Case Report Open Access
Sleep apnea in Chiari I malformation
Maher Abouda1*, Ferdaous Yangui2, Senda Turki2, Mehdi Charfi2
1University of Tunis El-Manar, Faculty of Medicine of Tunis, Respiratory and Sleep Medicine, FMT Bab Saadoun, TN 1004, Tunis, Tunisia
2University of Tunis El-Manar, Faculty of Medicine of Tunis, Interior Security Forces Teaching Hospital. FMT Bab Saadoun, TN 1004, Tunis, Tunisia
- Corresponding Author:
- Maher Abouda
University of Tunis El-Manar, Faculty of Medicine of Tunis
Respiratory and Sleep Medicine, FMT Bab Saadoun, TN 1004,Tunis, Tunisia
E-mail: maherabouda@yahoo.fr
Visit for more related articles at International Journal of Emergency Mental Health and Human Resilience
Abstract
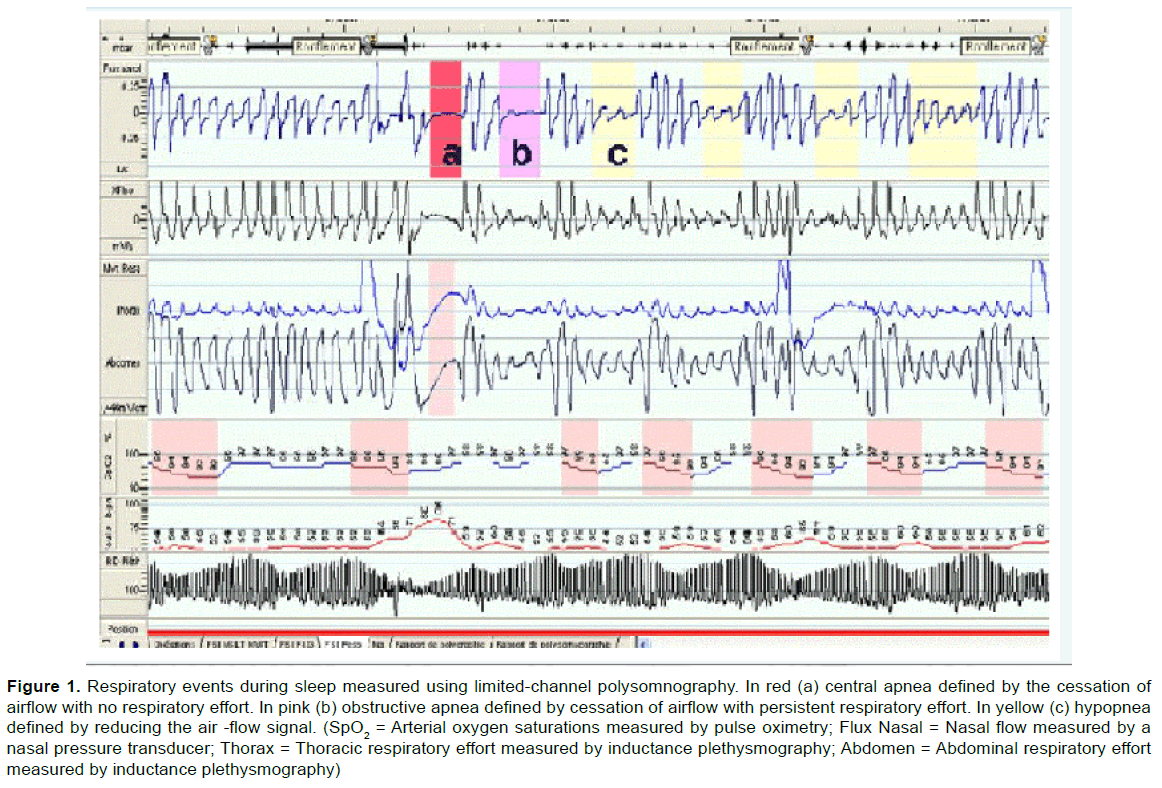
A 36-year-old non-obese woman consulted her physician for recent excessive daytime sleepiness (EDS) with Epworth sleepiness scale (ESS) at 13/24, morning headache and heavy snoring. Polysomnography revealed moderate mixed sleep apnea syndrome with an Apnoea–Hypopnoea Index (AHI) of 23/h (Figure 1). Despite adequate continuous positive airway pressure (CPAP) therapy, the patient reported an aggravation of EDS and headache. A second polysomnography with CPAP, conclude to moderate complex sleep apnea syndrome by revealing the persistence of numerous central sleep apnea (AHI of 21/h) but no evidence of obstructive events. The patient reported a sensation of unrefreshing sleep and EDS (ESS at 17/24) with no symptoms suggesting cardiac failure, periodic limb movement disorder or narcolepsy. Physical examination, including neurologic and cardiac examinations, was normal. Routine blood tests, arterial blood gas analysis and echocardiography were performed and showed no significant abnormalities.
