Commentary Open Access
Socio-Ecological Approach to Self-Management of HIV/AIDS: A Case Study of Women Patients with HIV Virus
Rashid M Ansari1*, Saiqaa Y Ansari2, Saher Al-Safarini3 and Muhammad Ayub41Department of General Practice, School of Primary Health Care , Monash University, Melbourne, Australia
2General Practitioner, Department of Endocrinology and Diabetes, Dallah Hospital, Riyadh, Saudi Arabia
3Senior Consultant, Head of Department of Endocrinology and Diabetes, Riyadh, Saudi Arabia
4Head of Physiology Department, Ayub Medical College, Peshawar, Pakistan
- *Corresponding Author:
- Rashid M Ansari
Department of General Practice
School of Primary Health Care
Monash University, Melbourne, Australia
E-mail: ansarirm@yahoo.com
Received date: August 23, 2013; Accepted date: October 22, 2013; Published date: October 29, 2013
Citation: Ansari RM, Ansari SY, Al-Safarini S, Ayub M (2013) Socio-Ecological Approach to Self-Management of HIV/AIDS: A Case Study of Women Patients with HIV Virus. Occup Med Health Aff 1:136. doi: 10.4172/2329-6879.1000136
Copyright: © 2013 Ansari RM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Occupational Medicine & Health Affairs
Abstract
Pakistan is perceived as a ‘high risk low prevalence country’ in relation to HIV/AIDS virus and the indication is that there is a rise in HIV/AIDS cases in the ‘high risk groups’ with concentrated epidemics beginning in marginalized population like the intravenous drug users in Karachi, which have a high potential of being passed onto the general population due to a closely weaved social network. Pakistani women are more vulnerable to HIV/AIDS infection due to biological and socio-economic factors, especially gender inequality. Since women in the country in general have lower socio-economic status, less mobility and lack of decision-making power, all of these factors further contribute to their HIV vulnerability. The literacy rate is much lower among females (41%) than males (64%) and while literacy presents an obstacle for HIV/AID preventive efforts in general, it is also much difficult to reach women with information about how they can prevent themselves from HIV infection. The present case study examines the case of women patients (n=12) with HIV virus in Pakistan. This study analyses how the health issue related to HIV/AIDS is viewed and addressed in community and identifies the barriers to HIV/AIDS care in community and healthcare clinics and recommends socio-ecological approach to self-management of HIV/AIDS and structural approach to HIV prevention
Introduction
Pakistan is perceived as a ‘high risk low prevalence country’ in relation to HIV/AIDS virus [1]. The indication is that there is a rise in HIV/AIDS cases in the ‘high risk groups’ with concentrated epidemics beginning in marginalized population like the intravenous drug users in Karachi, which have a high potential of being passed onto the general population due to a closely weaved social network [1]. The overall prevalence of HIV infection in adults aged 15 to 49 is 0.1% but majority of cases go unreported due to social taboos about sex and victims’ fears of discrimination and it is reported that the ratio of HIV positive males to females is 7:1 [2]. Despite the low prevalence rate of HIV/AIDS, the existence of a number of high risk sexual behaviour among general population, internal and external migration, unsafe and invasive medical practices and inadequate health and social services are some of the factors increasing the risk of a generalized HIV epidemic in the country [3].
Pakistani women are more vulnerable to HIV/AIDS infection due to biological and socio-economic factors, especially gender inequality [2]. Since women in the country in general have lower socio-economic status, less mobility and lack of decision-making power, all of these factors further contribute to their HIV vulnerability. For example, because of gender disparities in educational enrolment, the literacy rate is much lower among females (41%) than males (64%) and while literacy presents an obstacle for HIV/AID preventive efforts in general, it is also much difficult to reach women with information about how they can prevent themselves from HIV infection [1]. In addition, restrictions on mobility often make it difficult for women to access health and social services, including basic reproductive health care services, cultural traditions prevent women from consulting male doctors, women’s decision making power is somehow restricted to negotiate with their partners for safer sexual practices such as faithfulness, abstinence, or using condoms.
