Case Report Open Access
Spontaneous Conventional Osteosarcoma Transformation of a Chondroblastoma First Ever Case Report and Literature Review
Prashant N1*, Amber H2, Azuhairy A1, Serene L3, Chin Heng F4, Vivek Ajit S2 and Zulkiflee O11Department of Orthopaedics, Pulau Pinang Hospital, Georgetown, Penang, Malaysia
2Department of Orthopaedic Surgery, Universiti Malaya Medical Center, Jalan Universiti, Kuala Lumpur, Malaysia
3Department of Pathology, Pulau Pinang Hospital, Jalan Residensi, Georgetown, Penang, Malaysia
4Department of Oncology, Pulau Pinang Hospital, Jalan Residensi, Georgetown, Penang, Malaysia
- Corresponding Author:
- Prashant N
Department of Orthopaedics, Pulau Pinang Hospital
Kementerian Kesihatan Malaysia
Georgetown, Penang, Malaysia
Tel: +604-2225333
E-mail: rhikhesa@hotmail.com
Received Date: July 23, 2017; Accepted Date: July 31, 2017; Published Date: August 05, 2017
Citation: Prashant N, Amber H, Azuhairy A, Serene L, Chin Heng F, et al. (2017) Spontaneous Conventional Osteosarcoma Transformation of a Chondroblastoma First Ever Case Report and Literature Review. J Orthop Oncol 3:120. doi: 10.4172/2472-016X.1000120
