Splenic Hematoma after Colonoscopy in a Patient with Protein S Deficiency Managed with Prophylactic Splenic Angioembolization
Received: 20-Jun-2022 / Manuscript No. JGDS-22-67006 / Editor assigned: 22-Jun-2022 / PreQC No. JGDS-22-67006 (PQ) / Reviewed: 06-Jul-2022 / QC No. JGDS-22-67006 / Revised: 11-Jul-2022 / Manuscript No. JGDS-22-67006 (R) / Published Date: 18-Jul-2022 DOI: 10.4172/2161-069X.1000691
Abstract
Splenic hematoma is a rarely reported complication of colonoscopy. Traction of the splenocolic ligament is the most commonly implicated mechanism leading to this complication. Long term use of anticoagulation is an independent risk factor for splenic injury. We hereby report the first case of splenic hematoma as a complication of colonoscopy in a patient with Protein S deficiency on long term anticoagulation. The patient is a 51 year old female who presented 4 days after screening colonoscopy with increasing left upper quadrant abdominal pain that started within 24 hours of colonoscopy. The diagnosis was confirmed with a CT scan. She was hemodynamically stable with Grade II splenic hematoma managed with prophylactic splenic angioembolization.
Keywords: Splenic hematoma; Colonoscopy; Protein S deficiency; Angioembolization; Anticoagulation
Introduction
Colonoscopy is routine procedure performed for diagnostic as well as screening purposes of colorectal cancer. Recently, there has been a substantial rise in the number of colonoscopies performed annually for screening in individuals aged 50-75 years, with 64 million colonoscopies being performed alone in 2020 in the United States [1]. Although considered to be relatively safe, common complications after screening colonoscopy include perforation and post-colonoscopy bleeding [2]. Splenic hematoma is a very rare but a high risk complication of colonoscopy likely secondary to traction on the splenocolic ligament during the passage of the scope [3]. After a thorough review of literature, to the best of our knowledge, this is the first reported case of splenic hematoma status post colonoscopy in a patient with Protein S deficiency which was managed with prophylactic splenic embolization.
Case Presentation
A 50 year old female presented with chief complaint of left upper quadrant abdominal pain for 4 days. Patient had a past medical history significant for Protein S deficiency associated with unprovoked left lower extremity Deep Vein Thrombosis (DVT) and an episode of Pulmonary Embolism (PE) at the age of 19 years and another episode of unprovoked left lower extremity deep vein thrombosis at the age of 39 years. Patient was on anticoagulation with warfarin initially and was later switched to lifelong apixaban after the episode of DVT at 39 years of age.
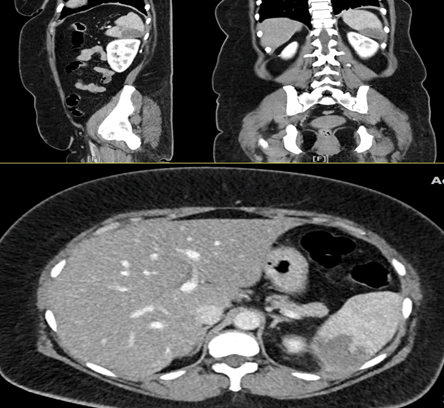
Patient went for a colonoscopy four days prior to her presentation. She acknowledged left upper quadrant pain within 24 hours of colonoscopy. Anticoagulation was held for 48 hours prior to the colonoscopy. Her only other complaint was of nausea. Patient was hemodynamically stable on presentation and on examination was found to have exquisite left upper quadrant tenderness. Given the location of the pain, splenic etiology was likely and hence CT scan of abdomen and pelvis with IV contrast was obtained. Results were consistent with 3.9 x 3.5 x 2.7 cm hypodensity in the inferior pole of the spleen which was not present on patient’s previous scans (Figure 1). Thus, the diagnosis of splenic hematoma was established. Patient was considered high risk given the nature of her presentation. She presented to a community hospital on a weekend where there was no 24 hour interventional radiology service, hence attempts were made to by the emergency department to transfer the patient to a tertiary center. However, none of the hospitals had beds available and thus she was admitted to the internal medicine service at the community hospital.
