Case Report Open Access
Single Step Simultaneous Bijaw Surgery and Alveolar Bone Grafting in an Adult with Cleft Lip and Palate: A Case Report
Agarwal SS1*, Karan Nehra2, Jayan B2, Sahoo NK3, Mohit Sharma4 and Prasanna Kumar4
1Department of Orthodontics, Indian Army Dental Corps, India
2Department of Orthodontics, Army Dental Centre R&R, New Delhi, India
3Department of Oral & Maxillofacial Surgery, Indian Army Dental Corps, India
4Department of Orthodontics, Armed Forces Medical College, Pune, India
- Corresponding Author:
- Agarwal SS, MDS
Department of Orthodontics
Indian Army Dental Corps, India
E-mail: docshivagarwal@rediffmail.com
Received Date: April 23, 2015; Accepted Date: June 07, 2016; Published Date: June 13, 2016
Citation: Agarwal SS, Nehra K, Jayan B, Sahoo NK, Sharma M, et al., (2016) Single Step Simultaneous Bijaw Surgery and Alveolar Bone Grafting in an Adult with Cleft Lip and Palate: A Case Report. Cosmetol & Oro Facial Surg 2:107. doi:10.4172/jcofs.1000107
Copyright: © 2016 Agarwal SS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Cosmetology & Oro Facial Surgery
Abstract
Cleft lip and palate (CLP) is one of the most common congenital anomaly affecting the oro-facial region. Growth and development is variously affected in such patients which in turn affect the social and psychological maturation of the individual along with its negative impact on facial aesthetics. Numerous multi-centric studies have been conducted world-wide to establish a specific treatment protocol for the management of CLP cases to achieve ideal results. But the situation, especially in developing countries is still alarming and it is not uncommon to encounter untreated/partially treated adult CLP patients in our clinical practice. The aim of this case report is to highlight interdisciplinary management of such an adult case of unilateral cleft lip and palate (GOSLON 5) along with moderate velopharyngeal incompetency (alveolar grafting was never attempted) by single step simultaneous bijaw surgery and alveolar bone grafting.
Keywords
Bijaw surgery in cleft patients; Alveolar bone grafting in adult cleft cases; GOSLON 5
Introduction
Oro-facial region is variously affected by syndromes and craniofacial clefts which occur due to non-fusion of embryonic processes during intra-uterine stages of development. Cleft Lip and/or Palate (CL ± P) are one of them and are the second most common congenital anomaly affecting humans [1]. The incidence of (CL ± P) worldwide is 1 in 600 live births and its prevalence is 9.92 per 10,000. The prevalence of CL alone is 3.28 per 10,000 and that of CLP 6.64 per 10,000 [2]. In India, about 28,600 children are born with CL ± P every year which amount of about 3 infants born every hour with this deformity [3]. In United States, its incidence is approximately 1/700 live births [4].
Craniofacial growth and development is very important for social and psychological maturation of the individual along with its impact on facial aesthetics. These parameters are adversely affected in CLP patients. Multi-centric studies conducted world-wide in developed countries over past few decades [5,6] have defined specific treatment protocols for the management of CLP patients to achieve ideal results. These studies have been funded by various healthcare agencies as well as various government and non-government organizations. However due to non-availability of cleft lip and palate teams/centres in developing countries, it is not very uncommon to see untreated/partially treated adult patients in these countries.
This article describes an adult case of unilateral cleft lip and palate (left side)-GOSLON 5 [6] with severe maxillo-mandibular dento-skeletal discrepancy (Class III) and moderate velopharyngeal incompetency which was managed ortho-surgically by single step simultaneous bijaw surgery and alveolar bone grafting.
Case Report
History
An 18 years old male reported to the Division of Orthodontics and Dentofacial Orthopedics at Armed Forces Medical College, Pune with chief complaint of forwardly placed lower jaw, irregularly placed teeth and gap in the upper jaw. He was a known case of unilateral CLP (left side), where primary closure of lip and palate was done at 3 and 18 months of age respectively and alveolar grafting was never attempted. He was the second of the two male children from his parents with no history of similar problems in family. The age of the father and mother was 35 and 33 years respectively at the time of his birth. Mother presented with the history of normal pregnancy and delivery.
