Review Article Open Access
Social-Psychiatric Care for Dementia Patients in Vienna, Austri a
Stefan Strotzka*
Clinical Psychologist, Geronto-Psychiatric Center for Psycho-Social Services, Gumpendorferstr, Vienna, Austria
- Corresponding Author:
- Stefan Strotzka
Clinical Psychologist, Geronto-Psychiatric Center for Psycho-Social Services
Gumpendorferstr, Wien,Vienna, Austria
Tel: +43 14000 53090
E-mail: stefan.strotzka@psd-wien.at
Received date: February 20, 2015; Accepted date: May 13, 2015; Published date: May 20, 2015
Citation: Strotzka S (2015) Social-Psychiatric Care for Dementia Patients in Vienna, AustriaJ Alzheimers Dis Parkinsonism 5:190. doi:10.4172/2161-0460.1000190
Copyright: © 2015 Utkin YN, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Alzheimers Disease & Parkinsonism
Abstract
In 2001, the Geronto-Psychiatric Center for Psycho-Social Services opened in Vienna. Supported by the city, this ambulatory social-psychiatric institution undertook with its multi-professional team to enable those afflicted with dementia to achieve the longest possible life in the familiar surroundings of their own homes. The Center cooperates closely with the social bases of support of the city and with backing from nursing care providers. It gives advice on organizing home assistance, visiting services and placements in geriatric day centers and day clinics. Family members can get advice for relieving their burden and obtain information about dementia as a disease. During the first thirteen years, the Center examined and assisted more than 5,000 clients (approximately 30 % through home visits) with an average age of 80. The results of an extended study of more than 150 dementia patients who consulted the Center for four years demonstrate that the ambulatory and human assistance has been highly effective.
Keywords
Geronto-psychiatric center; Social-psychiatric care; Dementia
The grey horses are waiting
Two months after the Vienna Geronto-Psychiatric Center (Geronto- Psychiatrisches Zentrum, GPZ) opened in the Sechsschimmelgasse in November, 2001, an 80-year old client arrived for examination with her nephew. Her occupation had been that of a seamstress. She was a widow without children, her nephew her only remaining relation. Not long before her visit, her apartment had been broken into. In consequence, she was in a state of deep confusion. The nephew was exceedingly concerned about the wellbeing of his aunt. The neuro-psychological examination established that she suffered from moderately severe dementia. On the Mini Mental State Examination (MMSE) [1,2], she scored only 12 out of 30 possible points and she experienced great difficulties in drawing the clockface of the clock drawing test [3] (Figure 1).
She was a joyous, freedom-loving person with a good sense of humour. The team at the Center undertook to fulfill her wish to remain as long as possible in the familiar surroundings of her apartment. The client was prescribed anti-dementive therapy and invited to come to the center once a week, on Thursdays at 10 a.m., for memory training. Due to her advanced dementia, it was no longer possible for her to recall the day of the week. Fortunately, however, she had an amiable acquaintance who called her on Thursday mornings and reminded her with the words, the gray horses are waiting (referring to the name of our street, Sechsschimmelgasse, or Street of the Six Gray Horses). The Sechsschimmelgasse, located in the Ninth Urban District of Vienna, is a relatively steep avenue, which according to legend required six grey horses to pull wagons up its incline. Luckily, the client’s apartment was located in this district which was familiar to her from her earliest days and therefore firmly anchored in her oldest memory stratum. As a result, she found her way without difficulties. The journey, invariably on foot, took about 20 minutes. Upon arrival, she rejoiced upon seeing the members of the team.
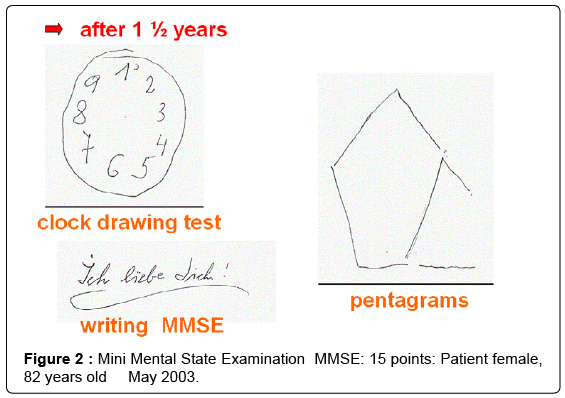
In this manner, the client was able to visit the Center on a regular basis every Thursday for an individually adjusted 45-minute memory training session; and at regular intervals she received an additional interview with the psychiatrist who treated her, thereby optimizing the anti-dementive therapy. Both her nephew and her sympathetic acquaintance who cared for her and charmingly reminded her of her Thursday appointments appeared often for consultations with dependents and were given support by phone with minor difficulties. After one and a half years a monitory examination registered a positive improvement on the MMSE from twelve to fifteen points (Figure 2).
