Short Communication Open Access
Skin ultrastructural similarities between Fibromyalgia and Ehlers-Danlos syndrome hypermobility type
Hermanns-Lê T1* and Pierard GE21Unit of electron microscopy, Department of Pathology, Unilab LG, University Hospital, Liège, Belgium
2Laboratory of Skin Bioengineering and Imaging (LABIC), Department of Clinical Sciences, Liège University, Belgium
- *Corresponding Author:
- Pierard GE
Laboratory of Skin Bioengineering and Imaging (LABIC)
Department of Clinical Sciences
Liège University, Belgium
Email: gerald.pierard@ulg.ac.be
Received date: December 04, 2015; Accepted date: December 15, 2015; Published date: January 27, 2016
Citation: Hermanns-Le T and Pierard GE (2016) Skin Ultrastructural similarities between Fibromyalgia and Ehlers-Danlos Syndrome Hypermobility Type. J Ost Arth 1:104. doi: 10.4172/joas.1000104
Copyright: © 2016 Hermanns-Lê T. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Osteoarthritis
Abstract
Fibromyalgia (FM) and hypermobility type Ehlers-Danlos syndrome (EDSH) share a series of common clinical signs. A clinical distinction between both diseases is occasionally difficult to be established. The physical changes observed in the mechanical properties of skin and joints do not distinctly distinguish these disorders. In addition, similar ultrastructural dermal changes are observed in both EDSH and some FM cases. The molecular alterations remain largely undisclosed in both diseases. As a result, EDSH remains undiagnosed in some FM patients. This condition deteriorates quality of life and possibly leads to prominent health problems.
Keywords
Fibromyalgia; Ehlers-Danlos syndrome hypermobility type; Skin ultrastructure; Joint hypermobility syndrome; Connective tissue disorder.
Introduction
Ehlers-Danlos syndrome (EDS) represents a conglomeration of distinct inherited genetic alterations in the molecular composition of the connective tissue extracellular matrix. Currently, six major types are recognized. Fibrillar collagen types are involved in the majority of EDS cases. The dermis, particularly its reticular layer is conveniently used for typing the molecular and ultrastructural EDS alterations [1]. Fibromyalgia (FM) is commonly evoked by widespread chronic musculoskeletal pain, tenderness and reactive joint, tendon and muscle stiffness, chronic fatigue, sleep disturbances and cognitive symptoms. Widespread pain is present at least for 3 months, on both sides of the body, both above and below the waist. The FM origin remains unknown. The diagnosis is assessed by rating the widespread pain index (WPI) endorsing 19 body regions, and a symptom severity score (SSS) based on the evaluation of fatigue, sleep disturbances and cognitive symptoms [2–5]. The combination with tender point refines the establishment of the FM diagnosis [5]. FM is frequently associated with joint laxity [6–14] representing a major diagnostic criterion of benign joint hypermobility syndrome (JSH) [15] and of the autosomal dominant hypermobility type Ehlers-Danlos syndrome (EDSH) [16–18]. In addition, several other common signs exist between FM and EDSH, including widespread pain, fatigue, anxiety, and functional gastrointestinal disorders [16]. From that observation, some FM presentations possibly represent an undiagnosed EDSH [19,20]. The genetic mutations are largely undisclosed in EDSH, but ultrastructural dermal abnormalities, although individually unspecific, appear relevant and contribute to the diagnosis drawing-up [1,18,21]. Globally, FM, EDSH and JHS represent three overlapping connective tissue disorders characterized by chronic and recurrent pain, joint instability and minor skin changes. The molecular defects remain unknown.
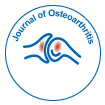
The dermal extracellular matrix is mainly composed of collagen and elastic fibres admixed with amorphous glycoproteins and glycosamimoglycans covalently linked to polypeptides to form proteoglycans. Collagen fibrils represent by far the most abundant component of the dermis. In normal subjects, they are present as a finely woven meshwork. They are united into thick interlacing and interconnected bundles in the reticulum dermis. In some connective tissue disorders, the aspect and the cut surface of the collagen fibrils are heterogeneous. These changes are best appreciated by combining electron microscopy and computerized image analysis [22-26]. Three main changes are possibly combined. First, wide variations are occasionally disclosed in the diameter of rounded fibrils. Second, large collagen fibrils with cauliflower shape and smaller serrated fibrils are present. Third, the interfibrillar spacing is irregularly enlarged. The EDSH diagnosis is tricky in absence of specific clinical clues and molecular mutation. Hence, its frequency is probably underestimated [20], and some FM possibly represents an undiagnosed EDSH. In our experience, at least about 15 % of FM patients show EDSH signs.
