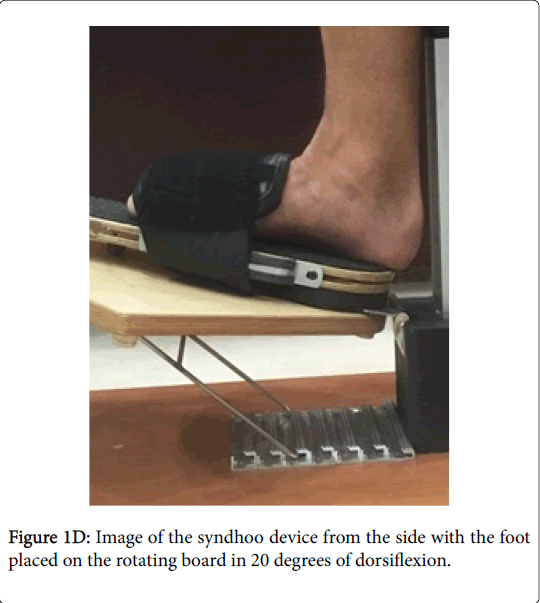
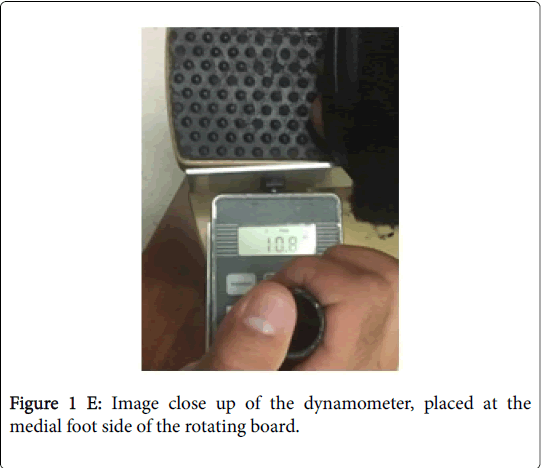
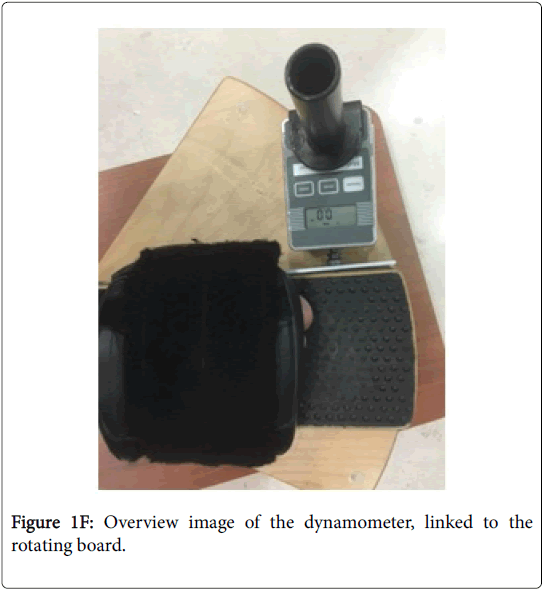
The principle of this syndhoo device is to dynamically evaluate the distal tibiofibular stability during external rotation of the ankle as an extension to the available clinical tests. Cadaveric testing has shown that the distal syndesmosis is unstable when a force of 87-100 N is applied. The foot is positioned and fixed on the syndhoo board that rotates over the heel (Figures 1A and 1B). The board can be put in neutral position, 20 degrees of plantar flexion and 20 degrees of dorsiflexion (Figures 1C and 1D). The knee is stabilized through a patellar strap and the patient is tested in sitting position (Figure 1B). With a dynamometer, the foot is passively externally rotated with the hinge positioned over the heel (Figures 1E and 1F). When the patient experiences clinical apprehension at a force <87 N, the syndhoo test is considered positive. If the apprehension occurs during a force 87-100N, the syndhoo test is considered equivocal. When no apprehension occurs or the apprehension occurs with a force >100N, the syndhoo test is considered negative.