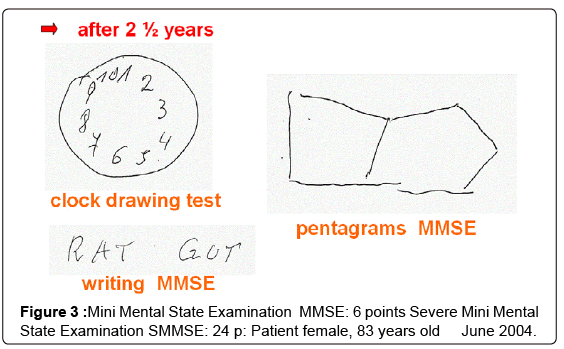
Two years after the initial contact the client was assaulted in the stairwell of her house by someone who had followed her in order to steal her purse. From then on, she no longer came for memory training. Instead, she received home visits and eventually in-home assistance and other mobile services. A monitory examination after two and half years resulted in a MMSE score of only six of thirty points, placing her in the range of severe dementia (Figure 3). In the meantime, her nice acquaintance had passed away. The nephew continued to attend to her needs, visiting her two or three times per week. A ninety-year old neighbour woman who was physically and mentally fit looked in on her every day. In this way, it was possible for a client in an advanced stage of dementia to continue living in her own apartment.
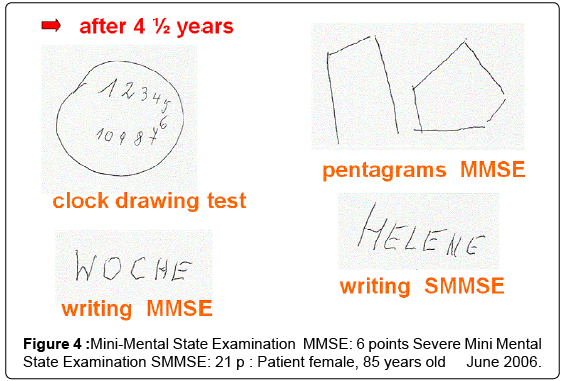
In June, 2006, four and a half years after the first visit in the Center, she came in to be examined for the last time. This time, too, she scored six points on the MMSE (Figure 4). Not until January, 2007, did the client move into a nursing home. From the time of her first visit, she had continued for five years in her familiar surroundings. She lived on in the nursing home for seven more years before dying in January, 2014, at the age of ninety-three.
In July 2012 the Center moved from Sechsschimmelgasse to Gumpendorferstraße in the Sixth Urban District of Vienna.
A Thirteen-Year Balance
The Geronto-Psychiatric Center exists as an ambulatory, socialpsychiatric institution of the Psycho-Social Services in Vienna [4,5]. Currently, the team consists of four women and five men from disciplines of psychiatry, psychology, social work and professional nursing. In total, they work 290 hours per week, which corresponds approximately to seven full-time employees. The referrals for the patients is borne chiefly by employees of the social support bases, nursing care providers, general practitioner physicians and specialists for psychiatry and neurology. In addition, there are referrals from the institutions of the Psycho-Social Services in Vienna and the city hospitals. Some patients are drawn to the Center due to word of mouth.
After the Center opened in September, 2001, for the first calendar year, 2002, only one percent of those examined had grown up in another country. Between 2010 and 2012 the share had already reached ten percent [6]. In the calendar years 2013 and 2014, a full eighteen percent of those who came to the GPZ were from 30 different countries. This equates roughly to the percentage of older foreign born in the Viennese population.
