Spontaneous Common Bile Duct Perforation: A Rare Cause of Biliary Peritonitis in a Patient of Chronic Calcific Pancreatitis
Received: 21-Feb-2022 / Manuscript No. JGDS-22-55029 / Editor assigned: 23-Feb-2022 / PreQC No. JGDS-22-55029(PQ) / Reviewed: 09-Mar-2022 / QC No. JGDS-22-55029 / Revised: 14-Mar-2022 / Manuscript No. JGDS-22- 55029(R) / Published Date: 21-Mar-2022 DOI: 10.4172/2161-069X.1000673
Abstract
Spontaneous perforation of common bile duct is a rare cause of acute generalized peritonitis. It is difficult to diagnose preoperatively and mainly caused due to increased intra-ductal pressure of common bile duct, which can occur due to stone, stricture or malignancy.
Here, we present an interesting case report of spontaneous common bile duct perforation in a patient of chronic calcific pancreatitis leading to peritonitis, the management protocol with highlight on previous literature.
Keywords: Chronic calcific pancreatitis; Biliary peritonitis; Spontaneous CBD perforation; Rare cause of peritonitis; Isolated CBD perforation
Introduction
Spontaneous perforation of common bile duct (CBD) is an infrequent cause of acute generalised peritonitis [1]. Other common causes being peptic ulcer disease complicated by duodenal or gastric perforation and unusually by gall bladder perforation. It is almost always diagnosed intra operatively and it is a rare entity in adults. The common causes are increased intraductal pressure due to stone, tumour, stricture and erosion of a biliary diverticulum. The incidence of common bile duct obstruction among patients with chronic pancreatitis range from 3% to 23% [2]. Till date only three cases of spontaneous common bile duct perforation with peritonitis as a complication in chronic pancreatitis has been reported [3]. We report an interesting case of spontaneous common bile duct perforation in a middle aged male with chronic calcific pancreatitis and review literature of such cases.
Case Report
A 35 year old male patient was referred from a private hospital as a nonsettling case of acute on chronic pancreatitis being managed conservatively for the last 4 days. Patient had complaints of generalised pain abdomen with multiple episodes of vomiting.
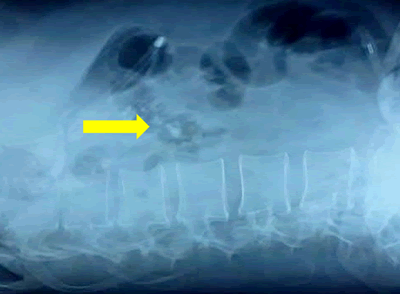
On examination he was sick looking and dehydrated with tachycardia, tachypnoea and was normotensive. On examination, the abdomen was distended and tender with presence of free fluid and absent bowel sounds. Initial investigations revealed haemoglobin 15.1 gm/dL, white cell count 27,100/cumm with 94% segmented neutrophils, serum bilirubin was 1.84 mg/dL, transaminases and alkaline phosphatase (ALP) were normal. Serum Amylase and Lipase were 321 U/L and 393 U/L respectively. Ultrasound abdomen showed moderate ascites with multiple pancreatic calcifications. Chest X-ray was normal and abdominal X-ray showed evidence of ileus with calcification in the region of pancreas (Figure 1, yellow arrow) with no evidence of air under diaphragm. Contrast enhanced Computed Tomography (CECT) of abdomen showed features of acute exacerbation with chronic calcific pancreatitis with multiple intraluminal calculi and normal common bile duct. Diagnostic paracentesis showed bilious fluid.
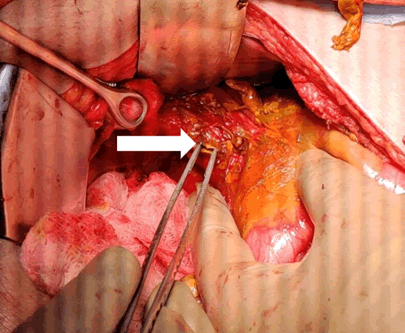
With the provisional diagnosis of biliary peritonitis, patient was taken up for explorative laboratory. Upon exploration, 1.5 litres of bilious peritoneal fluid was aspirated, omentum was studded with calcifications. The duodenum and stomach were normal. Gallbladder was intact and didn't contain any calculus. The common bile duct was mildly dilated 8 mm with a perforation of 5 x 5 mm in supraduodenal part (Figure 2, white arrow). It didn’t contain any calculus and distal patency was maintained. Cholecystectomy with primary closure of common bile duct perforation was done.
Post-operative Magnetic Resonance Cholangiopancreatography (MRCP) showed smooth tapering of CBD into duodenum with acute on chronic mass forming pancreatitis with multiple calculi in pancreatic duct.
Patient had an uneventful postoperative recovery and was discharged on 6th post-operative day.