Clinical examination
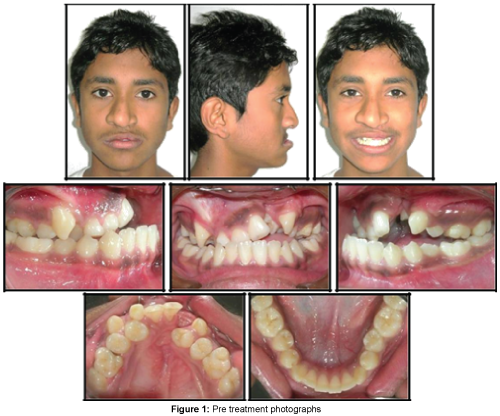
The patient presented with a dished-in midface, concave facial profile, acute nasolabial angle, scar mark on left side of upper lip (indicating previous surgery) and facial asymmetry due to nasal tip being deviated towards right side. Overall facial aesthetics of the patient was poor leading to restriction in social activities (Figure 1).
Speech evaluation done by an Otolaryngologist revealed difficulty in pronouncing words like /p/, /s/ and /f/ along with a moderate velopharyngeal incompetence and hyper-nasality of voice. There was however, no nasal regurgitation of oral fluids.
Intra-oral examination revealed a collapsed maxillary arch with an occult cleft, clinically absent 21 and 22, retained 53, scar mark on the palate indicating previous palatal repair, 14 and 24 placed palatal to 13 and 23 and lateral open bite (3 mm) on left side. Tooth Size Arch Length Discrepancy (TSALD) revealed crowding of 1.5 mm in maxilla and 2 mm in mandible along with a reverse overjet of 11 mm (Figure 1).
Radiographic assessment
Lateral cephalometric analysis revealed Class III skeletal and dentoalveolar pattern along with a retrognatic maxilla and a relatively prognathic mandible (SNA=68°, ANB=-9°, A-Na vertical=-13 mm), retroclined mandibular incisors (LI-NB=17°(3), IMPA=84°) and an acute nasolabial angle (60°) (Figure 2) (Table 1).
| Cephalometric Parameter | Observed value |
|---|---|
| SNA | 68° |
| SNB | 77° |
| ANB | -9° |
| UI-NA | 28°(5) |
| LI-NB | 17°(3) |
| GoGn–SN | 34° |
| FMA | 27° |
| IMPA | 84° |
| Co-A | 73mm |
| Co-Gn | 127 mm (95-97 mm) |
| LAFH | 69 mm |
| Pog-Na vert | -2 mm |
| A-Na vert | -13 mm |
| ANSPNS:GoPog | 1:1.6 (1:1.5) |
| Nasolabial angle | 60° |
Table 1: Pre-treatment cephalometric parameters.
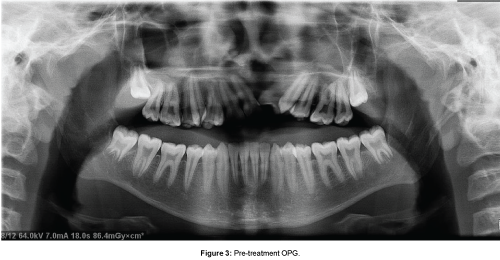
Orthopantomogram (OPG) findings revealed that the patient was in a permanent dentition stage with agenesis of 21, 22 and retained 53. No supernumerary teeth or radiographic evidence of any obvious pathology was evident. Maxillary alveolar defect was seen in the region of 21 and 22 (Figure 3).
Diagnosis
The patient was diagnosed as an operated case of UCLP - left side (GOSLON 5) associated with severe maxillary hypoplasia, collapsed maxillary arch and moderate velopharyngeal incompetence.