Case study of women patients with HIV/AIDS
The present case study examines the case of women patients (n=12) with HIV virus in Pakistan. These patients were selected from the four provinces representing the overall status of health care system of Pakistan in relation to HIV/AIDS. This study analyzes how the health issue related to HIV/AIDS is viewed and addressed in community and identifies the barriers to HIV/AIDS care in community and healthcare clinics and recommends socio-ecological approach to self-management of HIV/AIDS and structural approach to HIV prevention.
HIV/AIDS is now widely accepted as a chronic illness and, as such, requires ongoing primary care management [4,5]. Most chronic illnesses, such as diabetes, asthma, and arthritis, require adherence to some type of treatment regimen, and they typically involve self-care (self-monitoring of symptoms) on the part of the patient. However, there are several factors which make the management of HIV/AIDS different and more difficult from other chronic diseases. In this case study, we will explore these factors in the context of self management of HIV/AIDS and follow the appropriate guidelines to look into this case study. We have explained to the patients the nature of this study and sent them the information sheet and the list of questions (Appendix I) and obtained their consent to the interview.
Summary of the case study
The patients mentioned that health services in the community are not addressing the issues related to HIV/AIDS and there is no regular programme for management of this disease in any nearby clinics in the area and access to community-based doctors is not easy for this disease. Therefore, in the absence of medical support facilities, adherence to antiretroviral regimens is complex and often poor due to rigid adherence requirements, dietary guidelines and side effects. Also, daily self-monitoring of HIV/AIDS is difficult due to the nature of the disease itself. In family and community, it is perceived as self-inflicted problem and there is stigma attached to this disease and the discrimination in that society in terms of social isolation is very severe. There is no support from their husbands from whom they have actually acquired the virus after the marriage; but being women, they are the ultimate victims of discrimination and sometimes to violence and abuse in that society and culture.
Ecological Approach to Self-Management
This case study suggests that the patients are solely responsible to take care of their HIV/AIDS related problems and its management and therefore the issue of self-management becomes more important for those with chronic disease, where only the patient can be responsible for day to day care over the length of the illness [6]. It is generally agreed that self-management is required for control of chronic diseases and for prevention of disease complications; however, patients generally do not adhere to self-management recommendations [7,8]. The adherence to the recommendations and barriers are both problematic for “lifestyle” behaviour such as eating patterns and physical activity [9]. This is evident from the case study that adherence to antiretroviral regimens was difficult and often poor due to rigid adherence requirements, lack of medical facilities, dietary guidelines and side effects.
There is compelling evidence that higher levels of social support are related to better long-term self management and better health outcomes [10,11]. There is also a significant relationship between support and health where support can be assessed from variety of sources, including spouses, family, friends and neighbors [12]. The relationships between support and immunity [13], health status and health behaviors mortality and quality of life have also been reported [14,15].
Health services in the community
It has been mentioned in the summary of the case study that health services in the community are not adequate and that there is no health management programme in the community health clinics to provide help to people infected with HIV virus. At the government level, there is no policy to ensure that people living with HIV/AIDS in remote areas are involved in planning, implementation and evaluation of HIV/AIDS prevention, care and support services. Information on HIV/AIDS among education providers is very low and in remote areas there is very little access to information related to HIV/AIDS. One of the patients told us during interview that….“I have no idea where to go and whom to see, visiting medical centers in capital cities is very expensive and time consuming and not supported by the family…”
However, it has been reported that five medical centers have been established in capital cities to provide treatment and hospitalization for HIV infected people. The current statistics suggest that only 7.4% people with HIV infection have received antiretroviral from these centers in 2005 [16]. The government of Pakistan has recently passed the ‘HIV/AIDS Prevention Act” focusing on providing care, support and equitable access to treatment for people living with HIV/AIDS, services for vulnerable population, services and information for reducing stigma and discrimination against the people with HIV/ AIDS, and services to women vulnerable to HIV infection and improve their access to HIV specific knowledge and preventive services [16].
Interventions to improve health services in the community
The health services in the community can be improved by making use of on-going follow-up and support for the self-management of HIV/ AIDS. For the poor patients in that region of Pakistan where access to the community doctors is not easy and medical facilities to care for HIV infected people are not available, support and guidance may be provided through telephone calls or the internet or frequent visits of health care officers to the community centers. It is recommended to implement a comprehensive HIV/AIDS programme addressing the needs of wider population, women and girls, children and orphans, young people, migrants and highly stigmatized populations such as sex workers, injecting drug users [16].