Statistically, Cohen's kappa (κ) has been used to determine the inter-rater agreement between the arthroscopy method (as a reference) and the three syndhoo methods (dorsiflexion, neutral, plantar flexion). Based on the guidelines from Altman, and adapted from Landis & Koch, Cohen's kappa (κ) is interpreted as poor agreement if less than 0.20, fair agreement if between 0.20 to 0.40, moderate agreement if between 0.40 to 0.60, good agreement if between 0.60 to 0.80, and very good agreement if between 0.80 to 1.00).
Results
Syndhoo dorsiflexion: when pushing manually the dynamometer in external rotation (with the board in 20 degrees of dorsiflexion), the test is considered positive if the athlete feels apprehension at a force <87 Newton (N)
Syndhoo neutral: when pushing manually the dynamometer in external rotation (with the board in neutral position), the test is considered positive if the athlete feels apprehension at a force <87 Newton (N)
Syndhoo plantar flexion: when pushing manually the dynamometer in external rotation (with the board in 20 degrees of plantar flexion), the test is considered positive if the athlete feels apprehension at a force <87 Newton (N).
The descriptive results of the four types of diagnosis are presented in Table 1.
| Subject ID | Left Ankle |
Right Ankle |
Syndhoo Dorsiflexion | Syndhoo Neutral |
Syndhoo Plantar Flexion |
Arthroscopy |
|---|---|---|---|---|---|---|
| 1 | 2 | Positive | Positive | Positive | Positive | |
| 2 | 11.2 | Negative | Negative | Negative | Negative | |
| 3 | 13 | Negative | Negative | Negative | Negative | |
| 4 | 3.2 | Positive | Positive | Positive | Positive | |
| 5 | 6 | Positive | Negative | Negative | Positive | |
| 6 | 5.8 | Positive | Negative | Negative | Positive | |
| 7 | 1.6 | Positive | Positive | Positive | Positive | |
| 8 | 7 | Positive | Negative | Negative | Positive | |
| 9 | 5.4 | Positive | Positive | Negative | Positive | |
| 10 | 8,6 | Negative | Negative | Negative | Negative | |
| 11 | 8 | Negative | Negative | Negative | Negative | |
| 12 | 8,4 | Negative | Negative | Negative | Negative | |
| 13 | 3,6 | Positive | Positive | Positive | Positive | |
| 14 | 5,6 | Positive | Negative | Negative | Positive | |
| 15 | 6,2 | Positive | Negative | Negative | Positive |
Table 1: Diagnosis results.
There was very good agreement between arthroscopy and syndhoo dorsiflexion diagnosis (κ=1, p<0.001). However, no significant agreement was found between arthroscopy, and syndhoo neutral and syndhoo plantar flexion (p=0.053 and p=0.99, respectively).
Discussion
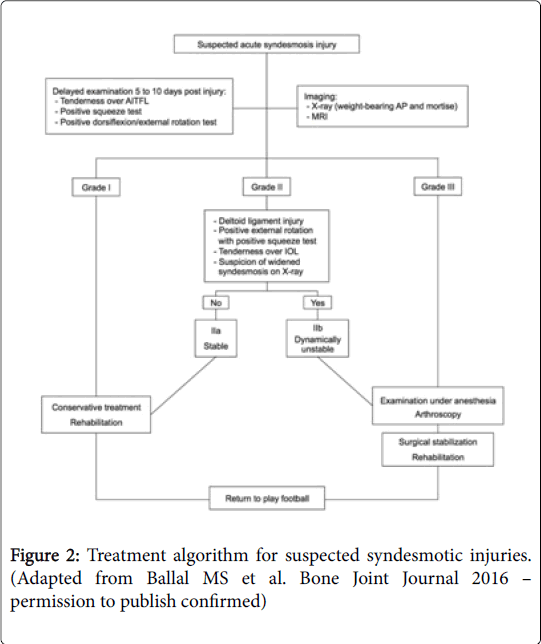
Syndesmotic injuries are divided into three grades. Grade I represents an AITFL sprain without instability. Grade II represents an AITFL tear and a partial IOL tear with mild instability. Grade III represents a complete rupture of all 3 syndesmotic ligaments with evident instability [7,15]. The severity of the syndesmotic instability guides the choice of treatment. Grade I injuries are treated nonsurgically [16] while the treatment of grade II injuries depends on the presented syndesmotic (in)stability testing [17]. Stable syndesmotic injuries (type I and IIa) should be treated conservatively, whereas unstable injuries (type IIb and III) warrant surgical fixation. A recent study found that a positive squeeze test and combined injury to the ATFL and deep deltoid ligament, are key factors in differentiating stable (type IIa) from unstable grade II injuries (type IIb). Nowadays, there is a consensus to perform an examination under anaesthesia and arthroscopic evaluation of the syndesmosis in case of a grade II injury with clinical and/or radiological suspicion of dynamic instability (type IIb) (Figure 2) [18,19]. In case of 2 mm or more dynamic distal tibiofibular diastasis, arthroscopic-assisted surgical fixation is warranted [16].