Treatment progress
Pre-surgical orthodontics
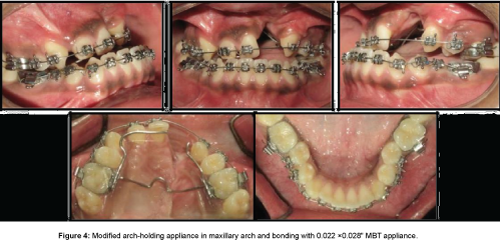
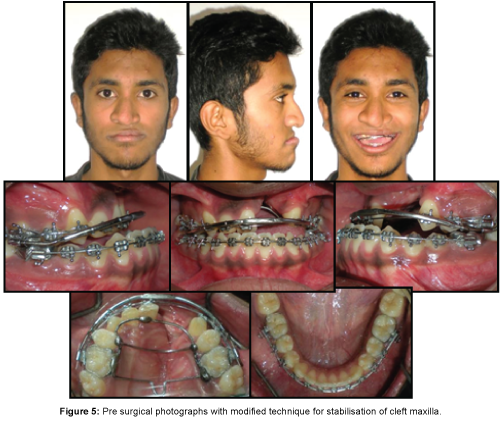
After therapeutic extraction of 53, 14 and 24, maxillary arch expansion was initiated as a preliminary procedure using Quad helix appliance and expansion was done as per protocol [1]. After the desired expansion was achieved, a fixed arch holding appliance was fabricated in maxilla to prevent relapse and fixed mechanotherapy with 0.022 × 0.028” MBT Pre Adjusted Edgewise Appliance (PEA) was initiated (Figure 4). After leveling and alignment of maxillary and mandibular arch, sequentially the patient was placed on rigid (0.021 × 0.025” Stainless Steel) arch wires. A modified technique [7] was used to stabilize the cleft maxilla pre-surgically using inner bow of face bow and a rigid palatal framework (Figure 5).
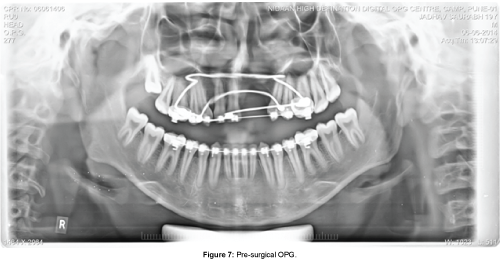
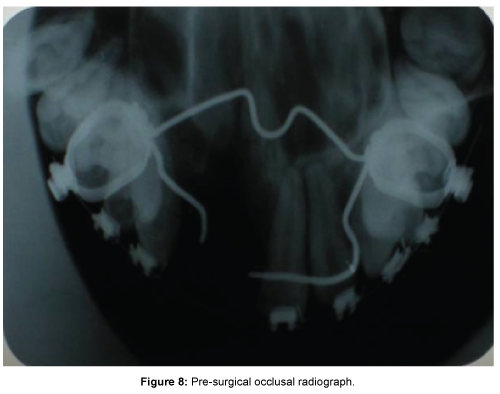
Pre-surgical lateral cephalgram (Figure 6) (Table 2) revealed dentoalveolar decompensation and optimization of maxillary and mandibular dentition (UI-NA=32°(6), LI-NB=21°(3), IMPA=88°). Pre-surgical OPG (Figure 7) confirmed parallel alignment of roots prior to surgery and occlusal radiograph revealed widening of the cleft defect (Figure 8).
| Cephalometric Parameter | Pre-treatment values | Pre-surgical values |
|---|---|---|
| SNA | 68 ° | 68 ° |
| SNB | 77 ° | 77 ° |
| ANB | -9 ° | -9 ° |
| UI-NA | 28 °(5) | 32°(6) |
| LI-NB | 17 °(3) | 21°(3) |
| GoGn –SN | 34 ° | 34 ° |
| FMA | 27 ° | 27 ° |
| IMPA | 84 ° | 88 ° |
| Co-A | 73mm | 73 mm |
| Co-Gn | 127mm(95-97) | 127 mm |
| LAFH | 69mm | 69 mm |
| Pog-Na vert | -2mm | -2 mm |
| A-Na Vert | -13mm | -12 mm |
| ANS-PNS:GoPog | 1:1.6 (1:1.5) | 1: 1.86 |
| Nasolabial angle | 60 ° | 56° |
Table 2: Pre-surgical cephalometric parameters.