We presently compare ultrastructural aspects of the skin in FM and EDSH, searching for objective diagnostic criteria. We revisit the ultrastructural aspects of the dermis in FM and EDSH.
Patients and methods
Over the past 7 years, one of us (THL) and her clinical staff examined 73 FM patients (68 women and 5 men), who contributed to a skin biopsy for ultrastructural assessments. Two 55 and 60 year-old women, who suffered from long standing FM, had no signs of joint laxity (0/9 Beighton score) nor EDSH family history. A total of 71 patients (66 women and 5 men), who were 15-70 year-old, had a Beighton score ranging between 0 and 7/9, mostly 4 or 5/9. They presented with a velvety and/or moderately hyperextensible skin, multiple minor EDSH signs such as sprains, joint (sub) luxations, easy bruising, and enlarged atrophic scars, Gorlin sign and, occasionally, a positive EDSH family history. Some patients had a 4/9 Beighton score, that was too low for a diagnosis of typical EDSH, but fitted with JHS. Some authors consider JHS as a minor form of EDSH [27-32]. Joint laxity is influenced by gender, and regresses with age and repeat joint micro traumatisms. A skin biopsy was taken from a sun protected area such as the armpit and buttock in order to avoid prominent actinic changes. The samples were fixed in 4% glutaraldehyde in phosphate buffer at pH 4.7, post-fixed in 1% osmium tetroxide and embedded in Epon. Semithin sections were stained with 0.5% toluidine blue. Ultrathin sections were stained with uranyl acetate and lead citrate. A Zeiss EM 910 electron microscope was operated at 60 kV.
Results
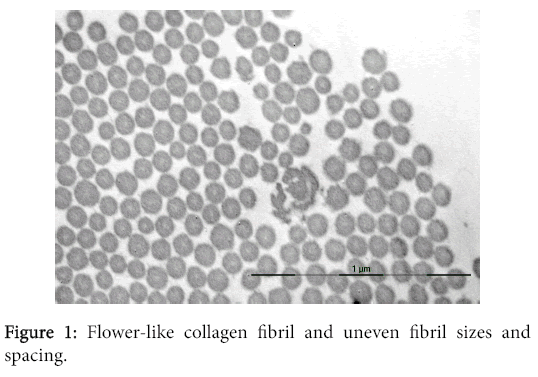
Skin ultrastructural examinations of the 71 FM patients with EDSH signs and familial history, revealed abnormalities in collagen and elastic fibers, and in other dermal components, similar to those found in EDSH. Collagen bundles showed uneven rounded fibril sizes, some flower-like collagen fibrils (Figure 1) and irregularly widened interfibrillar spacing. Elastic fibers exhibited irregular contours (Figure 2). Such aspects were absent in skin samples from normal individuals and from the two FM patients without EDSH clinical signs.
Discussion
At present, morphological observation of the dermal structure does not represent an outdated approach. It allows a better understanding of many connective tissue disorders in combination with molecular and genetic evaluations when possible [1]. FM and EDSH share some similar clinical aspects including joint laxity, chronic widespread pain, chronic fatigue, sleep disturbance, functional gastrointestinal manifestations and cognitive symptoms. Both FM and EDSH are more prevalent in women than in men [4,33,34]. The FM pathogenesis remains unclear, but the role of sex hormones seems to be limited [35,36]. EDSH is considered to be linked to autosomal dominant inheritance, but the role of sex hormones on the musculoskeletal system possily explains the predominance of EDSH in women.