Copyright: © 2017 Prashant N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Orthopedic Oncology
Introduction
Chondroblastomas are primary benign cartilagenous tumour that accounts for approximately 1% of all benign bone tumours [1]. They are commonly seen at the epiphysis region in an immature long bone [2]. Despite being benign, they do metastases to the lung in 2% of cases. Chondroblastomas are primarily treated by curretage. Precaution is taken to minimize damage to the adjacent physeal plate. Occasionally the remaining cavity is filled with either bone graft or cement to achieve stability and prevent joint collapse. In recent years, radio frequency ablation is carried out and it gives promising results [3]. As these treatments are considered intralesional, they carry a risk of local recurrence of 8-40% [4,5]. In the past, irradiation was not uncommon in treating chondroblastoma and this accounted for some post irradiation sarcoma. Malignancy associated with chondroblastoma without irradiation was unheard of until 1970 when M.V. Sirsat reported a case of chondroblastoma eventually presenting as a high grade undifferentiated sarcoma [6]. We report a case of benign chondroblastoma which subsequently manifested as high grade conventional osteosarcoma. As far as we are concerned, this is a first of such case ever reported in the literature. We will also be looking at some frequently used terms when dealing with aggressive chondroblastoma and clarify some common misconceptions.
Case Summary
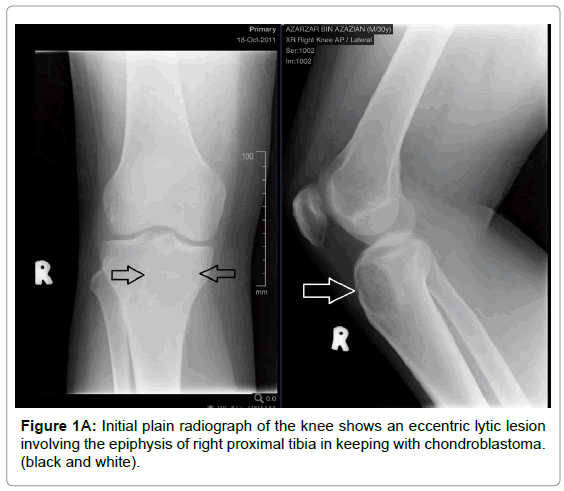
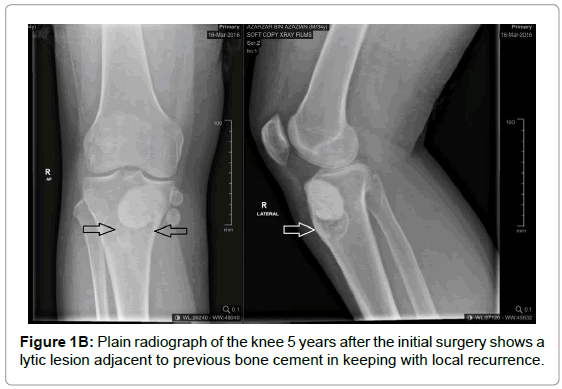
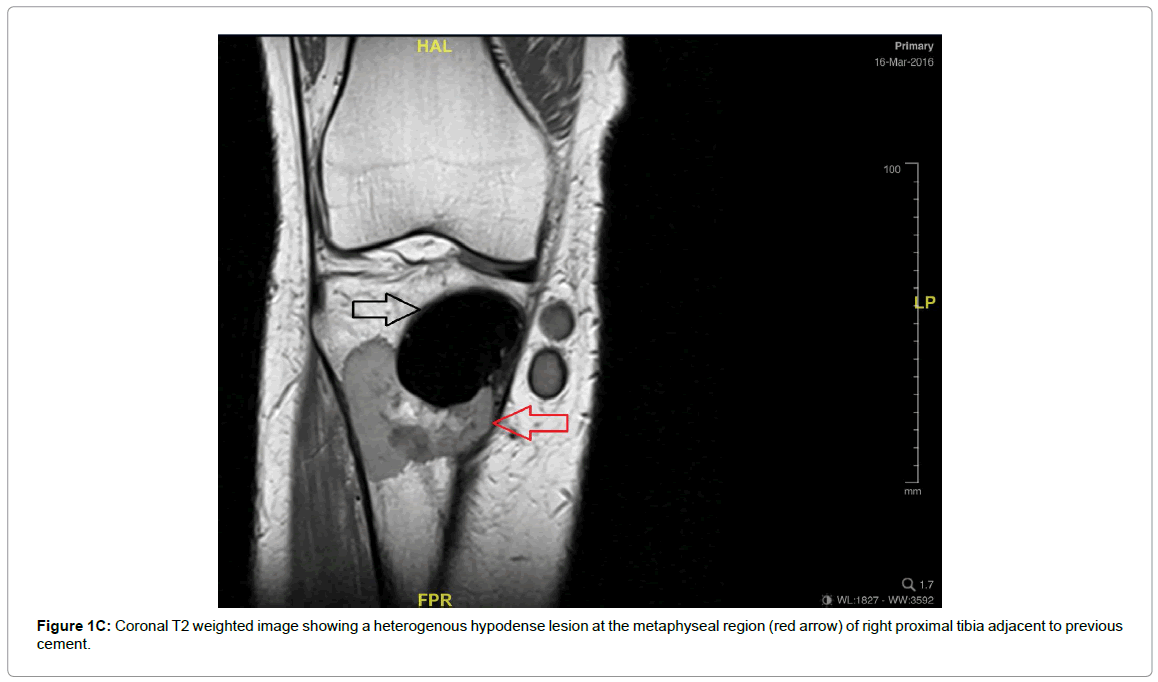
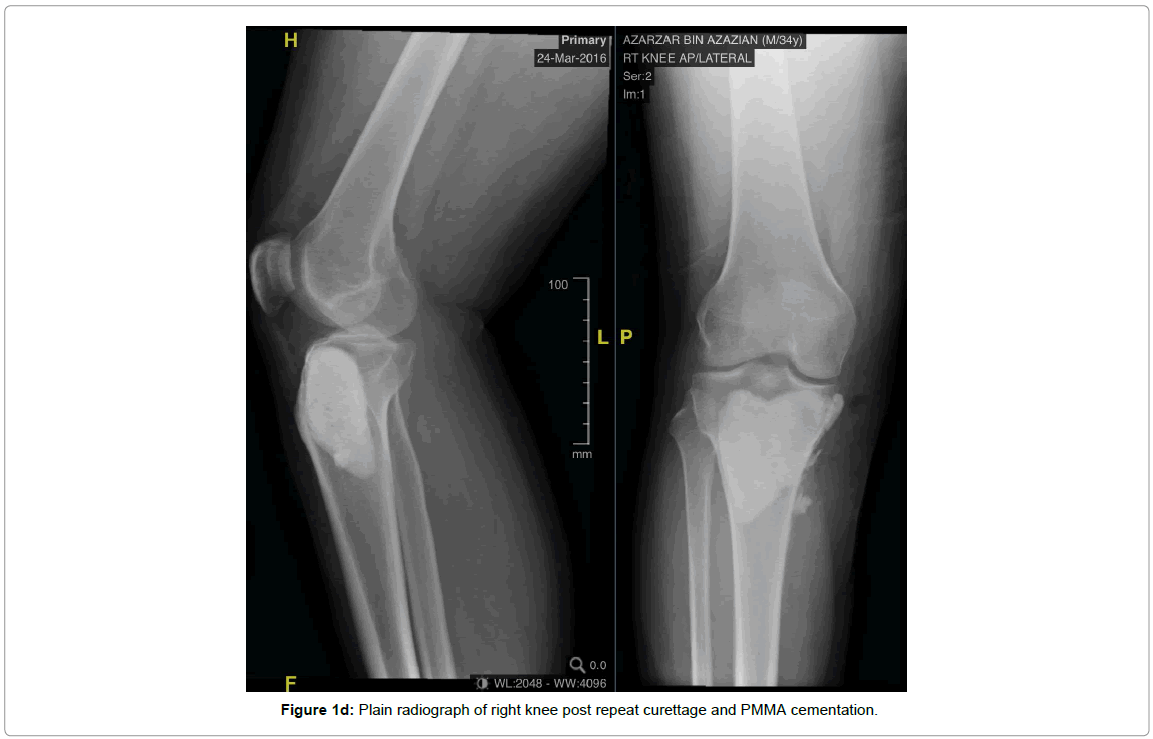
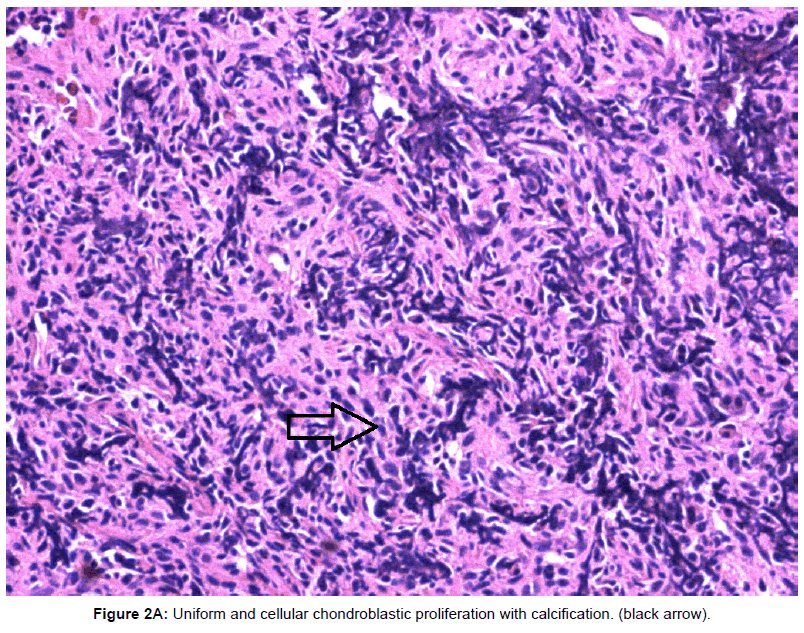
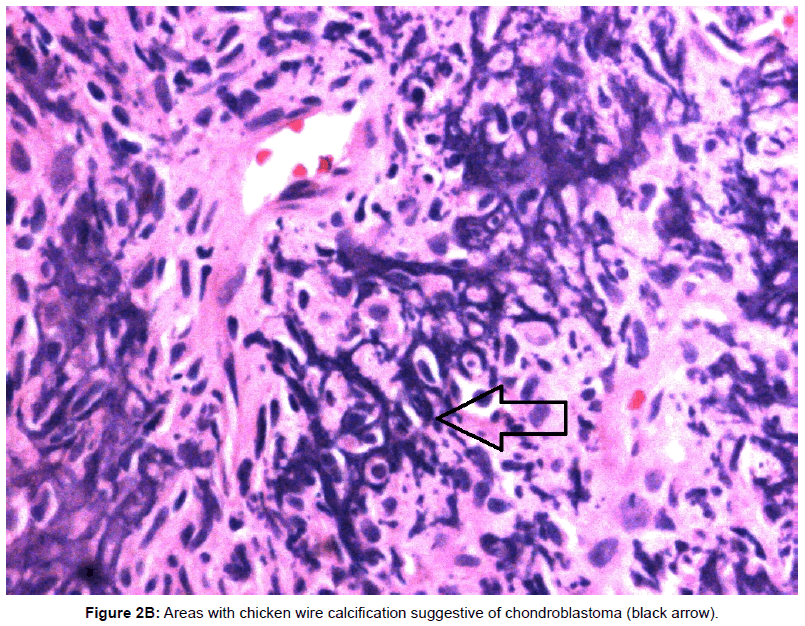
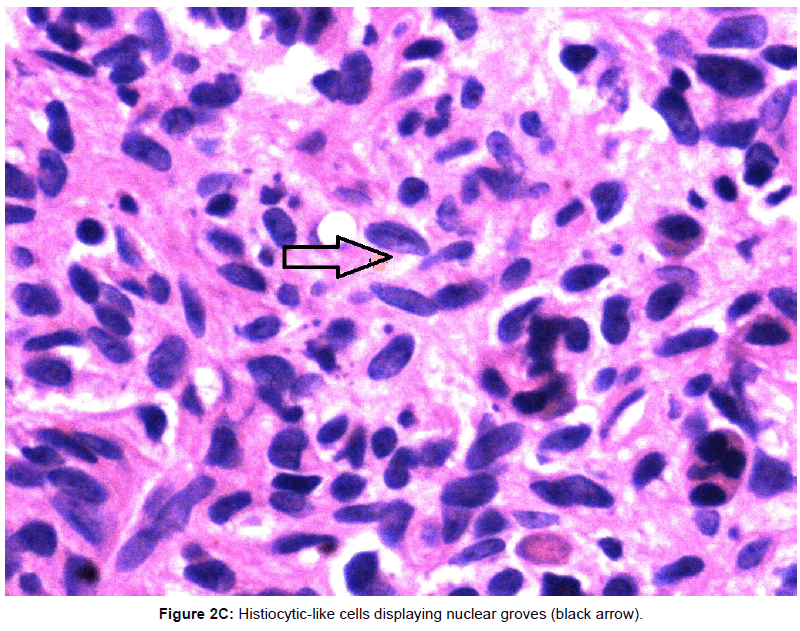
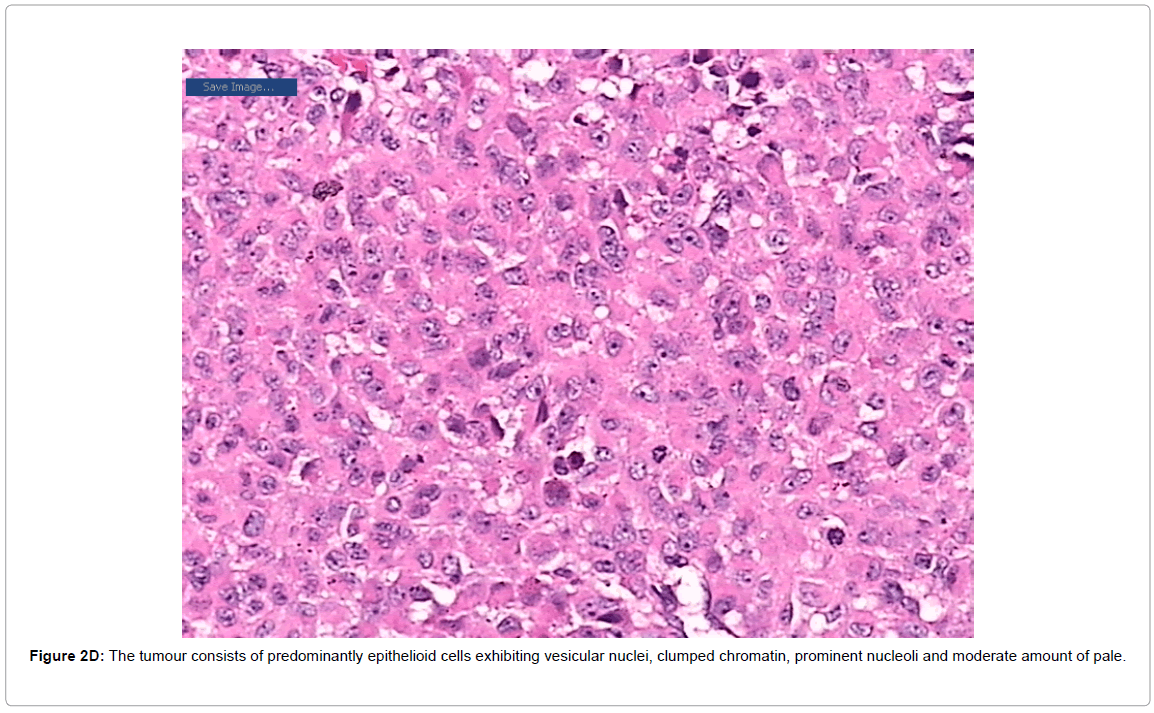
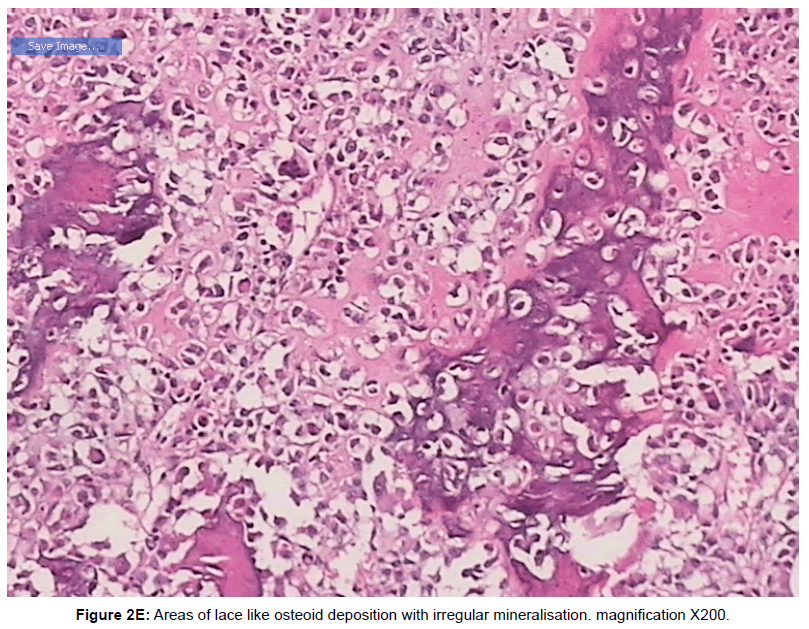