Grade III injuries often present with associated injuries and are inherently unstable. Surgical fixation by means of screws or suturebuttons can be used to reduce the mortise and stabilize the syndesmosis [20,21]. The Hook and/or Cotton test are regarded as reliable intra-operative stress tests to evaluate syndesmotic (in) stability [5]. Cadaveric studies have shown that the syndesmosis becomes unstable (opens more than 5 mm in tibiofibular clear space) when a force above 87-100 N is applied [5]. Arthroscopy is considered ‘the golden standard’ in the diagnostic assessment of syndesmotic (in)stability [22] and in case of doubt, fixation is advised because of the problems caused by chronic syndesmotic instability [5].
Athletes frequently present with an inability to bear weight, anterolateral pain between the distal tibia and fibula, medial ankle pain, ankle effusion and pain during gait push off [23]. However, anterolateral pain is not specific, as up to 40% of patients with an ATFL tear describe pain over the AITFL. Clinically it’s been suggested that the more proximal the patient’s pain, the more significant the injury [22].
Several clinical tests can be used in the evaluation of a syndesmotic injury. The external rotation test and the squeeze test are the most commonly described tests, but the Cotton test, the fibular-translation test and the cross-legged test can also be used [15]. The combination of tenderness on palpation over the ATFL, a positive fibular translation test, and positive Cotton test is considered highly clinically suspicious [17]. Although the squeeze test has been shown to be highly sensitive, there is no one “gold-standard” for the clinical diagnosis of syndesmotic instability [24]. In case of clinical suspicion, advanced imaging, such as MRI, is warranted.
Further studies on the correlation of this non-invasive test with clinical examination, imaging and arthroscopic findings are needed. Ongoing work at our institution is seeking to establish the agreement between the examination described here and MR quantification of syndesmotic injury which we hope will better depict the cut-point for a positive test.
We have found this clinical tool very helpful as part of the available options in the clinical diagnosis of syndesmotic instability.
Plain radiographs should always be obtained when there is concern for syndesmotic injury. The tibiofibular clear space, defined as the distance between the medial border of the fibula and the lateral border of the posterior tibia, is one of the most reliable indicators of syndesmotic disruption [25]. This distance is measured at 1 cm proximal to the tibial plafond and should not exceed 6 mm in both the AP and mortise views [25]. Stress radiographs are no longer recommended in the routine evaluation of syndesmotic instability since biomechanical studies have not shown significant advantage over plain radiographs [17,26]. Computed tomography (CT) scanning can be helpful in identifying minor diastasis and small avulsion fractures [27]. Although its value still needs further evaluation, promising new diagnostic types of bilateral standing CT scan stress view are useful [28]. Magnetic Resonance Imaging (MRI) can identify most ligamentous syndesmotic injuries and combined injuries [17]. MRI shows a sensitivity of 100% and a specificity of 93% for AITFL injuries (positive likelihood ratio of 14) and a sensitivity and specificity of 100% for PITFL injuries (infinite positive likelihood ratio) [29] and has high-degree of inter-observer reliability [30].
