Skin and Nasal Vestibule Colonisation by Staphylococcus aureus and Its Susceptibility to Drugs in Atopic Dermatitis Patients - Comments to the Results of the Project
Received: 24-Dec-2020 / Editor assigned: 01-Jan-1970 / Reviewed: 01-Jan-1970 / Revised: 01-Jan-1970 / Accepted Date: 06-Jan-2021 / Published Date: 13-Jan-2021
Description
It is widely known that inflammation in the course of AD is stimulated by the antigens of skin-colonising microorganisms. Damage to the epidermal barrier facilitates their penetration into the epidermis and dermis. Staphylococcus aureus (S. aureus) has a predominant role among the pathogens responsible for exacerbation of the dermatological condition in AD patients.
The aim of the study was to assess the frequency of colonisation of the nasal vestibule and apparently healthy skin by S. aureus and to assess dermal lesions for superinfection with S. aureus in AD patients.
The research was performed on a population of 100 AD patients (48 men and 52 women) aged 2-76 years. Three smears were collected for microbial tests: one from the nasal anterior nares, one from the skin where lesions appeared at the moment of investigations and one from the skin which was free from the eczema.
Among the 100 patients S. aureus was present at least in one location in 90 patients (90%). In 10 patients (10%) it was not found in any location.
44 patients (44%) presented S. aureus colonization of apparently healthy skin and within skin lesions. In case of 23 patients (23%) this particular pathogen was detected only in skin lesions, whereas 6 patients (6%) had a positive result within the area of apparently healthy skin. In total, S. aureus was detected in the skin of 73 patients (73%). In 50 out of 82 patients (61%) apparently healthy skin has been colonized with S. aureus, whereas in 67 out of 83 patients (81%) colonization has been proven within the skin lesions in Table 1.
| Age category, years | S. aureus colonisation in patients, n (%) | ||
|---|---|---|---|
| Nasal | Non-lesioned skin | Lesioned skin | |
| <15 ( n=32) | 23 (72) | 9 (28) | 20 (62.5) |
| >15 ( n=68) | 44 (65) | 37 (54) | 45 (66) |
Table 1: Skin and nasal colonisation by Staphylococcus aureus in different age groups of patients with atopic dermatitis.
S. aureus was detected in the nasal vestibule of 70 out of 82 AD patients (85%) tested for the presence of the pathogen. Among the group of the 70 patients with S. aureus in their anterior nares the pathogen was also found on the skin surface of 54 patients (77.1%). Results were negative in case of the skin of 6 patients (8.6%). 10 patients did not have their skin examined for the presence of S. aureus (14.3%).
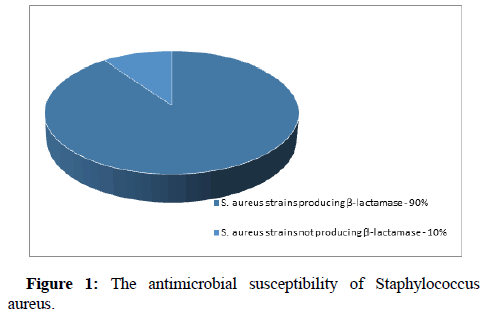
Antibiograms were made for all the S. aureus strains cultured from the skin lesions. 90% of the strains produced penicillinase (Figure 1). 90% of the strains were sensitive to tetracyclines. 100% were sensitive to levofloxacin, vancomycin, teicoplanin, tigecycline and linezolid. The strains were also assessed for sensitivity to macrolides (sensitivity to erythromycin amounted to 87%), clindamycin (91%) and trimethoprim/sulfamethoxazole (98%). As far as external use drugs are concerned, the strains were sensitive to gentamicin (94%), fusidic acid (99%), fosfomycin and mupirocin (100%) (Figure 2).
As far as the nasal vestibule smear is concerned, S. aureus was more often isolated in the group of children aged under 15 years (72%). As far as the colonisation of apparently healthy skin and the superinfection of skin lesions with S. aureus are concerned, there were higher values in the group of adults, i.e. patients aged over 15 years (54% and 66%, respectively). Apart from that, in the population of young people aged less than 15 years the percentage of positive results of the microbial test for the presence of S. aureus in apparently healthy skin was two times smaller than the percentage of positive results showing the presence of S. aureus in AD skin lesions. These values were similar in the group of patients aged over 15 years.
Conclusion
S. aureus colonises skin in most AD patients. S. aureus also colonises apparently healthy skin in AD patients. Most AD patients carry S. aureus in their nasal vestibules. S. aureus does not seem to colonise apparently healthy skin as often as skin lesions in young people (aged less than 15 years). The vast majority of S. aureus strains were sensitive to local antibiotics, i.e. fusidic acid and mupirocin. Due to the fact that most S. aureus strains produced penicillinase (90%) in AD patients, it is recommended to administer antibiotic therapy with β-lactamase inhibitors.
Citation: Operacz CM (2021) Skin and Nasal Vestibule Colonisation by Staphylococcus aureus and Its Susceptibility to Drugs in Atopic Dermatitis Patients: Comments to the Results of the Project. J Mucosal Immunol Res 5: 127.
Copyright: © 2021 Operacz C M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 1648
- [From(publication date): 0-2021 - Apr 29, 2025]
- Breakdown by view type
- HTML page views: 929
- PDF downloads: 719