In 2011, a 29 years old gentleman presented with a painful swelling over his right knee for 4 months duration. Plain radiograph showed an eccentric lytic lesion over the epiphysis of right proximal tibia (Figure 1A). Biopsy confirmed as chondroblastoma (Figure 2A-2C). Extended curretage and bone cementation using PMMA cement was performed. He was well for the next 4 years. In 2015, he presented for the second time with pain and swelling over right knee. Plain radiograph revealed a lytic lesion just adjacent to previous PMMA cement in keeping with local recurrence (Figure 1B). MRI showed recurrent lesion adjacent to the bone cement (Figure 1C). Repeat curretage with bone cementation was done (Figure 1D) for the lesion. Within a few weeks his knee pain and swelling worsened. He was in pain especially while weight bearing and the pain did disturb his sleep. His knee range of motion was restricted from 15 to 110 degrees of flexion. The histopathology report from the curretage unfortunately came back as Conventional Osteosarcoma. Further systemic staging showed multiple small lung nodules in keeping with distance metastasis. The bone scan however did not pick up any skeletal metastasis. He further underwent proximal tibia wide resection with endoprosthesis reconstruction and medial gastrocnemeus flap followed by adjuvant chemotherapy. Post-operative, his wound healing was uncomplicated and he started regaining good function of his right lower limb with physiotherapy. The resected specimen was send for histopathology and margins and revealed a high grade conventional osteosarcoma (Figure 2D and 2E) with close margins. The histology was reviewed and confirmed by a bone and soft tissue pathologist as the local pathologist was well aware of the rarity of this case. Patient was started on adjuvant chemotherapy. Sadly he succumb to lung metastasis after his 3rd cycle of chemotherapy.
Figure 1A: HPLC chromatogram of the nine reference compounds in 50% aqueous methanol, measured at 370nm. Retention times for rutin, sutherlandin A, sutherlandin B, kaempferol-3-O-rutinoside, sutherlandin C, sutherlandin D, quercitrin, quercetin and kaempferol were 11.9, 12.7, 13.8, 15.3, 16.2, 17.0, 18.0, 26.2 and 28.1 minutes, respectively.