There is an absence of genetic and biochemical markers in FM and EDSH, but skin ultrastructural abnormalities are well described in EDSH. For such reasons, we used skin biopsies for comparing these two pathological entities. Skin biopsy of some FM patients showed some dermal ultrastructural abnormalities indistinct from those found in EDSH. Such findings suggest that some FM types possibly represent undiagnosed EDSH. Genetic and molecular basis similar to EDSH might be considered as eventual candidates for the FM etiology. Distinctive clinical criteria for EDSH and FM remain crude and unsettled. Microscopy does not distinguish both conditions. We conjecture about a clear-cut distinction between them. At present, electron microscopy provides similar information for both conditions. However, similarity does not mean common genetic and molecular origin for both conditions although it possibly suggests the presence of related defects. Of note, signs and symptoms suggesting FM are also present in patients suffering from JSH [37]. Such cases are commonly misdiagnosed EDSH, FM and JHS. They are considered in the field of extracellular matrix disorders. The presently reported ultrastructural findings are in line with such concept. The present study represents the first attempt using skin ultrastruture for distinguishing EDSH and JHS from FM. Our conclusions are in line with clinical opinions supporting some similarities between these disorders, and perhaps common molecular causes for these clinical challenges. A common characteristic is the present of a non-inflammatory connective tissue disorder with similar ultrastructural changes in the collagen and elastic fibers. The impact on comorbidities and quality of life is frequent. Pain and disability are occasionally prominent. The relationship between EDSH, FM and JHS should be taken into consideration in the diagnosis and follow-up of women. Such consideration has a broad impact on chronic pain and daily life.
Acknowledgement
The authors appreciate the contribution of physicians who referred the patients to our clinical facilities, and the excellent secretariat assistance of Mrs Marie Marmol and Magali Caes. The paper has not been supported by external financing.
References
- Hermanns-Lê T, Reginster MA, Piérard-Franchimont C, Piérard G (2013) Ehlers-Danlos syndrome in Diagnostic electron microscopy: a practical guide to interpretation and technique. John W Stirling, Alan Curry and Brian Eyden, John Wiley & Sons, Ltd, Chichester. 309-321.
- Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Katz RS, et al. (2010) The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res (Hoboken) 62: 600-610.
- Wolfe F (2010) New American College of Rheumatology criteria for fibromyalgia: a twenty-year journey. Arthritis Care Res (Hoboken) 62: 583-584.
- Jahan F, Nanji K, Qidwai W, Qasim R (2012) Fibromyalgia syndrome: an overview of pathophysiology, diagnosis and management. Oman Med J 27: 192-195.
- Segura-Jiménez V,Aparicio VA,Álvarez-Gallardo IC,Soriano-Maldonado A,Estévez-López, et al. (2014) Validation of the modified 2010 American College of Rheumatology diagnostic criteria for fibromyalgia in a Spanish population. Rheumatology (Oxford) 53: 1803-1811.
- Acasuso-Díaz M, Collantes-Estévez E (1998) Joint hypermobility in patients with fibromyalgia syndrome. Arthritis Care Res 11: 39-42.
- Fitzcharles MA (2000) Is hypermobility a factor in fibromyalgia? J Rheumatol 27: 1587-1589.
- Karaaslan Y, Haznedaroglu S, Oztürk M (2000) Joint hypermobility and primary fibromyalgia: a clinical enigma. J Rheumatol 27: 1774-1776.
- Lai S, Goldman JA, Child AH, Engel A, Lamm SH (2000) Fibromyalgia, hypermobility, and breast implants. J Rheumatol 27: 2237-2241.
- Goldman JA (2001) Fibromyalgia and hypermobility. J Rheumatol 28: 920-921.
- Holman AJ (2002) Is hypermobility a factor in fibromyalgia? J Rheumatol 29: 396-398.
- Kasapçopur O, Tengirsek M, Ercan G, Yologlu N, Caliskan S, et al. (2004) Hypermobility and fibromyalgia frequency in childhood familial Mediterranean fever. Clin Exp Rheumatol 22: 79.
- Ofluoglu D, Gunduz OH, Kul-Panza E, Guven Z (2006) Hypermobility in women with fibromyalgia syndrome. Clin Rheumatol 25: 291-293.
- Sendur OF, Gurer G, Bozbas GT (2007) The frequency of hypermobility and its relationship with clinical findings of fibromyalgia patients. Clin Rheumatol 26: 485-487.
- Ting TV, Hashkes PJ, Schikler K, Desai AM, Spalding S, et al. (2012) The role of benign joint hypermobility in the pain experience in Juvenile Fibromyalgia: an observational study. Pediatr Rheumatol Online J 10: 16.
- Beighton P,De Paepe A,Steinmann B,Tsipouras P,Wenstrup RJ (1998) Ehlers-Danlos syndromes: revised nosology, Villefranche, 1997. Ehlers-Danlos National Foundation (USA) and Ehlers-Danlos Support Group (UK). Am J Med Genet 77: 31-37.
- Rombaut L, Malfait F, De Wandele I, Cools A, Thijs Y, et al. (2011) Medication, surgery, and physiotherapy among patients with the hypermobility type of Ehlers-Danlos syndrome. Arch Phys Med Rehabil 92: 1106-1112.
