Review Article Open Access
Small Things That Make a Big Difference
Pooja Kapoor*
Gian Sagar Dental College and Hospital, India
- Corresponding Author:
- Dr. Pooja Kapoor
Reader, Department of Orthodontics and Dentofacial Orthopaedics
Gian Sagar Dental College and Hospital, Ram Nagar, India
Tel: +91-9501093618
E-mail: pkaps82@gmail.com
Received date May 23, 2014; Accepted date September 11, 2014; Published date September 17, 2014
Citation: Kapoor P. (2014) Small Things That Make a Big Difference. J Interdiscipl Med Dent Sci 2:150. doi:10.4172/2376-032X.1000150
Copyright: © 2014 Kapoor P. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at JBR Journal of Interdisciplinary Medicine and Dental Science
Abstract
Goal directed orthodontic treatment is extremely important. If the goals of treatment are overlooked from the
diagnosis and treatment planning phase through to the phase of retention, continuous errors can be made. However, if the goals are kept constantly in mind, results are much more consistent, and when minor compromises must occur, the reasons for these can be understood to avoid many of them in the future. Therefore, the emphasis of this article is well summarized by the famous proverb “An ounce of prevention is better than pounds of cure”.
Keywords
Loading; Prevention; Orthodontics; Brackets; Archwires.
Introduction
Clinical efficiency or the lack thereof, dictates most of our management challenges. The paradox is getting a high quality finish in a reasonable number of appointments. Obviously, the more appointments it takes to treat each case, the more our workday is jammed. The term ‘loading’ is often used to characterize this phenomenon of any unnecessary or unplanned protocol that adds time to an appointment or adds an additional appointment to finish a case. But it’s the compounding effect that is devastating. When we load just a few visits per case, it adds thousands of appointments to our schedule each year.
We frequently talk about how much emergencies (like a wire sticking out in the cheek or a broken bracket) load the schedule, but the real menace are dozens of little steps that doctors take each day that are never thought of as extra. Oftentimes these additional steps are a result of things we don’t do early in treatment that cost us a lot of time later. Few important points usually overlooked are discussed ahead.
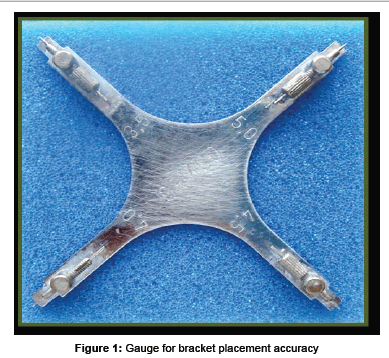
Accuracy in bracket placement
There is no other aspect more critical to a quality finish than the initial placement of brackets. We only get one chance at tooth preparation and bracket placement and this can be considered to be the most important doctor time spent in treatment as those extra few minutes per case pay big dividends. Inaccuracy at this stage will prevent the expression of the built in features of the bracket or wire. (Figure 1 shows Bracket placement gauge [1] that helps in accuracy)
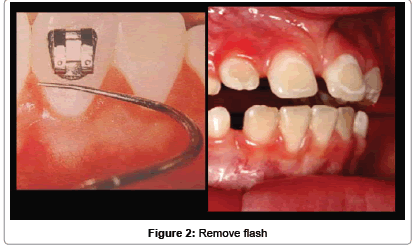
Removing flash to avoid white spots
One often encounters patients after completion of the treatment seeking help for the white spots on teeth once the orthodontic brackets have been removed with the affected teeth appearing as if they have small ‘bull's eyes’ on them. More often than not, it is then that we realize how easy it would have been to remove the excess flash [2] (Figure 2) than to subsequently do a cosmetic touch up on teeth again leading to the loading of our schedule. White spot lesions, the earliest visible stage of cavity formation, develop in association with brackets when excess flash is not taken care of at the initial bonding appointment to complicate conventional oral hygiene measures, leading to prolonged plaque accumulation.
