Spontaneous Pneumomediastinum: Prognostic Marker in COVID-19 Pneumonia Patients
Received: 18-Dec-2023 / Manuscript No. JIDT-23-120444 / Editor assigned: 21-Dec-2023 / PreQC No. JIDT-23-120444 (PQ) / Reviewed: 05-Dec-2023 / QC No. JIDT-23-120444 / Revised: 12-Dec-2023 / Manuscript No. JIDT-23-120444 (R) / Published Date: 19-Dec-2023 DOI: 10.4172/2332-0877.1000576
Abstract
Coronavirus Disease 2019 (COVID-19) began in late 2019 as a highly transmissible, infectious viral illness caused by the pathogen SARS-CoV-2. The related viral disease Severe Acute Respiratory Syndrome (SARS) has been around since early 2003 and presents as mild to moderate Upper Respiratory Illness (URI) progressing to Lower Respiratory Illness (LRI). Three years into the COVID-19 pandemic, uncommon presentations of disease are becoming more prevalent. Pneumomediastinum, a rare condition in which air is trapped in the mediastinum, was clinically examined during a case of COVID-19 in a 56-year-old patient.
Keywords: Pneumomediastinum; COVID-19; Lower respiratory illness; Upper respiratory illness
Introduction
Pneumomediastinum is the presence of air or other gas in the mediastinum which commonly arises from trauma secondary to mechanical ventilation or spontaneously in preexisting lung disease. Here, we present a case of COVID-19 pneumonia in which the patient developed Pneumomediastinum without any trauma or other risk factors. This article was previously presented as a meeting abstract at the 2020 AANS Annual Scientific Meeting on April 27, 2020.
Case Presentation
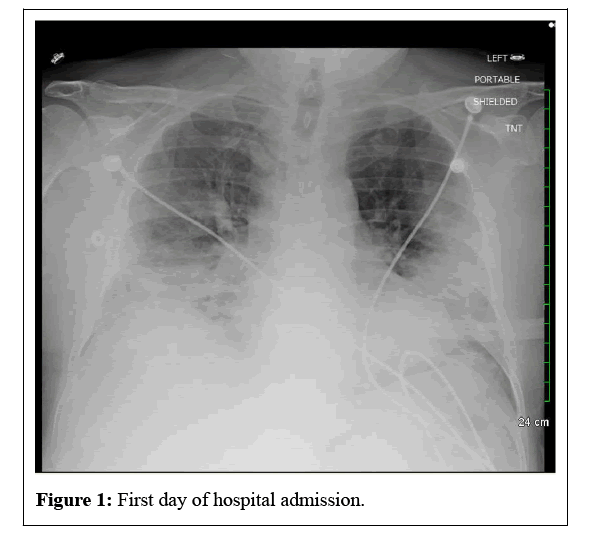
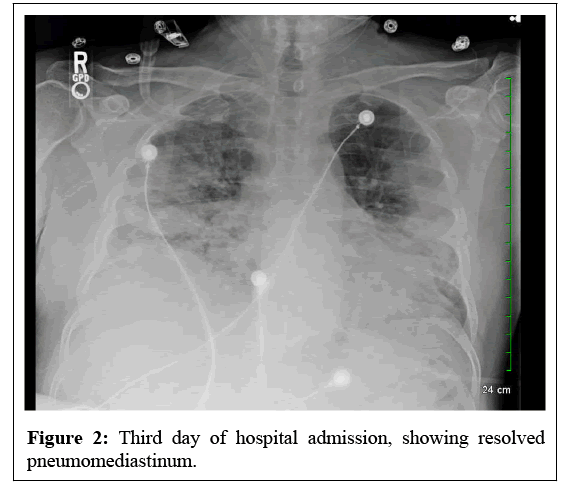
A 56-year-old COVID-unvaccinated male with a history of essential hypertension presented to the ED with shortness of breath and worsening cough for one week. He was living with his father, who was admitted to the ICU and receiving treatment for COVID pneumonia. The patient appeared to be in respiratory distress. His initial vital signs were a temperature of 99.6F, respiratory rate of 26 breaths per minute, blood pressure of 125/71 mm Hg, heart rate of 109 beats per minute with a regular rhythm, and oxygen saturation of 50% while he was breathing ambient air. Pulmonary examination revealed the use of respiratory accessory muscle and widespread bilateral coarse rhonchi on auscultation. The rest of the physical examination was within normal limits. RT-PCR COVID-19 test was positive. The blood gas analysis reported respiratory alkalosis. Inflammatory markers were elevated: Erythrocyte sedimentation rate (35.2 mg/L), C-Reactive Protein (17.70 mg/dL), Ferritin (1108.1 ng/mL), Lactate Dehydrogenase (813 U/L), Lactate (2.4 mg/dL), D-Dimer (35.20 mg/L) and Troponin High Sensitivity-236.6 ng/L. His total WBC count were WNL (10.7 × 10*3/uL). His electrolytes and kidney function were normal. Chest X-ray showed pneumomediastinum with dense basilar predominant consolidation. CT Angio Chest with contrast revealed pneumomediastinum, likely from the left central airway source, and bilateral dense ground glass consolidation. An echocardiogram showed an ejection fraction of 60-65% with no valvular abnormalities. He was placed on Vapotherm (Oxygen 40L/ min) with 100% FiO2. He was given Dexamethasone 6 mg for ten days, Remdesivir, Barcitinib, and a 7-day course of Azithromycin and Ceftriaxone for community-acquired pneumonia. He was advised to practice prone positioning for 12 hours or more per day. Pulmonology, infectious disease, and cardiology were consulted. Gradually, his oxygen requirement was weaned down. After day three, serial chest xrays showed resolved pneumomediastinum. After ten days, the patient was discharged on home oxygen in a clinically stable condition (Figures 1 and 2).
Discussion
Pneumomediastinum in viral pneumonia is rare. The current hypothesis is that COVID-19 pneumonia causes diffuse alveolar wall damage, which may result in air leakage into the mediastinum via dissection along the bronchovascular sheaths [1,2]. The development of pneumomediastinum can be an ominous sign in COVID-19 pneumonia after iatrogenic causes have been ruled out. Fortunately, our patient did not worsen and was weaned off high-flow oxygenation requirements.
Interestingly, similar cases have been reported in the literature where critical patients with COVID-19 positive pneumomediastinum have had favorable outcomes. Kong, et al., report a case of a 62-year-old male who did not receive any prior trauma or mechanical ventilation, yet developed a spontaneous pneumomediastinum on day 14 of his symptoms. His treatment also improved after supportive therapy and he did not have any other complications [3]. Kolani, et al., report having a 23- year-old patient that presented asymptomatically with favorable oxygen saturation at 98% after known COVID-19 contact. Non-contrast CT was performed after COVID-19 PCR and showed ground glass opacities consistent with early onset viral pneumonia. It also showed a small amount of air in the mediastinum, however without fluid retention, and repeat CT 7 days later showed complete resolution [4,5].
