Spontaneous Dissection of the Vertebral Artery
Received: 06-May-2021 / Accepted Date: 11-May-2021 / Published Date: 18-May-2021 DOI: 10.4172/2167-7964.1000329
Abstract
The dissection of the cervical arteries is a common cause of ischemic strokes in young adults,the dissection of vertebral artery (VAD) is less common than the dissection of carotid artery, MRI is reference examination allows direct visualization of the parietal hematoma, The Most of VAD heal spontaneously especially for extra cranial VAD, however intracranial VAD is generally of poor prognosis.
Keywords: Dissection of the vertebral arteries, MRI, Intramural haematoma
Clinical Observation
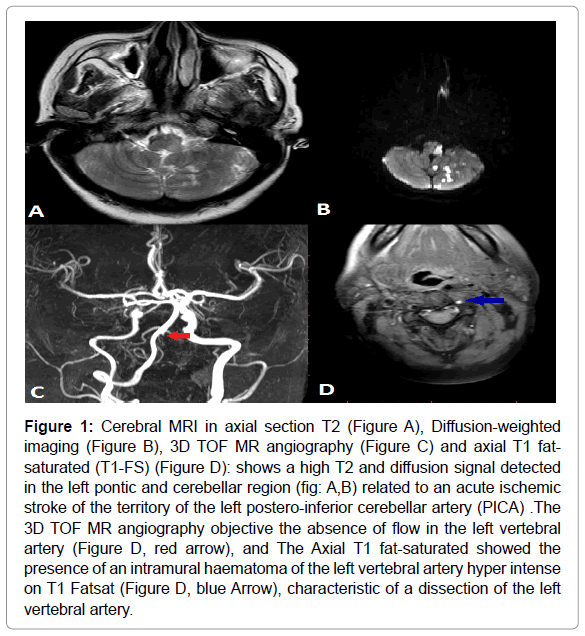
Our case is about a 40-year-old woman who consults in an emergency for a right acute Onset hemiplegia with no obvious history of cervical trauma.the interrogator finds the notion of headaches in the right occipital region since about ten days A cerebral CT was performed who shows an ischemic stroke of the left postero-inferior cerebellar artery (PICA territory), a cerebral MRI was carried out which shows the presence of an intramural haematoma of the left vertebral artery hyper intense on T1 Fat sat, and the 3D TOF MR angiography objective the absence of flow in the left vertebral artery related to the dissection of the vertebral artery.
Discussion
The dissection of the vertebral artery (VAD) indicates a tear of the wall of the vertebral artery with penetration and collection of blood in its layers and constitution of an intramural hematoma responsible for an occlusion or an aneurysmal dilation.
The dissection of the cervical arteries (CAD) is a rare pathology with an incidence of 2.6-2.9 per 100,000 per year for the carotid artery and 1.3-1.5 per 100,000 per year for the vertebral artery. There is no overall sex-based predilection. CAD considered a rare cause of stroke with a percentage of 2%, but it is a common cause of ischemic strokes in young adults with a percentage of 10 to 25% [1].
Its pathogenesis remains poorly understood, some authorities consider that the lesion of the connective tissue of the media is the main triggering element of the dissection artery, as well as the genetic component may be involved in the weakness of the vessel wall, because of The high prevalence of CAD in patients with hereditary connective tissue disorders, the Ehlers–Danlos syndrome pseudoxanthoma elasticum, Marfan’s syndrome, orthogenesis imperfect and fibro muscular dysplasia [1,2].
There is a strong relationship between the pathogenesis of the dissection and the clinical course, which is why we can classify intracranial dissection into four types:
Type 1 involves classic dissecting aneurysms, without intimal thickening, and patients of this type present a worrying clinical course with subarachnoid haemorrhage
Type 2 aneurysms often present as segmental ecstasies with an extended and / or fragmented internal elastic lamina (IEL) with intimal thickening, patients of this type have a placid clinical course.
Type 3 aneurysms characterized by multiple dissections of thickened intima and an organized thrombus in the lumen. Patients of this type are often symptomatic. On the other hand type 4 aneurysms are secular aneurysms that appear in areas with a little disturbed IEL without intimal thickening [3,4].
Spontaneous cervical artery dissection (sVAD) often occurs in healthy young people without obvious trauma. Sometimes presence of a mild mechanical stress such as hyper flexion and rotation during YOGA and chiropractic manipulation, a cough or sudden movement of the head during sports activities [2].
The dissection origin is often in C1-2 segment, It can begin in neck and extending in intracranial region of the vessel. The dissection of the vertebral artery affects in the ma-jority of cases more than one segments (in 38%). The there are two types of sVAD, the ischemic type by reduction of the arterial light or by thromboembolism and the haemorrhagic type in the form of a subarachnoid haemorrhage by the rupture of an arterial dissecting aneurysm.