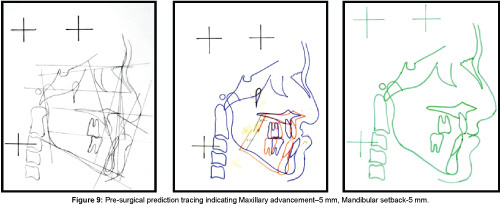
Pre-surgical prediction tracing (Figure 9) indicated need of a Bijaw surgery with maxillary advancement of 5 mm and mandibular setback of 5 mm to achieve optimum skeletal and dental relationship.
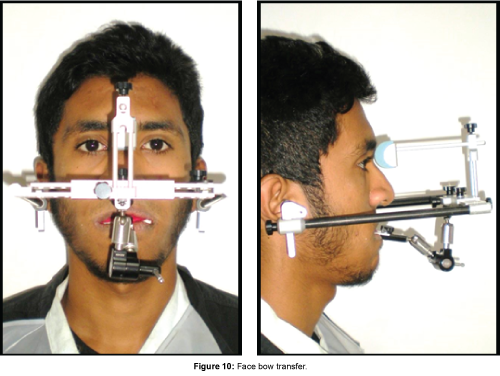
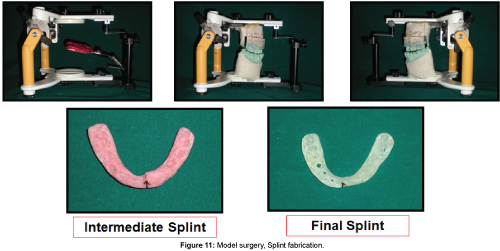
Face bow transfer (Figure 10) was then carried out to achieve correct orientation of maxilla in relation to the cranial base. The mandible was then aligned in relation to maxilla by occlusal wax bite record at centric occlusion.
The casts were then articulated on a semi-adjustable articulator and subjected to model surgery. Splint fabrication was then done for the planned two stage surgical procedure. Stage 1 (intermediate) splint was fabricated for maxillary advancement using pink acrylic and final splint was fabricated for mandibular setback using white acrylic resin (Figure 11).
Surgical phase
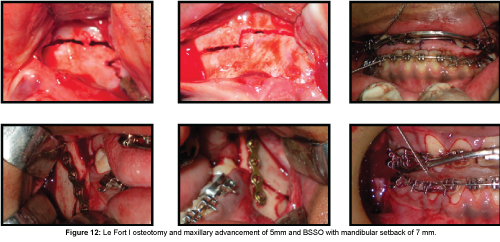
Under general anaesthesia, Le Fort I osteotomy and maxillary down fracture was done in stage 1 surgery and maxilla was advanced by 5 mm as guided by stage 1 splint and fixed in that position by rigid fixation. In stage 2 surgery, Bilateral Sagittal Split Osteotomy (BSSO) and mandibular setback of 7 mm was performed as guided by stage 2 splint and the mandible was stabilised in that position using rigid fixation (Figure 12).
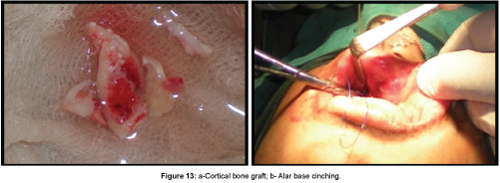
Cancellous bone from iliac crest was harvested and grafted into the alveolar defect region by raising full thickness mucoperiosteal flaps (Figure 13a). Alar base cinching was done simultaneously to prevent excessive nasal flaring which usually occurs after maxillary advancement surgery (Figure 13b).
Post-surgical phase
The stage 2 splint was cemented on the maxillary dentition with Glass ionomer cement on the third post operative day to guide mandibular movements and it remained in situ for 3 weeks (Figure 14).
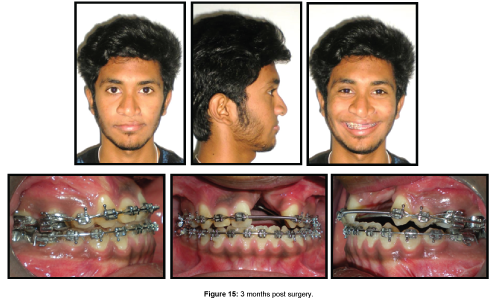
Photographs taken 3 months post operatively shows marked improvement in facial profile and occlusion of the patient (Figure 15).