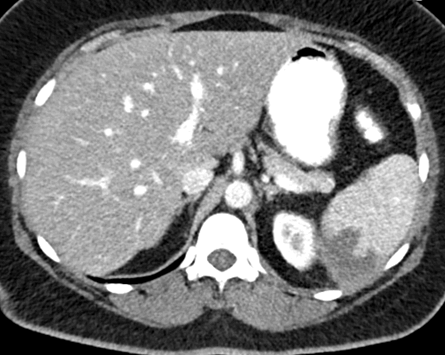
She had a grade 2 hematoma of the spleen and the current literature for management would recommend close observation of the patient with hemoglobin levels every 6 hours along with 24 hour interventional radiology back up for embolization if needed. This was complicated in this patient due to her history of protein S deficiency and risk of DVT/PE, which is why anticoagulation could not be held for a long duration, but resuming anticoagulation increased the risk of worsening splenic hemorrhage. Since there was no interventional radiology available over the weekend, management options of splenectomy versus observation were considered and a decision was made, in agreement with the patient, to treat conservatively. She was initially kept nil per orally and her CBC was checked every 6 hours which remained stable. Frequent and periodic abdominal examinations were conducted and no further worsening was noted. Repeat CT scan of the abdomen and pelvis with IV contrast was done 12 and 48 hours after initial CT scan and it showed stable hematoma (Figure 2). Once interventional radiology team became available, management options of prophylactic embolization of the spleen vs continued observation were discussed in conjunction with surgery, interventional radiology and hematology/ oncology. Given patient’s Protein S deficiency and her need to be restarted on anticoagulation, decision was made to offer the patient prophylactic embolization. Her splenic capsule was not very strong given her age and she was at high risk for sudden splenic rupture if anticoagulation was restarted. Consent was obtained and prophylactic embolization of the spleen was pursued. Embolization was completed with embo-coils and mesenteric angiogram performed showed no evidence of blush or pseudoaneurysm formation in splenic artery or its branches shown in (Figure 3). Patient continued to have pain for 2 days post procedure after which the pain significantly improved. Follow up after 2 months of procedure was completed and she continued to be pain free and without any complications.
Discussion
Splenic hematoma is a rare but serious complication of colonoscopy. Laanani et al in their study noted the incidence of splenic injury to be about 0.20 to 0.34 per 10000 colonoscopies. Another study by Ha et al also reports the incidence to be between 0.00005%-0.017% [4,5]. However, Ko et al did a prospective study of 21,735 patients undergoing screening colonoscopy and found only 1 patient to have developed splenic hematoma [6].
Exact mechanism pertaining to such an injury is yet to be fully established although various theories are in place, most common being injury to the splenocolic ligaments. Another mechanism implicated is trauma during maneuvering of the colonoscope at the splenic flexure causing injury to the splenic capsule mimicking a blunt abdominal trauma. Most common presenting symptom is abdominal pain with Ha et al in their review of 66 patients with splenic injury in colonoscopy finding 74% of the patients to have developed abdominal pain and 55.8% patients presented to the hospital within the first 24 hours [5,7,8]. Our patient did endorse the beginning of the pain 24 hours after the colonoscopy but presented after 4 days when pain got worse. CT scan is the preferred imaging modality as it also entails the grading which decides the management plan [9].
Anticoagulation is an independent risk factor for spontaneous as well as triggered splenic injury. Bassler et al in their study of 613 cases of splenic rupture between 1950 to 2011 in patients without any risk factors found anticoagulation to be independently contributing in 21 cases. With the use of anticoagulation being wide amongst patients with atrial fibrillation, deep vein thrombosis and pulmonary embolism, it’s role in contributing towards serious complications like splenic injury after elective procedures cannot be neglected even if anticoagulation is held for appropriate recommended interval before the procedure [10].
Grading of splenic hematoma is based on its diameter if the lesion is intraparenchymal and on its involvement of the surface area if the lesion is subcapsular [11]. According to the AAST classification, this patient had a grade 2 splenic hematoma. Current guidelines for the management of hemodynamically stable AAST grade 2 splenic hematoma such as our patient include non-operative management with serial clinical/laboratory and radiological evaluations. Angioembolization is indicated if there is CT evidence of contrast blush, pseudo-aneurysm or arteriovenous fistula. In the absence of these findings, angioembolization can be considered if blush was previously noted on CT scan or there are signs of persistent hemorrhage after having ruled out extra splenic source of bleeding. It can also be considered in the presence of risk factors for failure of non-operative management [12]. Proximal splenic artery embolization is the procedure which is usually selected in patients with splenic trauma because of its advantages over distal splenic artery embolization in terms of reduced procedure time, radiation dose and incidence of small splenic infarcts. Targeted site for embolization is usually between dorsal and great pancreatic artery [13]. This has the advantage of preserving splenic perfusion and thus its immunologic function via collaterals. Schimmer et al in a systematic review of 12 observational studies did not find any Overwhelming postsplenectomy infection (OPSI) reported after splenic embolization proving preserved splenic function and thus making it a preferable procedure over splenectomy in hemodynamically stable patients [14].
Even with such wide indications and implications for angioembolization, Ullah et al in their case review of splenic injury after colonoscopy till April 2019 found only 4 cases to have been managed with proximal splenic artery embolization [15]. Our patient did not have the CT evidence of blush, pseudoaneurysm or fistula. She did not have any significant change in clinical, laboratory and radiological evaluation for the initial 48 hours after presentation. Angioembolization was however performed in our case as she had Protein S deficiency and anticoagulation needed to be resumed to prevent further episodes of DVT and PE. This was considered to be a significant risk factor of non-operative management (NOM) as resumption of anticoagulation would put her at risk of splenic rupture in the setting of a weak splenic capsule.