- Hermanns-Lê T,Piérard GE,Piérard-Franchimont C (2015) [Ehlers-Danlos Syndrome of the Hypermobile Type: A Multisystemic Disorder. Contribution of Skin Ultrastructure to Individual Management]. Rev Med Liege 70: 325-330.
- Miller VJ,Zeltser R,Yoeli Z,Bodner L (1997) Ehlers-Danlos syndrome, fibromyalgia and temporomandibular disorder: report of an unusual combination. Cranio 15: 267-269.
- Hermanns-Lê T, Piérard GE, Angenot P (2013) [Fibromyalgia: an unrecognized Ehlers-Danlos syndrome hypermobile type?]. Rev Med Liege 68: 22-24.
- Hausser I,Anton-Lamprecht I (1994) Differential ultrastructural aberrations of collagen fibrils in Ehlers-Danlos syndrome types I-IV as a means of diagnostics and classification. Hum Genet 93: 394-407.
- Holbrook KA,Byers PH (1982) Structural abnormalities in the dermal collagen and elastic matrix from the skin of patients with inherited connective tissue disorders. J Invest Dermatol 79: 7s-16s.
- Barton SP, Marks R (1984) Measurement of collagen-fibre diameter in human skin. J Cutan Pathol 11: 18-26.
- Mensing H, Schaeg G (1984) 'Composites'--an aberrant structure of the collagen fibril. Dermatologica 168: 1-9.
- Piérard GE, Lê T, Hermanns JF, Nusgens BV, Lapière CM (1987) Morphometric study of cauliflower collagen fibrils in dermatosparaxis of the calves. Coll Relat Res 6: 481-492.
- Piérard GE, Lê T, Piérard-Franchimont C, Lapière CM (1988) Morphometric study of cauliflower collagen fibrils in Ehlers-Danlos syndrome type I. Coll Relat Res 8: 453-457.
- Grahame R (1999) Joint hypermobility and genetic collagen disorders: are they related? Arch Dis Child 80: 188-191.
- Grahame R (2000) Heritable disorders of connective tissue. Baillieres Best Pract Res Clin Rheumatol 14: 345-361.
- Zweers MC, Kucharekova M, Schalkwijk J (2005) Tenascin-X: a candidate gene for benign joint hypermobility syndrome and hypermobility type Ehlers-Danlos syndrome? Ann Rheum Dis 64: 504-505.
- Trinh Hermanns-Lê,Marie-Annick Reginster,Claudine Piérard-Franchimont,Philippe Delvenne, Gérald E. Piérard, et al. (2012) Dermal Ultrastructure in Low Beighton Score Members of 17 Families with Hypermobile-Type Ehlers-Danlos Syndrome. J Biomed Biotecnol.
- Castori M,Morlino S,Celletti C,Ghibellini G,Bruschini M, et al. (2013) Re-writing the natural history of pain and related symptoms in the joint hypermobility syndrome/Ehlers-Danlos syndrome, hypermobility type. Am J Med Genet A 161: 2989-3004.
- Castori M,Dordoni C,Valiante M,Sperduti I,Ritelli M, et al. (2014) Nosology and inheritance pattern(s) of joint hypermobility syndrome and Ehlers-Danlos syndrome, hypermobility type: a study of intrafamilial and interfamilial variability in 23 Italian pedigrees. Am J Med Genet A 164: 3010-3020.
- Castori M, Camerota F, Celletti C, Grammatico P, Padua L (2010) Ehlers-Danlos syndrome hypermobility type and the excess of affected females: possible mechanisms and perspectives. Am J Med Genet A 152A: 2406-2408.
- De Paepe A, Malfait F (2012) The Ehlers-Danlos syndrome, a disorder with many faces. Clin Genet 82: 1-11.
- Okifuji A, Turk DC (2006) Sex hormones and pain in regularly menstruating women with fibromyalgia syndrome. J Pain 7: 851-859.
- Bramwell BL (2010) The role of sex hormones on fibromyalgia pain mediators. Int J Pharm Compd 14: 193-199.
- Bravo JF (2009) [Ehlers-Danlos syndrome, with special emphasis in the joint hypermobility syndrome]. Rev Med Chil 137: 1488-1497.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 19855
- [From(publication date):
January-2016 - Apr 03, 2025] - Breakdown by view type
- HTML page views : 18946
- PDF downloads : 909