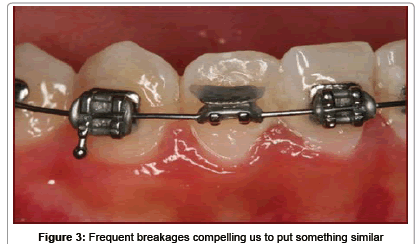
Exact bracket specifications or “something similar”
Brackets often debond due to failures with the bonding materials, traumatic occlusion, etc. and loading in a practice may generally not allow us to recycle a bracket immediately. Sometimes, a non compliant patient turns up to demand a replacement for a lost bracket! It goes without saying that what an orthodontic specialist dreads the most is ‘broken bracket syndrome’ (Figure 3) as it requires a new bracket adding to the cost of inventory and sometimes when we are out of it, we generally tend to look for a “something similar” to the original bracket. Later, it takes a lot more time and precision in wire bending to achieve the desired tip and torque required leading to loss in balance of biomechanics and frustration for both the clinician and the patient.
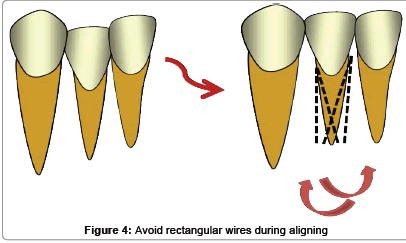
Avoiding rectangular wires during alignment to prevent round tripping
During stage one of treatment, mesio distal and labiolingual tipping guided by an archwire is needed, but root movement usually is not, as root apices are reasonably close to their correct positions even though crowns have been displaced as the teeth erupted. The corollary is that although a highly resilient rectangular arch wire such as 17 x 25” NiTi once deemed as magic wires could be used in the alignment stage, this is not advantageous because rectangular wire will create unnecessary and undesirable root movement [3] (Figure 4) causing more damage and round tripping identified as a radiographic havoc evident later on.
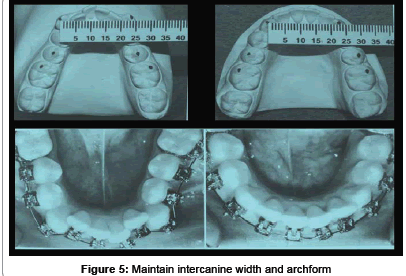
Maintain intercanine width
This is the most critical part of an archform [4] since significant relapse occurs if this dimension is changed. Upper and lower intercanine width [5] should be kept as close as possible (Figure 5) to starting dimensions for stability taking care that crowding is not relieved at the expense of uncontrolled expansion of the arches.
Maintain arch form
When teeth are engaged into an archwire, it is important to recognize that the plane of occlusion must not be altered erroneously. Maintenance of archform [4] (Figure 5) leads to stability at the end of treatment and prevents round tripping many a times by attaining equilibrium at all points due to balancing forces of the tongue and circum oral tissues.
Small upper second premolar
Upper second premolars are sometimes small [6] in daily practice as compared to other teeth. Therefore additional first order in out bending, or, an alternative bracket that is 0.5mm thicker than normal can be used to achieve proper contact and marginal ridge relationship with adjacent teeth (Figure 6).
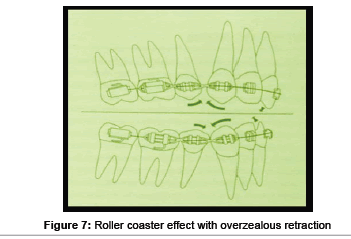
Roller coaster effect with overzealous retraction
This is generally seen during leveling and aligning stages or when we overenthusiastically retract teeth on flexible archwires. More time is later spent to rectify the roller coaster [7] effect (Figure 7) than that spent in using the optimum forces and keeping the biomechanics of the system accurate. Stainless steel wires and NiTi wires look the same and sometimes we may mistake a NiTi for a Stainless Steel and start retracting, so to avoid this problem we must always fill in the notes in our case history notebook which can be referred to in the next appointment.
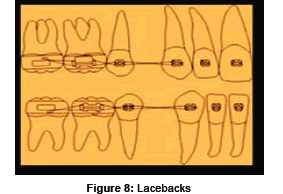
Lacebacks
Lacebacks [8] are indicated routinely to assist the control of canine crowns in pre molar extraction cases and some non-extraction cases (Figure 8). They help in anchorage control in the early stages of treatment where the main threat comes from influence of anterior bracket tip. Failure to use lacebacks can be an obstacle in achieving ideal result in many cases.