Structural intervention for effective HIV prevention
The social, economic, political, and environmental factors directly affect HIV risk and vulnerability and have stimulated interest in structural approaches to HIV prevention [17]. Efforts to address these factors are commonly referred to as structural approaches and seek to change the root causes or structures that affect individual risk and vulnerability to HIV [17,18].
In a male dominated society such as Pakistan or sub-continent, structural approach combined with other prevention strategies might be a better way to achieve effective HIV prevention. One of the patients mentioned that ….“Had my husband informed me before that he is HIV positive or used condoms after the marriage that might have saved me from HIV infection….”.
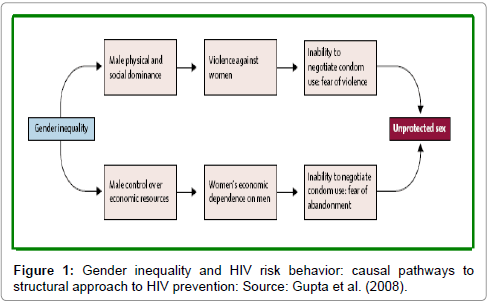
This statement points to the direction that taking a structural approach begins by understanding the causal pathways in order to identify the points of maximum effect for any given intervention as shown in Figure 1.
For example, if gender inequality manifests violence, stigma and discrimination against women, which in a local community results in women’s fear of retribution, it reduces their ability or willingness to negotiate condom use (Figure 1). This study case was in line with this risk behaviour and was a case of structural intervention at the time of her marriage. This causal pathway points to several potential areas to intervene such as involvement of some agencies promoting civil rights for women, upholding women’s property rights in cases of domestic violence, enforcing the law and order to declare HIV positive results to partners or prosecuting men who inflict violence on women [17]. Therefore, to implement structural approaches for prevention of HIV virus, the social, political, economic and environmental factors influencing both vulnerability and risk must be identified along with causal pathways between the structural factor and the behaviours that need to be changed [17,18].
Mitigating the impact of HIV/AIDS on societies and culture
It is important to understand how the virus is affecting communities and institutions, to learn to live with the virus and to mitigate its impact as much as possible. The education sector needs information about conditions which encourage the spread of HIV/AIDS and how best to educate those at risk. New and more robust evidence must inform HIV/ AIDS teaching and learning, particularly in life skills programmes. Children, their parents and communities need comprehensive health education aimed at preventing and controlling the spread of the disease among young people in and out of school. The national policy of Pakistan on HIV/AIDS for educators must protect the constitutional rights of all educators and learners [16]. The educators need more knowledge of, and skills to deal with, HIV/AIDS and should be trained to give guidance on HIV/AIDS and should be able to increase the awareness and changing behaviours to reduce stigma and discrimination associated with HIV infected people [19,20].
Recommendations to improve access to resources
The problem of access to resources in community settings has been addressed in many approaches which include the use of coaches to help individuals identify available resources for intervention strategies. Community-based groups may develop resources such as walking paths [20] or to redesign the communities to improve healthy behaviours and eventually the population health [21,22]. A systematic review of interventions to promote physical activity carried out by with the conclusion that improving access to places and opportunities for physical activity in communities and improving access to healthy foods were effective in promoting physical activity and healthy eating habits [23].