Although in the aforementioned cases complete resolution was achieved, the literature also describes rare cases in which pneumomediastinum in COVID-19 patients has resulted in further clinical decompensation. Wang et. al reported the case of a 36-year-old woman who presented with 12 days of URI symptoms. Chest CT demonstrated multiple areas of consolidation and ground-glass opacities with lung severity score of 19 out of 20. No source of mediastinal air was detected and it was deemed spontaneous secondary to covid pneumonia. She was given antiviral and antiinflammatory drugs along with supportive oxygenation but still passed away due to acute respiratory distress syndrome [6]. A case series from Wali et. al discusses 5 patients (Age/Sex: 60M, 51M, 38M, 60M, 70M) with COVID-19 pneumonia who developed pneumomediastinum, all of which occurred after intubation. None of these patients had any known prior lung disease. These patients were all in the ICU and they reported mean airway pressures of 13-15 cm H2O and peak airway pressures of 22-30 cm H2O.Pneumomediastinum was confirmed by chest x-ray or CT and bilateral intra-pleural chest drains were placed on a closed circuit. Of these 5 patients, 2 passed away after multi-organ failure and the other 3 were decannulated and clinically stable at the time of publication [5]. Another case series published by Damous, et al., reports 4 cases (74F, 48M, 70M, 50M), all with no prior lung injury or disease, who were all ventilated without any complications. Of these 4 patients, 3 had passed away and the remaining patient (48M) went home on home rehabilitation with no need for oxygen therapy. They report that all 4 of these patients had greater than 10 days of disease, more than 50% pulmonary involvement confirmed by chest CT, and PEEP between 8-10 cm H2O [1].
The management of pneumomediastinum in COVID-19 patients currently lacks evidence-based clinical guidelines due to the infrequency of its presentation. A review article by Patel, et al., outlines a proposed management algorithm for pneumomediastinum, subcutaneous emphysema, and pneumothorax in COVID-19 patients. Their study indicated that conservative management of pneumomediastinum, as conducted by our team, is the best course of action unless the patient presents with multiple pulmonary risk factors [7].
Conclusion
Few isolated reports of pneumomediastinum in a COVID-19 patient have been associated with life-threatening complications. These cases typically present with no history of trauma, mechanical ventilation, or any other iatrogenic cause to explain the pneumomediastinum. It should be used as a prognostic marker, and close monitoring of these patients is advisable.
References
- Damous SHB, dos Santos Junior JP, Pezzano ÁVA, Majid Chams MA, Haritov N, et al. (2021) Pneumomediastinum complicating COVID-19: a case series. Eur J Med Res 26:114.
[Crossref] [Google Scholar] [PubMed]
- Caceres M, Braud RL, Maekawa R, Weimen DS, Garret EH (2009) Secondary pneumomediastinum: a retrospective comparative analysis. Lung 187:341-346.
[Crossref] [Google Scholar] [PubMed]
- Kong N, Gao C, Xu MS, Xie YL, Zhou CY (2020) Spontaneous pneumomediastinum in an elderly COVID-19 patient: a case report. World J Clin Cases 8:3573-3577.
[Crossref] [Google Scholar] [PubMed]
- Kolani S, Houari N, Haloua M, Alaoui Lamrani Y, Boubbou M, et al. (2020) Spontaneous pneumomediastinum occurring in the SARS-COV-2 infection. IDCases 21:e00806.
[Crossref] [Google Scholar] [PubMed]
- Wali A, Rizzo V, Bille A, Routledge T, Chambers AJ (2020) Pneumomediastinum following intubation in COVID-19 patients: a case series. Anaesthesia 75:1076-1081.
[Crossref] [Google Scholar] [PubMed]
- Wang J, Su X, Zhang T, Zheng C (2020) Spontaneous pneumomediastinum: a probable unusual complication of Coronavirus Disease 2019 (COVID-19) pneumonia. Korean J Radiol 21:627-628.
[Crossref] [Google Scholar] [PubMed]
- Patel N, Nicolae R, Geropoulos G, Mandal P, Christou CD, et al. (2022) Pneumomediastinum in the COVID-19 era: to drain or not to drain? Monaldi Arch Chest 93:2.
[Crossref] [Google Scholar] [PubMed]
Citation: Mehdizadeh C, Amatya P, Bhakta P, Patel F (2023) Spontaneous Pneumomediastinum: Prognostic Marker in COVID-19 Pneumonia Patients. J Infect Dis Ther 11:577. DOI: 10.4172/2332-0877.1000576
Copyright: © 2023 Mehdizadeh C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1608
- [From(publication date): 0-0 - Oct 31, 2025]
- Breakdown by view type
- HTML page views: 1318
- PDF downloads: 290