Keywords
Sleep apnea, Chiari malformation
Case Report
A 36-year-old non-obese woman consulted her physician for recent excessive daytime sleepiness (EDS) with Epworth sleepiness scale (ESS) at 13/24, morning headache and heavy snoring. Polysomnography revealed moderate mixed sleep apnea syndrome with an Apnoea–Hypopnoea Index (AHI) of 23/h (Figure 1). Despite adequate continuous positive airway pressure (CPAP) therapy, the patient reported an aggravation of EDS and headache. A second polysomnography with CPAP, conclude to moderate complex sleep apnea syndrome by revealing the persistence of numerous central sleep apnea (AHI of 21/h) but no evidence of obstructive events. The patient reported a sensation of unrefreshing sleep and EDS (ESS at 17/24) with no symptoms suggesting cardiac failure, periodic limb movement disorder or narcolepsy. Physical examination, including neurologic and cardiac examinations, was normal. Routine blood tests, arterial blood gas analysis and echocardiography were performed and showed no significant abnormalities.
Figure 1: Respiratory events during sleep measured using limited-channel polysomnography. In red (a) central apnea defined by the cessation of airflow with no respiratory effort. In pink (b) obstructive apnea defined by cessation of airflow with persistent respiratory effort. In yellow (c) hypopnea defined by reducing the air -flow signal. (SpO2 = Arterial oxygen saturations measured by pulse oximetry; Flux Nasal = Nasal flow measured by a nasal pressure transducer; Thorax = Thoracic respiratory effort measured by inductance plethysmography; Abdomen = Abdominal respiratory effort measured by inductance plethysmography)
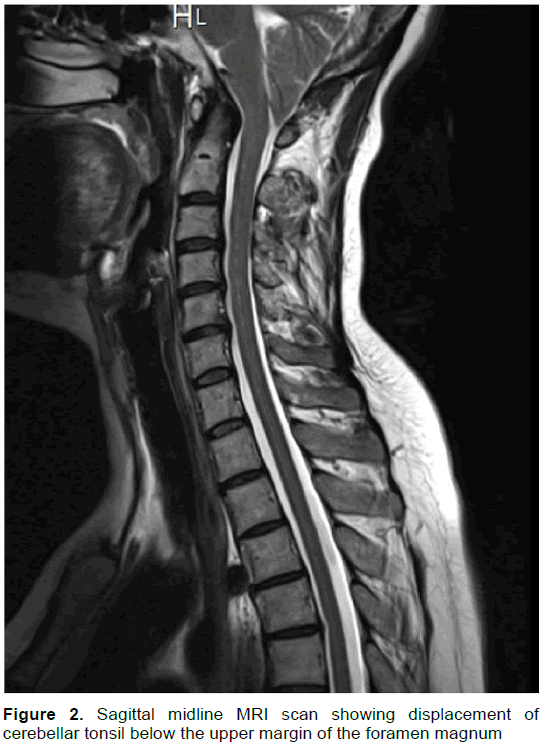
A cerebral MRI confirmed a type I Chiari malformation (CM) by showing displacement of cerebellar tonsil below the upper margin of the foramen magnum (Figure 2). The headaches were first treated with analgesics without success. Suboccipital craniotomy with upper cervical laminectomy was performed leading to improvement in symptoms. Three months later, polysomnography showed a persistence of mild apnea hypopnea syndrome.
CM defined by the presence of a part of the cerebellum below the foramen magnum, is a congenital disease with five subtypes among which type I is the most common. CM-I is usually discovered during the second or third decade of life either in asymptomatic patients or in patients presenting nervous system symptoms such as headache, fatigue, neck pain, lower cranial nerve signs or spinal cord disturbances. Different types of sleep apnea can be observed in patients with CM-I (Zolty, Sanders, & Pollack, 2000). Depression of the respiratory center by compression of the brain stream and abnormal chemosensitivity, are the potential mechanisms of central apnea in such patients. However, obstructive apnea can be due to alteration in upper airway patency during sleep related to abnormalities in Hypoglossal nerve activity (Roberta, & Leu, 2015). Complex sleep apnea defined by the emergence of repeated central apneas despite CPAP treatment, is probably related in patient with CM to altered chemo-reflexes (Losurdo et al., 2013).
References
- Losurdo, A., Dittoni, S., Testani, E., Di Blasi, C., Scarano, E., Mariotti, P., et al. (2013).Sleep disordered breathing in children and adolescents with Chiari malformation type I. Journal of Clinical Sleep Medicine: JCSM: Official Publication of the American Academy of Sleep Medicine, 9(4), 371–377.
- Roberta, M., &Leu, MD.(2015). Sleep-related breathing disorders and the Chiari 1 malformation.Chest, 148 (5), 1346-1352.
- Zolty, P., Sanders, M. H., & Pollack, I. F. (2000).Chiari malformation and sleep-disordered breathing: a review of diagnostic and management issues. Sleep, 23(5), 637–643.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 11813
- [From(publication date):
December-2016 - Apr 06, 2025] - Breakdown by view type
- HTML page views : 10884
- PDF downloads : 929