Environmental and community perspectives of HIV/AIDS
The social interaction between the patients and doctors is of great significance. The patients of HIV/AIDS need to engage with a range of health professionals. Gaining knowledge of the patient’s perspective builds on traditional models of physician-patient provides greater clarity to the range of lay understandings that should be explored as a component of effective risk communication [24]. In this case study it was a common concern of all the patients that: “In the absence of medical support facilities, adherence to antiretroviral regimens is difficult for them and for others with HIV virus……”
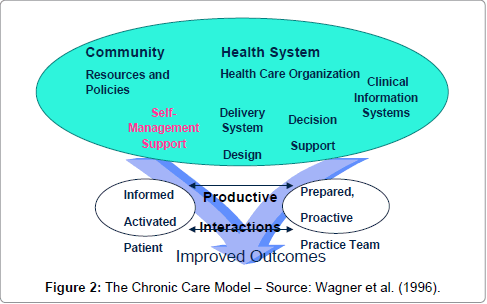
This statement is very well supported by framework for integrating the resources and supports for self-management with key components of clinical care was provided by in their Chronic Care Model shown in (Figure 2) [25]. There are six fundamental areas identified by the chronic care model making up a system that encourages high-quality chronic disease management. Organizations must focus on these six areas (self-management, decision support, delivery system design, clinical information system, organization of health care, community) as well as develop productive interactions between patients who take an active part in their care and providers backed up by resources and expertise [25]. The changes described here can be applied to a variety of chronic illnesses (in this case study to HIV/AIDS), health care settings, and target populations.
A number of studies have also suggested that patient understanding and beliefs about health and illness may be shaped by historical and local contexts whether respondents are thinking about health or behaviour in general or about their own and personal experience and observation [26-29].
HIV infection is a behavioural disease subject to environmental influence and therefore, effective HIV prevention and self-management not only comprises targeted interventions fostering changes in individual behaviour, but also interventions creating local environments conducive to, and supportive of, individual and community–level behaviour change. This requires a focus in bringing about changes in the physical, social, economic, legal and policy environments influencing HIV risk and HIV prevention [30,31]. These approaches have been variously termed as an ‘enabling environment’ approach to prevention and ‘structural HIV prevention’ [19,32].
Psychological Impacts of HIV/AIDS
A person diagnosed with HIV virus, may suffer from psychological trauma from knowing that recovery from the disease is not possible. Also, one of the most common causes for psychological trauma related to HIV/AIDS is the impact of social stigma on the infected individual. This stigma can lead to feelings of depression, guilt and shame, limited participation within communities [33]. The impact of stigma is particularly negative due to the common perception that the infected individual is to blame or should be held personally responsible for this condition [33]. In case of these patients, this problem was inflicted on them by their husbands who were HIV positive and did not inform these women before the marriage. During this interview, it was clearly mentioned by women patients that: “We think that individual who tests positive for HIV have obligation to notify his partner, it is our life which has been ruined by the social injustice and cultural norms.”
This statement is very important in the context of self-management of HIV/AIDS and the way lay people think about health and wellness influences their health and wellness related behaviours [34,35]. There is evidence of substantial research on psychological, cultural and social factors in individual’s “personal models of illness.” suggesting that the best practice for health education to begin with the perspective of the individual and that of the culture in which he or she was raised.
Barriers to HIV/AIDS Self-Management and Quality of Life
During interview it was emphasized many times that patients had difficulties accessing community doctors due to the absence of medical support facilities and the lack of information on HIV/AIDS among education providers and health workers in remote areas.
It was mentioned by the patients under this case study during the interview that: “There are a lot of people with HIV/AIDS who are reluctant to see the doctor because of the stigma attached to this disease in the society…….”.
In this case study, the barriers to HIV/AIDS are more specific to the local context and as such addressing the cultural norms and tradition of that society. The fact that Pakistan’s status has changed from ‘high risk low prevalence’ country to one that has concentrated epidemic, did not change the behaviour of the public as they still reluctant to accept the danger of a generalized epidemic [16]. Cultural, social and religious factors concerning the discussions of sexual behaviour have inhibited the public discussion of reproductive health and sexual behaviours.
The women patients in this case study are the victims of social and cultural norms of that society as they were deprived of the information that their husbands were HIV positive before the marriage and infected them as well. Now these women face the stigma attached to them carrying this disease, subject to isolation from society, lack of family support and discrimination in day to day life. The other barriers are the coverage of HIV prevention and control services among target populations especially high risk group remains low, the quality of care in counselling and treatment services remains an ongoing issue and seeing a male doctor by a female patient is out of the norm of the culture which poses great difficulties for HIV/AIDS patients to see a doctor particularly in remote areas where there is a keen shortage of medical practitioners.