Figure 1B: HPLC chromatogram of the nine reference compounds in 50% aqueous methanol, measured at 370nm. Retention times for rutin, sutherlandin A, sutherlandin B, kaempferol-3-O-rutinoside, sutherlandin C, sutherlandin D, quercitrin, quercetin and kaempferol were 11.9, 12.7, 13.8, 15.3, 16.2, 17.0, 18.0, 26.2 and 28.1 minutes, respectively.
Figure 1C: HPLC chromatogram of the nine reference compounds in 50% aqueous methanol, measured at 370nm. Retention times for rutin, sutherlandin A, sutherlandin B, kaempferol-3-O-rutinoside, sutherlandin C, sutherlandin D, quercitrin, quercetin and kaempferol were 11.9, 12.7, 13.8, 15.3, 16.2, 17.0, 18.0, 26.2 and 28.1 minutes, respectively.
Figure 1D: HPLC chromatogram of the nine reference compounds in 50% aqueous methanol, measured at 370nm. Retention times for rutin, sutherlandin A, sutherlandin B, kaempferol-3-O-rutinoside, sutherlandin C, sutherlandin D, quercitrin, quercetin and kaempferol were 11.9, 12.7, 13.8, 15.3, 16.2, 17.0, 18.0, 26.2 and 28.1 minutes, respectively.
Figure 2A: HPLC chromatogram of the nine reference compounds in 50% aqueous methanol, measured at 370nm. Retention times for rutin, sutherlandin A, sutherlandin B, kaempferol-3-O-rutinoside, sutherlandin C, sutherlandin D, quercitrin, quercetin and kaempferol were 11.9, 12.7, 13.8, 15.3, 16.2, 17.0, 18.0, 26.2 and 28.1 minutes, respectively.
Figure 2B: HPLC chromatogram of the nine reference compounds in 50% aqueous methanol, measured at 370nm. Retention times for rutin, sutherlandin A, sutherlandin B, kaempferol-3-O-rutinoside, sutherlandin C, sutherlandin D, quercitrin, quercetin and kaempferol were 11.9, 12.7, 13.8, 15.3, 16.2, 17.0, 18.0, 26.2 and 28.1 minutes, respectively.
Figure 2C: HPLC chromatogram of the nine reference compounds in 50% aqueous methanol, measured at 370nm. Retention times for rutin, sutherlandin A, sutherlandin B, kaempferol-3-O-rutinoside, sutherlandin C, sutherlandin D, quercitrin, quercetin and kaempferol were 11.9, 12.7, 13.8, 15.3, 16.2, 17.0, 18.0, 26.2 and 28.1 minutes, respectively.
Figure 2D: HPLC chromatogram of the nine reference compounds in 50% aqueous methanol, measured at 370nm. Retention times for rutin, sutherlandin A, sutherlandin B, kaempferol-3-O-rutinoside, sutherlandin C, sutherlandin D, quercitrin, quercetin and kaempferol were 11.9, 12.7, 13.8, 15.3, 16.2, 17.0, 18.0, 26.2 and 28.1 minutes, respectively.
Figure 2E: HPLC chromatogram of the nine reference compounds in 50% aqueous methanol, measured at 370nm. Retention times for rutin, sutherlandin A, sutherlandin B, kaempferol-3-O-rutinoside, sutherlandin C, sutherlandin D, quercitrin, quercetin and kaempferol were 11.9, 12.7, 13.8, 15.3, 16.2, 17.0, 18.0, 26.2 and 28.1 minutes, respectively.
Discussion
To the best of our knowledge, this is the first case of an established chondroblastoma which eventually transformed into conventional osteosarcoma in a non radiated limb. Although there may be argument that the earlier disease might have been osteosarcoma from the beginning, we defer to disagree as the patient was well for 4 years before he developed a local recurrence. Naturally in osteosarcoma with no chemotherapy on board, the patient would have succumbed within 2 years of the initial disease.