During the first thirteen years, nearly 5,000 clients (approximately thirty percent through home visits) were assisted, with an average age of almost eighty. Two thirds of these were suffering from dementia. In twenty percent of the cases, mild cognitive impairment (MCI) was diagnosed with probable development of dementia. The MCI-patients were typically summoned by phone or letter for a neuropsychological examination within six months of their initial visit. In general, however, the examinations were annual. There occurred 1,200 initial examinations, 650 second ones, 395 third, 220 fourth, 150 fifth, 100 sixth, 60 seventh, 40 eighth, 20 ninth, ten tenth, and five eleventh ones. Counting initial visits, five patients tallied up a full twelve visits. Among the 2,850 examinations, approximately fifty percent of those examined were constant in cognitive performance. Roughly forty percent became worse; and around ten percent actually improved. Considering that one third of the patients were suffering from moderate to severe dementia and their average age was eighty, it is remarkable that no more than five percent of the patients had to be resettled into nursing homes after one year.
Altogether in the first thirteen years more than 6,000 neuropsychological examinations were carried out, of which roughly 55 % were initial exams and 45 % follow up control exams. It is evident from this that a high priority is placed on regular follow up exams in the GPZ. The tests take place in a good and relaxed atmosphere in an amicably furnished space. The majority of clients find the experience pleasant [7].
Extended Retrospective Study
For the extended retrospective study numerical results for 150 individuals were evaluated. All clients who came for four years to the center with a diagnosis of Alzheimer’s dementia were included in the study.
The investigation of the 150 patients suffering from dementia revealed between the initial examination and the fourth control visit an average worsening on the MMSE Test on 23.8 to 19.8 points, thus a reduction of only four points after four years (Table 1). Clinical studies show that without treatment a worsening of on the average between 3-4 in a single year can be expected on the MMSE [8-11]. This means that after four years the patients on average worsened only to the degree that one would have expected after a single year. To the degree that we can point to something like a control group, its function is represented by this average worsening without treatment; however, on ethical grounds, we would not have been permitted to withhold treatment to constitute a control group.
| First Examination | Fourth Examination | |
|---|---|---|
| Age | 77 y. | 81 y. |
| MMSE | 23,8 | 19,8 |
| Anti-dementive therapy | 10% | 96% |
| Receiving care-giving subsidy | 26% | 67% |
Table 1: Extended retrospective study for four years with 150 dementia patients.
The author of this article is aware of being part of the institution described and therefore not an external observer. Nonetheless, in evaluating the work of the center, he has attempted to adhere to strict criteria as conscientiously as possible. Although the center was not in a position to withhold treatment in order to constitute a control group, there were nonetheless patients who for various reasons did not return for treatment in the course of four years and who therefore did not receive the social-psychiatric treatment. In that group a worsening of 11-12 points was often observed. Although these are isolated cases, they also suggest that with a rigorously organized control group from which treatment were withheld, an unequivocal worsening might well have been the experimental result.
What sort of individuals are found in this group and how can such a favourable result be explained? The average age of the patients of whom 65 % were women and 35 % men came to 81 years as of the fourth follow up examination. Of these, roughly half were, from first being tested to the fourth follow up, in a mild state of dementia. Eleven percent remained in moderately severe for the four years; a third worsened from mild to moderately severe; and eight percent from moderately severe to severe.
Nearly half (42 %) lived alone in an apartment; 49 % with a spouse; six with a child or grandchild. Five individuals resided in assistedliving units. About half had two to four children; a third one child; and only sixteen percent were childless. In many cases, an extensive labour of care giving is performed by the spouse and children. Prior to visiting the Center, only 26 % of the clients were evaluated to receive a care-giving subsidy; afterward, 67 % received financial support in the form of the same subsidy. Only 15 of the 150 dementia patients had received an anti-dementive therapy as of the initial examination; after the medical examination in the Center 96 % were treated with modern anti-dementive medications. Twenty-four patients were treated with the combination therapy (acetylcholine-esterase inhibitors plus memantine).
The 150 individuals studied each visited the GPZ in the four years an average of ten times, with a minimum of 5 and a maximum of 95 times. The phone calls with subjects averaged 24, with a minimum of six and a maximum of 115: more than double the number of ambulatory visits. For thirteen patients, a total of 27 house visits took place. There is no single exhaustive explanation for the relatively favourable results with this group after its four years of care; but we can assume that their success was effected by a good mixture of anti-dementive therapy, intensive counselling of carers, social contacts, and the memory training conducted at the Center.