Conclusion
It has been demonstrated in this case study that the women infected with HIV facing a complex array of medical, psychological, social and cultural challenges. In order to meet these challenges, socio-ecological approach to self-management of HIV/AIDS has been proposed reflecting the grounding of this disease in the context of social and environmental influences. Therefore, understanding selfmanagement of HIV/AIDS is the ultimate goal for the patients and that leads to an appreciation of the complementary nature of processes rooted at the individual level such as assessment, goal settings, learning skills and processes that are intrinsically social and based on families, organizations and communities. In order to improve the quality health care for HIV/AIDS in health clinics, it would require a multifactorial approach emphasizing patient education, improved training in behavioural change for providers, and enhanced delivery system.
The stigma associated with HIV/AIDS places a major burden on patients such as isolation, self-depreciation, and a lack of education, contributing to the negative psychological impact of HIV/AIDS on these patients living with HIV and the patients in this case study are the victim of that stigma as well, however, this stigma can be reduced if community and society work together towards improving the psychological conditions of all those infected and affected by HIV/ AIDS.
Finally, in a male dominated society such as Pakistan, it is important that HIV testing should be made compulsory by law for both the parties before marriage and that will eliminate the case of ‘victim blaming’ as in this case study where the women were not HIV positive before marriage. This case study has revealed only small number of women from the four provinces of Pakistan, but there may be a lot of women in that country who are suffering from the same cultural and traditional injustice where the demand of HIV test results before marriage are considered against the norms of the culture and are in conflict with the traditions of the families. Therefore, it is required to focus in bringing about changes in the physical, social, economic, and legal and policy environments influencing HIV risk and HIV prevention.
Acknowledgements
The authors extend thanks to the interviewees from all the provinces of Pakistan for their great cooperation and understanding during the course of the interviews to share their health related issues and difficulties facing with the selfmanagement of HIV/AIDS.
References
- National AIDS Control Programme (NAIDS-2006) UNGASS Indicators country report.
- Mahmud G, Abbas S (2009) Prevalence of HIV in pregnant women identified with a risk factor at a tertiary care hospital. J Ayub Med Coll Abbottabad 21: 124-127.
- Family Health Intervention (FIH-2005). National study of reproductive tract and sexually transmitted infections, mapping exercise of high risks groups in selected district of Punjab.
- Siegel K, Lekas HM (2002) AIDS as a chronic illness: psychosocial implications. AIDS 16 Suppl 4: S69-76.
- Bartlett JG, Cheever LW, Johnson MP (2004) Primary care as chronic care. In: Bartlett JG, Cheever LW, Johnson MP, A Guide to Primary Care for People HIV/AIDS.
- Lorig KR, Holman H (2003) Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med 26: 1-7.
- Gochman D S (1997) Handbook of Health Behaviour Research II, Plenum Press, NY.
- Sherbourne CD, Hays RD, Ordway L, DiMatteo MR, Kravitz RL (1992) Antecedents of adherence to medical recommendations: results from the Medical Outcomes Study. J Behav Med 15: 447-468.
- Roter DL, Hall JA, Merisca R, Nordstrom B, Cretin D, et al. (1998) Effectiveness of interventions to improve patient compliance: a meta-analysis. Med Care 36: 1138-1161.
- Kaplan RM, Toshima MT (1990) The functional effects of social relationships on chronic illness and disability. In Sarason, BS, Sarason, I.G and Pierce, G.R (eds). Social Support: An International View, Wiley, New York, pp: 427-453.
- Uchino BN, Cacioppo JT, Kiecolt-Glaser JK (1996) The relationship between social support and physiological processes: a review with emphasis on underlying mechanisms and implications for health. Psychol Bull 119: 488-531.
- Dignam JT, Barrera M Jr, West SG (1986) Occupational stress, social support, and burnout among correctional officers. Am J Community Psychol 14: 177-193.
- Cohen S, Doyle WJ, Skoner DP, Rabin BS, Gwaltney JM Jr (1997) Social ties and susceptibility to the common cold. JAMA 277: 1940-1944.
- Glasgow RE, Strycker LA, Toobert DJ, Eakin E (2000) A social-ecologic approach to assessing support for disease self-management: the Chronic Illness Resources Survey. J Behav Med 23: 559-583.
- House JS, Landis KR, Umberson D (1988) Social relationships and health. Science 241: 540-545.