Conclusion
Splenic injury is a life threatening complication of colonoscopy although it is not very well recognized likely due to under reporting of the cases, with possible higher numbers in patients with ongoing anticoagulation. Management of AAST grade I and II splenic hematoma that are hemodynamically stable include NOM with angioembolization usually indicated if CT findings of blush, pseudoaneurysm or fistula are not present. However, for patients who are at high risk of failure of NOM like patients on long term anticoagulation in whom holding anticoagulation for prolonged period of NOM would increase the risk of systemic clot formation, prophylactic angioembolization needs to be considered for safe and early resumption of anticoagulation. Large scale studies are needed for guidelines on management of low grade splenic hematoma that have risk factors for failure of NOM, such as need for long term anticoagulation.
References
- CDC (2020) Use of colorectal cancer screening tests.
- Reumkens A, Rondagh EJ, Bakker CM, Winkens B, Masclee AA, et al. (2016) Post colonoscopy complications: A systematic review time trends, and meta-analysis of population based studies. Am J Gastroenterol 111(8):1092-101.
[Crossref] [Google Scholar] [PubMed]
- Patel DD, Shih-Della Penna DC, Terry SM (2020) Splenic trauma from colonoscopy: A case series. Int J Surg Case Rep 71:30-33.
[Crossref] [Google Scholar] [PubMed]
- Laanani M, Coste J, Blotière PO, Carbonnel F, Weill A (2019) Patient, procedure, and endoscopist risk factors for perforation, bleeding and splenic injury after colonoscopies. Clin Gastroenterol Hepatol 17(4):719-727.
[Crossref] [Google Scholar] [PubMed]
- Ha JF, Minchin D (2009) Splenic injury in colonoscopy: A review. Int J Surg 7(5):424-7.
- Ko CW, Riffle S, Michaels L, Morris C, Holub J, et al. (2010) Serious complications within 30 days of screening and surveillance colonoscopy are uncommon. Clin Gastroenterol Hepatol 8(2):166-73.
[Crossref] [Google Scholar] [PubMed]
- D'Orazio B, Cudia B, Martorana G, Di Vita G, Geraci G (2020) Conservative treatment of splenic haematoma after colonoscopy: A case report. Cureus 12(9):e10531.
[Crossref] [Google Scholar] [PubMed]
- McBride R, Dasari B, Magowan H, Mullan M, Yousaf M, et al.(2013) Splenic injury after colonoscopy requiring splenectomy. BMJ Case Rep 2013:bcr2013009126.
[Crossref] [Google Scholar] [PubMed]
- Janes SE, Cowan IA, Dijkstra B (2005) A life threatening complication after colonoscopy. BMJ 330(7496):889-90.
[Crossref] [Google Scholar] [PubMed]
- Aubrey-Bassler FK, Sowers N (2012) 613 cases of splenic rupture without risk factors or previously diagnosed disease: A systematic review. BMC Emerg Med 14:11-12.
[Crossref] [Google Scholar] [PubMed]
- Gaillard F, Jones J (2022) AAST spleen injury scale. Reference article, Radiopaedia.org.
- Coccolini F, Montori G, Catena F, Kluger Y, Biffl W, et al. Splenic trauma: WSES classification and guidelines for adult and pediatric patients. World J Emerg Surg 18:51-4.
[Crossref] [Google Scholar] [PubMed]
- Quencer KB, Smith TA (2019) Review of proximal splenic artery embolization in blunt abdominal trauma. CVIR Endovasc 2(1):11.
[Crossref] [Google Scholar] [PubMed]
- Schimmer JA, van der Steeg AF, Zuidema WP (2016) Splenic function after angioembolization for splenic trauma in children and adults: A systematic review. Injury 47(3):525-30.
[Crossref] [Google Scholar] [PubMed]
- Ullah W, Rashid MU, Mehmood A, Zafar Y, Hussain I, et al. (2020) Splenic injuries secondary to colonoscopy: Rare but serious complication. World J Gastrointest Surg 12(2):55-67.
[Crossref] [Google Scholar] [PubMed]
Citation: Raval M, Suhail F, Sanghvi L, Patel S, Campbell M (2022) Splenic Hematoma after Colonoscopy in a Patient with Protein S Deficiency Managed with Prophylactic Splenic Angioembolization. J Gastrointest Dig Syst 12:691. DOI: 10.4172/2161-069X.1000691
Copyright: © 2022 Raval M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2863
- [From(publication date): 0-2022 - Dec 19, 2025]
- Breakdown by view type
- HTML page views: 2391
- PDF downloads: 472