Discussion
Spontaneous extrahepatic bile duct perforation is a rare entity. Since its first description by Freeland in 1882 only 90 cases have been reported in infancy and 97 cases in adults [4]. Pathogenesis of spontaneous CBD perforation is not clearly understood. Proposed mechanisms are increased intraductal pressure due to stone, stricture and tumour and weak CBD wall due to pancreatic juice reflux, Anomalous Pancreaticobiliary Junction (APBJ), choledochal cyst and connective tissue disorders. Complications of chronic pancreatitis are pseudocyst (25%), CBD obstruction (3%-23%), duodenal obstruction (0.5%-13%), pancreatic fistula and malignancy [2]. Chronic pancreatitis presenting as biliary peritonitis secondary to CBD perforation to our knowledge has only been reported three times and all three were in paediatric age group and had impacted pancreatic calculus at duodenal papilla [3] and one patient had APBJ [5].
Presentation is usually insidious with diffuse abdominal pain, vomiting, jaundice and patient is usually septic with raised white cell counts. Bilirubin and transaminases are seldom deranged [6]. Absence of air under diaphragm with moderate ascites with normal gall bladder on ultrasound with a diagnostic ascetic tap showing bile should raise a suspicion of bile duct perforation. CECT abdomen is rarely informative of CBD perforation. Endoscopic Retrograde Cholangiopancreatography (ERCP) and MRCP to delineate biliary and pancreatic anatomy and Radio-nucleotide study demdemonstrating tracer in peritoneum is diagnostic but it is rarely done due to non-availability and lack of suspicion. ERCP with stenting across perforation can be done if perforation is diagnosed preoperatively. Reports of two cases managed with ERCP are available [7]. Spontaneous CBD perforation is almost always diagnosed intraoperatively and is usually managed with cholecystectomy with CBD exploration with primary repair or repair over T-tube [1]. In our case, primary repair of CBD was done after confirming distal patency with post-operative MRCP. Biliary-enteric anastomosis is usually unwarranted in the emergency setting with grossly inflamed tissues.
Conclusion
Spontaneous bile duct perforation leading to biliary peritonitis is an uncommon diagnosis in the setting of chronic pancreatitis, but this differential should be sought when a case of suspected acute on chronic pancreatitis has diffuse peritonitis with bile in a diagnostic paracentesis. MRCP and biliary scintigraphy aid in preoperative diagnosis. Early diagnosis and management is must owing to its high mortality and morbidity.
References
- Khanna R, Agarwal N, Singh AK, Khanna S, Basu SP (2010) Spontaneous common bile duct perforation presenting as acute abdomen. Indian J Surg 72(5):407-408.
[CrossRef] [Google Scholar] [Pubmed]
- Vijungco J, Prinz R (2003) management of biliary and duodenal complications of chronic pancreatitis. World J Surg 27:1258-1270.
[CrossRef] [Google Scholar] [Pubmed]
- Kumar A, Kataria R, Chattopadhyay TK, Karak PK, Tandon RK (1992) Biliary peritonitis secondary to perforation of common bile duct: An unusual presentation of chronic calcific pancreatitis. Post grad Med J 68(804):837-9.
[CrossRef] [Google Scholar] [Pubmed]
- Kang Sung-Bum, Han Ho-Seong, Seog Ki Min, Kook Lee Hyeon (2004) Nontraumatic perforation of the bile duct in adults. Arch Surg 10:1083-7.
[CrossRef] [Google Scholar] [Pubmed]
- Shenoy V, Jawale S (2001) Anomalous pancreaticobiliary union and chronic pancreatitis: Rare presentation with biliary peritonitis. Pediatr Surg Int 17:549-551.
[CrossRef] [Google Scholar] [Pubmed]
- Hamura R, Haruki K, Tsutsumi J, Takayama S, Shiba H, et al (2016) Spontaneous biliary peritonitis with common bile duct stones: Report of a case. Surg Case Rep 2(1):103.
[CrossRef] [Google Scholar] [Pubmed]
- Barrett HB, Narkewicz MR, Ronald SJ (2006) Spontaneous Perforation of the Bile Duct in a Toddler: The Role of Endoscopic Retrograde Cholangiopancreatography in Diagnosis and Therapy. J Pediatr Gastroenterol Nutr 43(5):695-697.
[CrossRef] [Google Scholar] [Pubmed]
Citation: Rajdev V, Nandakumar BM, Gupta R, Chandel P, Gupta J (2022) Spontaneous Common Bile Duct Perforation: A Rare Cause of Biliary Peritonitis in a Patient of Chronic Calcific Pancreatitis. J Gastrointest Dig Syst.12:673 DOI: 10.4172/2161-069X.1000673
Copyright: © 2022 Rajdev V, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3293
- [From(publication date): 0-2022 - Apr 28, 2025]
- Breakdown by view type
- HTML page views: 2718
- PDF downloads: 575