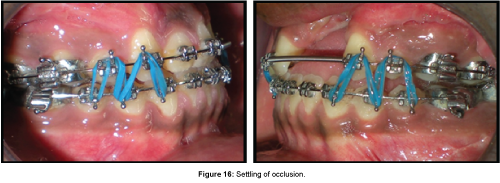
Settling of occlusion was done after completion of finishing and detailing of occlusion using inter-arch elastics (Figure 16).
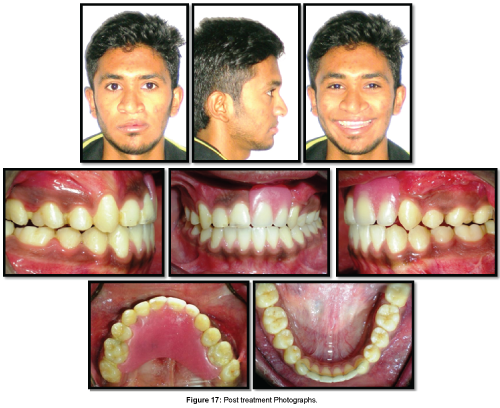
A removable partial denture was fabricated for the patient which simultaneously served two purposes: firstly, it replaced missing teeth and restored gingival aesthetics and secondly, it provided rigid transverse stabilisation of maxilla to prevent its collapse post treatment. It was analysed that there was an inadequate alveolar bone support even after alveolar bone grafting and hence the option of prosthetic rehabilitation with fixed partial denture or implants was ruled out. Also both these rehabilitation modalities would have not provided transverse stabilisation of maxilla warranting the need for a separate arch holding appliance to prevent post treatment relapse (Figure 17).
Post treatment lateral cephalogram (Figure 18) (Table 3) revealed optimization of dento-skeletal parameters of the patient as shown by achievement of a positive overjet (ANB=1°), an optimised position of maxilla (SNA=73°, A-Na vertical=-2 mm), mandible (SNB=72°, Pog to Na-vertical=2 mm), dentition (UI-NA=27°(6), LI-NB=21°(3)), nasolabial angle (87°) and achievement of lip competency.
| Cephalometric Parameter | Pre-treatment values | Post-treatment values |
|---|---|---|
| SNA | 68° | 73° |
| SNB | 77° | 72° |
| ANB | -9° | 1° |
| UI-NA | 28°(5) | 27°(6) |
| LI-NB | 17°(3) | 21°(3) |
| GoGn –SN | 34° | 38° |
| FMA | 27° | 32° |
| IMPA | 84° | 85° |
| Co-A | 73 mm | 79 mm |
| Co-Gn | 127 mm | 120 mm |
| LAFH | 69 mm | 71 mm |
| Pog-Na vert | -2 mm | 2 mm |
| A-Na Vert | -13 mm | -2 mm |
| Nasolabial angle | 60° | 87° |
Table 3: Post-treatment cephalometric parameters.
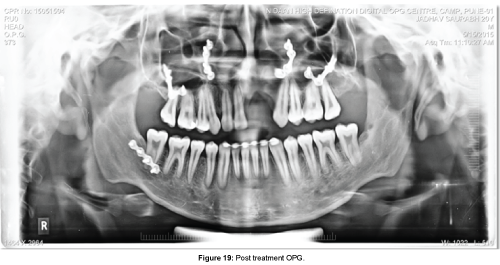
Post treatment OPG revealed achievement of root parallelism and absence of clinically significant root resorption (Figure 19).
Post treatment extra-oral photographs shows marked improvement in facial aesthetics, profile, occlusion and self confidence of the patient without adversely affecting his speech. Bonded fixed spiral wire retainers were placed for retention in the lower arch (Figure 17).
Total treatment duration was 24 months and at the end of treatment we could achieve a marked improvement in self-esteem and confidence of the patient. The patient is on periodic recall and maintenance therapy.
Discussion
The management of CLP patients requires an interdisciplinary approach beginning with pre-natal diagnosis and counselling of parents, management of airway and feeding problems at birth, monitoring the growth and development of the child and possible intervention whenever required [8,9]. CLP cases present with varying levels of difficulty and challenges to the cleft team which include speech and aesthetic problems, mid-face deficiency (sometimes associated with actual or relative mandibular excess as seen in our case), narrow maxilla, malformed or missing (21 and 22 in our case)/supernumerary teeth, varying severity of alveolar defects and oro-antral communications. Aesthetics and speech are often primary complains (as in our case) which may jeopardise the social life of these patients [10,11].