Aggresiveness in chondroblastoma can be subdivided into 3 types; malignant chondroblastoma, benign chondroblastoma with lung metastases and benign chondroblastoma with subsequent development of high grade malignancy. Subsequent development of malignancy is common in post irradiation cases, however a benign chondroblastoma subsequently presenting as a high grade sarcoma is the rarest among all of them [7]. To the best of our knowledge there has been only 2 cases reported so far (Table 1).
| CASE | DESCRIPTION | YEAR REPORTED |
|---|---|---|
| case 1 | Benign chondroblastoma changing to undiffentiated sarcoma after 8 years | 1970 |
| Case 2 | Benign chondroblastoma pelvis changing to unspecified sarcoma after 10 years | 1979 |
Table 1: Cases of chondroblastoma eventually presenting as sarcoma with no history of radiation.
Chondroblastoma
Chondrobalstomas are a rare benign bone lesions that predominantly occurs in growing bone at the epiphyseal region. It is histologically marked by presence of chondroblast arranged in chickenwire pattern with presence of multinucleated giant cell and mononuclear stromal cells [8]. They are treated by curretage and bone grafting or cementation. They carry a local recurrence rate of 8 to 40 percent [4,5]. Study of the histone mutation in chondroblastoma indicated that p.Lys36Met alteration predominantly occurred in H3F3B gene in majority of the chondroblastoma cases, whereas p.Gly34Trp mutations are dominated in the H3F3A gene [9]. As the histone H3 variant H3.3 is able to regulate the patterns of DNA methylation at the gene body [10], it is possible that the mutated H3.3 in chondroblastic initially alters DNA methylation status and further leads to the development of chondroblastoma in patients. In mammals, since DNA methyltransferases (DNMTs) and some histone modifiers, including H3K9 methyltransferases G9a and GLP, are essential for the establishment and maintenance of DNA methylation at heterochromatin loci [11,12] investigation the interact of H3.3 and the above enzymes might create a novel direction for understanding the genesis and progression of chondroblastoma.
Malignant chondroblastoma
The term “malignant” is probably misnomer. In fact, Aycan et al., termed “malignant chondroblastoma” as a histologically benign lesion. The term “malignant” denotes its metastatic potential and aggressive behavior rather than histological malignancy [13]. Approximately 2% of benign chondroblastoma do metastases to lung. The metastatic lesion in lung carries similar morphology of being benign as well. The term malignant chondroblastoma is synonymous with aggressive chondroblastoma and metastatic chondroblastoma; none of which are histologically malignant.
Malignant trasformation of a chondroblastoma
Malignant trasformation of chondroblastoma is defined as sarcoma arising in a previous chondroblastoma site. It can be subdiveded into 2 more groups; post irradiation sarcoma and “secondary” sarcoma at previous chondroblastoma site. When it comes to chondroblastoma, the “malignant” part of it is probably not as clearly defined as Giant Cell Tumour. Malignancy in GCT is divided into primary malignant GCT and secondary malignant GCT. Primary malignant GCT is defined as high grade sarcoma arising side by side a benign GCT and secondary malignant GCT is a high grade sarcoma arising in a previous benign GCT site. Post radiation sarcoma is the commonest type of secondary malignant GCT [14]. This probably can be used for chondroblastoma but due to its rarity there has not been any formal classification of this sort before. In fact, there has only been 2 cases of sarcoma arising in previous chondroblastoma site (Table 1). Our case is probably the first ever case of a secondary osteosarcoma arising at a previous chondroblastoma site.
Chondroblastoma like osteosarcoma
A rare variant of osteosarcoma known as chondroblastoma like ostesarcoma has been described first in 1990 by Schajowicz et al. [15]. It is a rare variant of osteosarcoma that commonly occurs in the bone of the foot. It is thought to be less than 1% of all osteosarcoma. It is often misdiagnosed as benign lesion and probably accounted for many of the “malignant” or “aggressive” chondroblastoma that were reported before 1990. In 1985, Michael Kyriakos, reported a case of aggressive malignant chondroblastoma which presented with lung metastasis which eventually killed the patient [11]. They did emphasis, while most malignant or aggressive behavior occurs after some surgical intervention, this case was not such as it was malignant from presentation. It is cases like this that makes us wonder if they were probably chondroblastoma like osteosarcoma from the onset thus the aggressive behavior. Its not till the next 5 years before this entity is first described in 1990. As for now, we probably poorly understand chondroblastoma like osteosarcoma due to its extremely rare occurance.