- National AIDS Control Programme (NAIDS-2007) Progress report on the declaration of commitment on HIV/AIDS. Ministry of Health, Government of Pakistan, Islamabad.
- Gupta GR, Parkhurst JO, Ogden JA, Aggleton P, Mahal A (2008) Structural approaches to HIV prevention. Lancet 372: 764-775.
- Merson MH, O’Malley J, Serwadda D (2008) The history and challenge of HIV prevention. Lancet 372: 475-488.
- Sumartojo E (2000) Structural factors in HIV prevention: concepts, examples, and implications for research. AIDS 14 Suppl 1: S3-10.
- Brownson RC, Housemann RA, Brown DR, Jackson-Thompson J, King AC, et al. (2000) Promoting physical activity in rural communities: walking trail access, use, and effects. Am J Prev Med 18: 235-241.
- Frank, LD, Engelke, PO, Schmid, TL (2003) Health and Community Design: The Impact of the Built Environment on Physical Activity. Washington, DC: Island Press.
- Frumkin, H, Frank, L, Jackson, R (2004) Urban Sprawl and Public Health: Designing, Planning, and Building for Healthy Communities. Washington, DC: Island Press.
- Kahn EB, Ramsey LT, Brownson RC, Heath GW, Howze EH, et al. (2002) The effectiveness of interventions to increase physical activity. A systematic review. Am J Prev Med 22: 73-107.
- Holmström I, Rosenqvist U (2001) A change of the physicians' understanding of the encounter parallels competence development. Patient Educ Couns 42: 271-278.
- Wagner EH, Austin BT, Von Korff M (1996) Organizing care for patients with chronic illness. Milbank Q 74: 511-544.
- MacFarlane A, Kelleher C (2002) Concepts of illness causation and attitudes to health care among older people in the Republic of Ireland. Soc Sci Med 54: 1389-1400.
- Blaxter M (1990) Health and Lifestyles. London: Tavistock/Routledge.
- French DP, Senior V, Weinman J (2001) Causal attributions for heart disease: a systematic review. Psychol Health 16: 77-98.
- Davison C, Smith GD, Frankel S (1991). Lay epidemiology and the prevention paradox. Sociol Health Illness 13: 1-19.
- Rhodes, T (2002) The risk environment: a framework for understanding and reducing drug-related harm. International Journal of Drug Policy 13: 85-04.
- Singer M, Clair S (2003) Syndemics and public health: reconceptualizing disease in bio-social context. Med Anthropol Q 17: 423-441.
- Tawil O, Verster A, O'Reilly KR (1995) Enabling approaches for HIV/AIDS prevention: can we modify the environment and minimize the risk? AIDS 9: 1299-1306.
- Fife BL, Wright ER (2000) The dimensionality of stigma: a comparison of its impact on the self of persons with HIV/AIDS and cancer. J Health Soc Behav 41: 50-67.
- Hughner RS, Kleine SS (2004) Views of health in the lay sector: a compilation and review of how individuals think about health. Health (London) 8: 395-422.
- Inouye J, Flannelly L, Flannelly KJ (2001). The effectiveness of self-management training for individuals with HIV/AIDS. J Assn Nurse AIDS Care 12(5): 71-82.
Relevant Topics
- Child Health Education
- Construction Safety
- Dental Health Education
- Holistic Health Education
- Industrial Hygiene
- Nursing Health Education
- Occupational and Environmental Medicine
- Occupational Dermatitis
- Occupational Disorders
- Occupational Exposures
- Occupational Medicine
- Occupational Physical Therapy
- Occupational Rehabilitation
- Occupational Standards
- Occupational Therapist Practice
- Occupational Therapy
- Occupational Therapy Devices & Market Analysis
- Occupational Toxicology
- Oral Health Education
- Paediatric Occupational Therapy
- Perinatal Mental Health
- Pleural Mesothelioma
- Recreation Therapy
- Sensory Integration Therapy
- Workplace Safety & Stress
- Workplace Safety Culture
Recommended Journals
Article Tools
Article Usage
- Total views: 15516
- [From(publication date):
October-2013 - Dec 04, 2024] - Breakdown by view type
- HTML page views : 10992
- PDF downloads : 4524