Résumé
Together with his colleagues at the Center, the author participates in practical work on behalf of patients and pursues the objective of making the knowledge acquired in their work available to a broader public. He has presented the latest findings of dementia research and the practical work of the GPZ Vienna at conferences and professional development meetings. His paper on the quick clock test (Schneller Uhren-Dreier) [3], a modification of the Mini-Cog [12], has since become a widely used screening test for dementia in Austria [13]. The Severe Mini Mental State Examination [14], a test for the advanced stage of dementia, has been translated from the author for use in Germanspeaking countries [15]. It is hoped that this article may contribute to the introduction of badly needed social-psychiatrically oriented geronto-psychiatric centers in other cities.
Acknowledgements
The author would like to thank Andrew Weeks for the translation and Asita Sepandj for reading the manuscript.
References
- Folstein MF, Folstein SE, Mc Hugh PR (1975) Mini-Mental State – A Practical Method for Grading the Cognitive State of Patients for the Clinician. J Psychiatr Res 12: 189-198
- Strotzka S (2004) 30 Jahre Mini-Mental State Examination – Eine kritische Würdigung. Psychopraxis 05/04: 24-34.
- Strotzka S, Psota G, Sepandj A (2003) Uhrentest in der Demenzdiagnostik – Auf der Suche nach der verlorenen Zeit. Psychopraxis 04/03: 16-24
- Strotzka S, Psota G, Sepandj A (2004) Das Gerontopsychiatrische Zentrum (GPZ) des PSD Wien. Neuropsychiatrie 18(S1): 45-50
- Strotzka S, Sepandj A, Psota G (2009) Die Schimmel warten schon…“ – Acht Jahre Geronto Psychiatrisches Zentrum des PSD Wien. Gemeindenahe Psychiatrie 03/09: 169-175.
- Strotzka S (2015) Kognitives Assessment für Migrantinnen und Migranten. Z Gerontol Geriat 48: 10-14
- Auer S, Strotzka S, Weber S (2008) Leistungstestung von Menschen mit Demenz. Psychopraxis 02/08: 16-21.
- Schneider LS (2001) Cornerstones in the Management of Alzheimer´s disease, 15 Supplement 1: 8-18.
- Förstl H (2001) Demenzen in Theorie und Praxis. Berlin, Heidelberg, New York: Springer.
- Ivemeyer D, Zerfaß, R (2002) Demenztests in der Praxis. EinWegweiser. München: Urban & Fischer.
- Wächtler C (2003) Demenzen. Frühzeitigerkennen, aktivbehandeln, Betroffene und Angehörigeeffektivunterstützen. Stuttgart: Georg Thieme
- Scanlan J, Borson S (2001) The Mini-Cog: receiver operating characteristics with expert and naïve raters. Int J Geriatr Psychiatry 16: 216-222
- Kamenski G, Dorner T, Lawrence K et al (2009) Detection of dementia in primary care: comparison of the original and a modified Mini-Cog Assessment with the Mini-Mental State Examination. Ment Health Fam Med 6: 209-217.
- Harrell LE, Marson D, Chatterjee A et al (2000) The Severe Mini-Mental State Examination: a new neuropsychologic instrument for bedside assessment of severely impaired patients with Alzheimer disease. Alz Dis Assoc Dis 14(3): 168-175
- Strotzka S, Sepandj A, Psota G (2005) Severe Mini Mental State Examination – Neuropsychologie für schwer demente Menschen. Psychopraxis 06/05: 10-15
Relevant Topics
- Advanced Parkinson Treatment
- Advances in Alzheimers Therapy
- Alzheimers Medicine
- Alzheimers Products & Market Analysis
- Alzheimers Symptoms
- Degenerative Disorders
- Diagnostic Alzheimer
- Parkinson
- Parkinsonism Diagnosis
- Parkinsonism Gene Therapy
- Parkinsonism Stages and Treatment
- Stem cell Treatment Parkinson
Recommended Journals
Article Tools
Article Usage
- Total views: 15896
- [From(publication date):
September-2015 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 11351
- PDF downloads : 4545