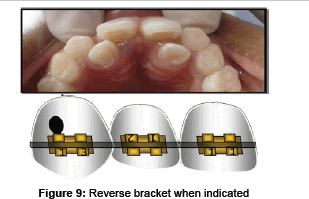
Reverse bracket when indicated
Sometimes, like in palatally placed lateral incisors (Figure 9), the brackets have to be reversed [9], to change the torque values from positive to negative to achieve root movements. This saves valuable treatment time at the end for torquing.
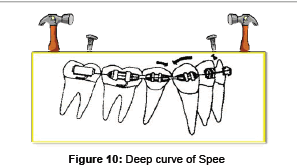
Deep curve of spee
Correction of Curve of Spee [10] is important, else, it will lead to space in the extraction areas (Figure 10) that is unsightly, and persistence to level the curve at the finishing stages will unnecessarily cause disappointment.
Follow specific biomechanics
Certain appliances require specific biomechanics and reactivation protocols. For example, KSIR [11] (Figure 11) arch for simultaneous intrusion and retraction need not be reactivated before 6-7 weeks.
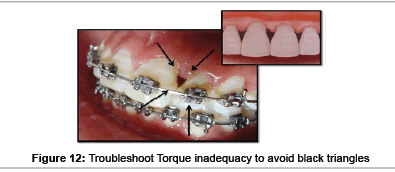
Troubleshooting torque inadequacy to avoid black triangles
Inconsistent, unpredictable, inaccurate and irreproducible actual torque forces lead to numerous clinical problems including extended treatment time with incisors tipping lingually (Figure 12) instead of maintaining their antero-posterior positions, under force systems designed to protract the posterior teeth. Invariably, this leads to loss of alveolar bone and recession of the gingival papillae leading to unsightly black triangles in the area.
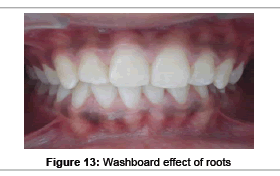
Washboard effect
This is usually seen in lower anterior teeth. Overenthusiastic aim at proclining these teeth to reduce overjet can lead to the so called washboard effect and resultant bone loss or root resorption as teeth touch cortical bone (Figure 13).
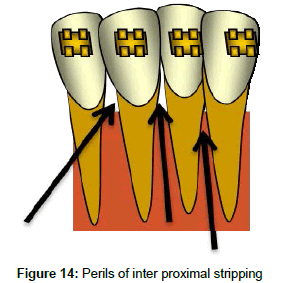
Perils of inter proximal stripping
If the roots of adjacent teeth are too close as is usually the case in lower anterior teeth (Figure 14), interproximal stripping should be avoided, as it will lead to quick bone loss and papilla recession causing long clinical crowns and triangular spaces apart from sensitivity on exposed cementum.
Residual growth status
Residual growth status must always be considered before planning orthognathic surgeries [12], else, relapse is unavoidable after a spurt suddenly leads to the same deformity. Also, it can be very frustrating if growth modulation techniques yield no fruit if the spurt we need to take advantage of has already surpassed.
CSF (Circumferential Supracrestal Fiberotomy)
Rotated teeth are part of the most common malocclusions and permanent retentions which depend on patient compliance are not the ultimate solution for the same. However, CSF [13] can take care of the same to a large extent (Figure 15).
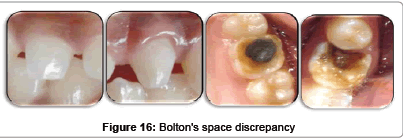
Bolton’s space discrepancy
Antero posterior problems at the end of the treatment can invariably occur as a result of failure to calculate the Bolton’s discrepancy [14] at the time of treatment planning. Decreased overjet can be due to lower anterior tooth material excess, or due to upper anterior tooth material deficiency and vice versa (Figure 16).
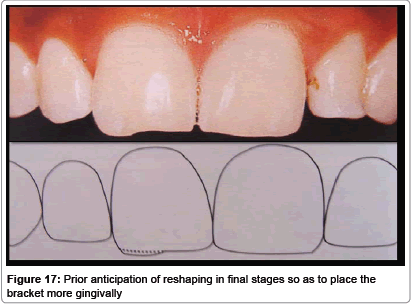
Tooth morphology
Shape of the crowns, especially incisors, needs to be assessed during finishing and settling. Triangular or barrel shaped teeth, for example can be reshaped [15] in final stages, but, the challenge is to calculate accurately space discrepancies when artificial crowns are an indication during orthodontic treatment or prior to that because of loss of tooth structure. Prior anticipation of reshaping incisal edges later (Figure 17) can guide us to place bracket more gingivally at the very first appointment.