Clinical manifestations in Extra cranial VAD mainly include a severe neck pain predominantly in the occipitocervical region occurring after a variable interval (the delay between onset of symptoms and stroke onset ranged between 1 to 14 days), as well as dizziness, double vision, ataxia and dysarthria even neurological symptoms deficient. Wallenberg’s syndrome and cerebellar infarctions are also frequent situations. On the other hand, the intracranial VAD are associated with subarachnoid haemorrhage in more than 50% with a worse prognosis [2,3].
Doppler ultrasound shows a parietal hematoma with hemodynamic repercussions, abnormal flow in 95% of patients, the Doppler ultrasound has the advantages of being quick, non-invasive and often easily accessible, but in some situations the dissection may not be well seen with ultrasound. The CT scan may show the area of cerebral ischemia or subarachnoid haemorrhage. It can also identify an occlusion of the vertebral artery or the indirect signs (arterial stenosis, wall thickening) and the CT angiography appears to have very high sensitivity for dissection of the vertebral artery [3].
MRI is a benchmark examination in the diagnosis of VAD with very high sensitivity and specificity allowing direct visualization of the parietal hematoma with a semilunar morphology or a unilateral crescent along the affected portion, visualized in hyper T1 signal with saturation of the fat signal which (due to the presence of methemoglobin) the most affected portion is the C1-2 segment where the artery is more movable, RM angiography shows stenosis or complete occlusion of the lumen [3,4].
Catheter angiography has been the gold standard for diagnosing arterial dissections, but it is considered an invasive method that tends to be replaced by MR, the classic sign found on angiography is the “chord sign” at the affected segment. the other signs are an intimal flap or a double lumen. The artery may show a sudden tapering due to occlusion of the lumen, aneurysm dilations are also found in some cases [5,6].
The Most of VAD heal spontaneously especially for extra cranial VAD, however, intracranial VAD is generally of poor prognosis.
The therapeutic management is the same as that of the stroke in acute phase include intravenous heparin, calciparin, heparin of low molecular weight and the antiplatelet antithrombotics.the final vascular treatment (angioplasty with placement and intra-arterial thrombolysis) must be discussed case by case, reperfusion is the best sign of successful procedure, on the other hand, non-recanalization leads to death. Recurrence of dissection is rare [3,4].
Conclusion
The dissection of the vertebral artery results from a tear of the wall of the vertebral artery with constitution of an intramural hematoma, MRI is reference examination for the diagnostic, with very high sensitivity and specificity allowing direct visualization of the parietal hematoma. The therapeutic management is the same as that of the stroke in acute phase. The vascular discussed case by case. The Most of VAD heal spontaneously especially for extra cranial VAD, however intracranial VAD is generally of poor prognosis Figure 1.
Figure 1: Cerebral MRI in axial section T2 (Figure A), Diffusion-weighted imaging (Figure B), 3D TOF MR angiography (Figure C) and axial T1 fat-saturated (T1-FS) (Figure D): shows a high T2 and diffusion signal detected in the left pontic and cerebellar region (fig: A,B) related to an acute ischemic stroke of the territory of the left postero-inferior cerebellar artery (PICA) .The 3D TOF MR angiography objective the absence of flow in the left vertebral artery (Figure D, red arrow), and The Axial T1 fat-saturated showed the presence of an intramural haematoma of the left vertebral artery hyper intense on T1 Fatsat (Figure D, blue Arrow), characteristic of a dissection of the left vertebral artery.
References
- Hassen WB, Machet A, Edjlali-Goujon M, Legrand L,nLadoux A, et al.  (2014) Imagerie de landissection des artères cervico-encéphaliques. Jde Radiologie Diagnostique et Intervetionnelle 95n(12): 1136-1147.
- Chen JL, Smith R, Keller A, Kucharczyk W (1989) Spontaneous dissection of the vertebral arterynMR findings. J Computer Assisted Tomography 13(2): 326-329.
- Sano H, Kato Y, Okuma I, Yamaguchi S, Ninomiya T, etnal (1997) Classification et traitement denl'anévrisme à dissection vertébrale 48 (6): 598-605.
- Abdullah Bin Saeed, Shuaib A, Emery D, Sulaiti Gn(2000) Dissection de l'artèrenvertébrale: symptômes précurseurs, caractéristiques cliniques et pronostic chez 26npatients. Revue canadienne des sciences neurologiques 27 (4): 292-296.
- Park KW, Park JS, Hwang SC, Im SB, Shin, et al. (2008)n Dissection de l'artère vertébrale: histoire naturelle, caractéristiques cliniques etnconsidérations thérapeutiques. Journal de la Société coréenne de neurochirurgien44 (3): 109.
- De Bray JM, Alecu C (2006) Le diagnostic de dissection des artèresncervicales en 87(4):343-344
Citation: Maniani AID, Sahli H, Kabir D, Fikri M, Jiddane M, et al. (2021) Spontaneous Dissection of the Vertebral Artery. OMICS J Radiol 10: 329. DOI: 10.4172/2167-7964.1000329
Copyright: © 2021 Maniani AID, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 1973
- [From(publication date): 0-2021 - Mar 29, 2025]
- Breakdown by view type
- HTML page views: 1219
- PDF downloads: 754