Ultrasonography is a fast and inexpensive tool to evaluate distal tibiofibular stability and does not expose the athlete to radiation. Further, it enables a dynamic assessment of the ligamentous injury, which is useful in cases of subtle instability. Patients with an acute AITFL rupture (confirmed on MRI) show a 100% sensitivity and specificity on dynamic ultrasound evaluation [1]. The disadvantages are that ultrasonography cannot detect associated injuries and is proven to be investigator dependent [17].
Conclusion
Traditionally, individuals with clinical and/or radiological suspicion of syndesmotic instability warrant an examination under anaesthesia and/or diagnostic arthroscopy to confirm and treat. However, the invasive process of this has inherent risks to the patient. The described non-invasive syndhoo device in this article can be a valuable tool in the evaluation of isolated syndesmotic ankle instability.
Further studies on the correlation of this non-invasive test with clinical examination, imaging and arthroscopic findings are needed. Ongoing work at our institution is seeking to establish the agreement between the examination described here and MR quantification of syndesmotic injury which we hope will better depict the cut-point for a positive test.
We have found this syndhoo device very helpful as part of the available options in the clinical diagnosis of syndesmotic instability.
References
- Mei Dan O, Kots E, Barchilon V, Massarwe S, Nyska M, et al. (2009) A dynamic ultrasound examination for the diagnosis of ankle syndesmotic injury in professional athletes: A preliminary study. Am J Sports Med 37: 1009-1016
- Kofotolis ND, Kellis E, Vlachopoulos SP (2007) Ankle sprain injuries and risk factors in amateur soccer players during a 2-year period. Am J Sports Med 35: 458-466.
- Roemer FW, Jomaah N, Niu J, Almusa E, Roger B, et al. (2014) Ligamentous Injuries and the risk of associated tissue damage in acute ankle sprains in athletes: A cross-sectional MRI study. Am J Sports Med 42: 1549-1557.
- Woods C, Hawkins R, Hulse M, Hodson A (2003) The football association medical research programme: An audit of injuries in professional football: An analysis of ankle sprains. Br J Sports Med 37: 233-238.
- Van den Bekerom MP (2011) Diagnosing syndesmotic instability in ankle fractures. World J Orthop 2: 51–56.
- Wright RW, Barlie J, Suprent DA, Matave MJ (2004) Ankle syndesmosis sprains in national hockey league players. Am J Sports Med 32: 1941–1945.
- Gerber JP, Williams GN, Scoville CR, Arciero RA, Taylor DC (1998) Persistent disability associated with ankle sprains: A prospective examination of an athletic population. Foot Ankle 19: 653–660.
- Waldén M, Hagglund M, Ekstrand J (2013) Time-trends and circumstances surrounding ankle injuries in men's professional football: An 11-year follow-up of the UEFA champions league injury study. Br J Sports Med 47: 748-753.
- Williams GN, Jones MH, Amendola A (2007) Syndesmotic ankle sprains in athletes. Am J Sports Med 35: 1197–1207.
- Xenos JS, Hopkinson WJ, Mulligan ME, Olson EJ, Popovic NA (1995) The tibiofibular syndesmosis: Evaluation of the ligamentous structures, methods of fixation, and radiographic assessment. J Bone Joint Surg Am 77: 847-856.
- Waterman BR, Belmont PJ, Cameron KL, Svoboda SJ, Alitz CJ, et al. (2011) Risk factors for syndesmotic and medial ankle sprain: Role of sex, sport, and level of competition. Am J Sports Med 39: 992-998.
- Williams GN, Allen EJ (2010) Rehabilitation of syndesmotic (high) ankle sprains. Sports Health 2: 460-470.
- Beumer A, Valstar ER, Garling EH, Niesing R, Ginai AZ, et al. (2006) Effects of ligament sectioning on the kinematics of the distal tibiofibular syndesmosis. Acta Orthop 77: 531-540.
- Zalavras C, Thordarson D (2007) Ankle syndesmosis injury. J Am Acad Orthop Surg 15: 330-339.