To conclude, this case has been a unique and challenging case for us. It is definitely very interesting to find out that a merely benign chondroblastoma can present as an aggressive osteosarcoma after 4 years of being “disease free”. The subsequent disease being very aggressive, presenting with lung metastasis and proved to be fatal despite patient being on chemotherapy.
References
- Jaffe HL, Lichtenstein L (1942) Benignchondroblastoma of bone: a reinterpretation of the so-called calcifying or chondromatous giant cell tumor. The American journal of pathology 18: 969.
- Elek EM, Grimer RJ, Mangham DC, Davies AM, Carter SR, et al. (1998) Malignant chondroblastoma of the oscalcis. Sarcoma 2: 45-48.
- Xie C, Jeys L, James SL (2015) Radiofrequency ablation of chondroblastoma: long-term clinical and imaging outcomes. European radiology 25: 1127-1134.
- Springfield DS, Capanna R, Gherlinzoni F, Picci P Campanacci M (1985) Chondroblastoma: A review of seventy cases. J Bone Joint Surg Am 67: 748-755.
- Lin , Thenaan A, Deavers MT, Lewis VO, Yasko AW (2005) Treatment and prognosis of chondroblastoma. Clinical orthopaedics and related research 438: 103-109.
- Sirsat MV, Doctor VM (1970) Benignchondroblastoma of bone. Bone & Joint Journal 52: 741-745.
- Kyriakos M, Land VJ, Penning HL, Parker SG (1985) Metastatic chondroblastoma. Report of a fatal case with a review of the literature on atypical, aggressive, and malignant chondroblastoma. Cancer 55: 1770-1789.
- Aycan OE, Vanel D, Righi A, Arikan Y, Manfrini M (2015) Chondroblastoma-like osteosarcoma: a case report and review. Skeletal radiology 44: 869-873.
- Behjati S, Tarpey PS, Presneau N, Scheipl S, Pillay N, et al. (2013). Distinct H3F3A and H3F3B driver mutations define chondroblastoma and giant cell tumor of bone. Nature genetics 45: 1479-1482.
- Wollmann H, Stroud H, Yelagandula R, Tarutani Y, Jiang D, et al. (2017) The histone H3 variant H3. 3 regulates gene body DNA methylation in Arabidopsis thaliana. Genome biology 18: 94.
- Bird A (2002) DNA methylation patterns and epigenetic memory. Genes & development 16: 6-21.
- Zhang T, Termanis A, Özkan B, Bao XX, Culley J, et al. (2016) G9a/GLP complex maintains imprinted DNA methylation in embryonic stem cells. Cell reports 15: 77-85.
- Duttaluri R, Sultanpurkar GP, Raorane H, Vikram H (2016) Malignant chondroblastoma of extra skeletal origin. International Journal of Alied and Basic Medical Research 6: p146.
- Bertoni F, Bacchini P, Staals El (2003) Malignancy in Giant Cell Tumour of Bone. Cancer 97: 2520-2529.
- Schajowicz F, de Próspero JD, Cosentino E (1990) Case report 641. Skeletal radiology 19: 603-606.
Relevant Topics
- 3D Printing in Limb-Sparing Surgery
- Adamantinoma
- Aneurysmal Bone Cysts
- Chondrosarcoma
- Chordomas
- Cryosurgery
- Enchondroma
- Ewing’s Sarcoma
- Fibrous Dysplasia
- Giant Cell Tumor of Bone
- Immunotherapy for Osteosarcoma
- Liquid Biopsy in Orthopedic Oncology
- Malignant Osteoid
- Metastatic Bone Cancer
- Molecular Profiling of Bone Tumors
- Multilobular Tumour of Bone
- Orthopaedic Oncology
- Osteocartilaginous Exostosis
- Osteochondrodysplasia
- Osteoma
- Osteonecrosis
- Osteosarcoma
- Primary Bone Tumors
- Sarcoma
- Secondary Bone Tumours
- Targeted Therapy in Bone Sarcomas
- Tumours of Bone
Recommended Journals
Article Tools
Article Usage
- Total views: 4000
- [From(publication date):
September-2017 - Jul 12, 2025] - Breakdown by view type
- HTML page views : 3110
- PDF downloads : 890