Patient compliance
Patient compliance before, during and after treatment in the retention phase are all equally important for success. A non compliant and non motivated patient will rarely comprehend the protocols to be followed for maintenance of oral hygiene, wearing of elastics, keeping the appointments, breakage of appliance, etc.
Summary and Conclusion
Nearly all the practices are seeing many more patients per day than is necessary. Once the cycle begins, it is exacerbated of its own accord. When we are crazily seeing patients in a rushed manner, we often can’t do everything planned for that day, so we appoint them to return in 2 to 3 weeks. This further jams the schedule and the snowball effect begins. Additional appointments require more staff, more space and result in more stress. They require more practice days and drive our receptionists nuts trying to figure out a schedule that works. Everybody suffers the consequences, including the patient and our chance of producing a beautifully finished case diminishes significantly. Life is all about decreasing stress and if we want to grow our practice, we can use the time we’ve gained through ‘unloading’ to start more patients within the existing time. So, it is not for nothing that this article reinforces the motto “A stitch in time saves nine” to obtain the necessary potpourri of finishing pearls.
References
- Bennett JC, McLaughlin RP (2001) Orthodontic management of the dentition with the preadjusted appliance, Mosby. St Louis, USA.
- McNamara J, Brudon WL (2001) Orthodontics and Dentofacial Orthopedics.Needham Press.Ann Arbor, USA.
- Proffit WR, Fields HW, Sarver DM (2007) Contemporary Orthodontics. (4thedn), Mosby, St Louis, USA.
- Henrikson J, Persson M, Thilander B (2001) Long-term stability of dental arch form in normal occlusion from 13 to 31 years of age. Eur J Orthod 23:51-61.
- Burke SP, Silveira AM, Goldsmith LJ, Yancey JM, Van Stewart A, Scarfe WC (1998) A meta-analysis of mandibular intercanine width in treatment and postretention. Angle Orthod. 68:53-60.
- McLaughlin RP, Bennett JC, Trevisi HJ (2001)Systemized orthodontic treatment mechanics.(1stedn), Mosby, St Louis, USA: 352.
- McLaughlin RP, Bennett JC, Trevisi HJ (2001) Systemized orthodontic treatment mechanics. (1stedn), Mosby, St Louis, USA: 98,137.
- McLaughlin RP, Bennett JC, Trevisi HJ (2001) Systemized orthodontic treatment mechanics. (1stedn), Mosby, St Louis, USA: 100-101.
- McLaughlin RP, Bennett JC, Trevisi HJ (2001) Systemized orthodontic treatment mechanics. (1stedn), Mosby, St Louis, USA: 41.
- McLaughlin RP, Bennett JC, Trevisi HJ (2001) Systemized orthodontic treatment mechanics. (1stedn), Mosby, St Louis, USA: 131,288.
- Kalra V (1998) Simultaneous intrusion and retraction of the anterior teeth. J. Clin. Orthod 32: 535-540.
- Bell WH, Proffit WR, White RP. Surgical correction of dentofacial deformities. W.B. Saunders Co, Orlando, USA.
- Proffit WR, Fields HW, Sarver DM (2007) Contemporary Orthodontics. (4thedn), Mosby, St Louis, USA: 615.
- Bolton WA (1962)The clinical application of a tooth size analysis. Am J Orthod48:504-529.
- McLaughlin RP, Bennett JC, Trevisi HJ (2001) Systemized orthodontic treatment mechanics. (1stedn), Mosby, St Louis, USA: 64.
Relevant Topics
- Cementogenesis
- Coronal Fractures
- Dental Debonding
- Dental Fear
- Dental Implant
- Dental Malocclusion
- Dental Pulp Capping
- Dental Radiography
- Dental Science
- Dental Surgery
- Dental Trauma
- Dentistry
- Emergency Dental Care
- Forensic Dentistry
- Laser Dentistry
- Leukoplakia
- Occlusion
- Oral Cancer
- Oral Precancer
- Osseointegration
- Pulpotomy
- Tooth Replantation
Recommended Journals
Article Tools
Article Usage
- Total views: 17994
- [From(publication date):
December-2014 - Apr 11, 2025] - Breakdown by view type
- HTML page views : 13274
- PDF downloads : 4720