- Calder JD, Bamford R, Petrie A, McCollum GA (2016) Stable versus unstable grade ii high ankle sprains: A prospective study predicting the need for surgical stabilization and time to return to sports. Arthroscopy 32: 634-642.
- Mc Collum GA, van den Bekerom MP, Kerkhoffs GM, Calder JD, van Dijk CN (2013) Syndesmosis and deltoid ligament injuries in the athlete. Knee Surg Sports Traumatol Arthrosc 21: 1328-1337.
- van Dijk CN, Longo UG, Loppini M, Florio P, Maltese L, et al. (2016) Classification and diagnosis of acute isolated syndesmotic injuries: ESSKA-AFAS consensus and guidelines. Knee Surg Sports Traumatol Arthrosc 24: 1200-1216.
- Hunt KJ, Phisitkul P, Pirolo J, Amendola A (2015) High ankle sprains and syndesmotic injuries in athletes. J Am Acad Orthop Surg 23: 661-673.
- Kerkhoffs GMMJ, de Leeuw PAJ, Tennant JN, Amendola A (2014) Ankle ligament lesions. In: The ankle in football. Springer Verlag, Paris, pp: 81-96.
- Schepers T (2012) Acute distal tibiofibular syndesmosis injury: A systematic review of suture-button versus syndesmotic screw repair. Int Orthop 36: 1199–1206.
- van Dijk CN, Longo UG, Loppini M, Florio P, Maltese L, et al. (2016) Conservative and surgical management of acute isolated syndesmotic injuries: ESSKA-AFAS consensus and guidelines. Knee Surg Sports Traumatol Arthrosc 24: 1217-1227.
- Nussbaum ED, Hosea TM, Sieler SD, Incremona BR, Kessler DE (2001) Prospective evaluation of syndesmotic ankle sprains without diastasis. Am J Sports Med 29: 31-35.
- Hopkinson WJ, St Pierre P, Ryan JB, Wheeler JH (1990) Syndesmosis sprains of the ankle. Foot Ankle 10: 325–330.
- Sman AD, Hiller CE, Refshauge KM (2013) Diagnostic accuracy of clinical tests for diagnosis of ankle syndesmosis injury: A systematic review. Br J Sports Med 47: 620-628.
- Harper MC (1993) An anatomic and radiographic investigation of the tibiofibular clear space.  Foot Ankle 14: 455-458.
- Beumer A, Valstar ER, Garling EH, van Leeuwen WJ, Sikma W, et al. (2003) External rotation stress imaging in syndesmotic injuries of the ankle: Comparison of lateral radiography and radiostereometry in a cadaveric model. Acta Orthop Scand 74: 201-205.
- Ebraheim NA, Lu J, Yang H, Mekhail AO, Yeasting RA (1997) Radiographic and CT evaluation of tibiofibular syndesmotic diastasis: A cadaver study. Foot Ankle Int 18: 693-698.
- Vopat ML, Vopat BG, Lubberts B, DiGiovanni CW (2017) Current trends in the diagnosis and management of syndesmotic injury. Curr Rev Musculoskelet Med 10: 94-103.
- Takao M, Ochi M, Oae K, Naito K, Uchio Y (2003) Diagnosis of a tear of the distal tibiofibular syndesmosis. The role of arthroscopy of the ankle. J Bone Joint Surg Br 85: 324-329.
- Oae K, Takao M, Naito K, Uchio Y, Kono T, et al. (2003) Injury of the tibiofibular syndesmosis: Value of MR imaging for diagnosis. Radiology 227: 155-161.
Citation: D’Hooghe P, Bouhdida S, Whiteley R, Rosenbaum A, Khelaifi K et al. (2018) Stable versus Unstable Grade 2 High Ankle Sprains in Athletes: A Noninvasive Tool to Predict the Need for Surgical Fixation. Clin Res Foot Ankle 6:252. DOI: 10.4172/2329-910X.1000252
Copyright: © 2017 D’Hooghe P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 8290
- [From(publication date): 0-2018 - Apr 19, 2025]
- Breakdown by view type
- HTML page views: 7233
- PDF downloads: 1057