The present case was an adult patient whose treatment was not properly monitored throughout his growth and development and arch expansion and/or alveolar grafting were never attempted [5,6,12]. Arch expansion is an important step in management of transverse discrepancy in CLP patients and is usually done prior to alveolar grafting. In the present case, arch expansion was carried out with Quad helix appliance as per standard protocol (approximate duration=6 months) [1,12]. A 0.022 × 0.028” slot appliance was selected since it permitted use of stiffer wires pre-surgically (0.021 × 0.025 Stainless Steel wires in our case). A modified appliance framework was designed to stabilise and unify maxilla pre-surgically [7]. It served two purposes: firstly, it helped in rigid unification of cleft maxilla and prevented its collapse intra-operatively during Le-fort 1 osteotomy and maxillary down fracture. Secondly, it permitted simultaneous use of intermediate and final splints during two stage surgical procedure, which would not have been possible without this technique [7,13,14]. The present case was in CVMI stage 6 with minimal/no growth left. There was a severe maxillary deficiency along with relative mandibular excess and moderate velopharyngeal incompetency. Maxillary protraction with rigid external distraction device was not feasible (which required about 13-14 mm of maxillary protraction) as this might have worsened the velopharyngeal incompetency and reduced post-treatment stability. The scar tissue from previous palatal surgeries increase chances of post treatment relapse in CLP patients especially in cases of large overjet as in the present case [1,15]. Hence, bijaw surgery was considered as a better alternative since bijaw surgeries provide more stable results and its effects on velopharyngeal incompetency and airway are minimal [1]. A tertiary alveolar grafting with anterior iliac crest bone (cancellous bone) was planned simultaneously during the bijaw surgery as primary and secondary alveolar grafting were never attempted for this patient. The cancellous bone of anterior iliac crest is usually a gold standard because it incorporates and vascularises well in the grafted area; allow tooth eruption through it and also stimulates adjacent undifferentiated cells to differentiate into a healthy attachment apparatus. In the present case, the rigid stabilisation framework was removed 6 weeks postsurgically to provide sufficient immobilisation time to the graft. Success rates are variable in tertiary alveolar grafting and in our case it was a partial failure as insufficient bone was available post-grafting to place an implant [13,14,16,17].
Conclusion
Single step bijaw surgery with tertiary alveolar bone grafting is a viable option in adult untreated/incompletely treated cases with large dento-skeletal discrepancies and velopharyngeal incompetency. Proper case selection and an interdisciplinary team approach is a key factor in successful management of such cases. Long-term follow-up and maintenance of the treatment results is as important as the treatment itself.
References
- Profit WR, Fields WH, Sarver MD (2001) Contemporary Orthodontics. (4thedn), Elsevier publishers, pp: 74-75.
- Redett RJ (2009) A guide to understanding Cleft Lip and palate Dallas, Texas: Children’s craniofacial association.
- Sah RK, Powar R (2014) Epidemiological Profile of Cleft Lip and Palate Patients Attending Tertiary Care Hospital and Medical Research Centre, Belgaum, Karnataka-A Hospital Based Study. IOSR J Dent Med Sciences 13: 78-81.
- Gorlin RJ, Cervenka J, Pruzansky S (1971) Facial clefting and its syndromes. In Bergsma D, ed. The clinical delineation of birth defects. Part XI, Orofacial Structures. Baltimore: Williams & Wilkins 7: 3-46.
- Mars M, Asher C, Brattstrom V, Dahl E, Mc William J, et al. (1992) A six centre comparison of treatment outcome in UCLP. Dental arch relationships. The Cleft Palate-Craniofacial journal 29: 405-408.
- Mars M, Plint DA, Houston WJB, Bergland O, Semb G (1987) The Goslon Yardstick: A new system of assessing dental arch relationships in children with unilateral clefts of the lip and palate. Cleft Palate J 24:314-322.
- Agarwal SS, Jayan B, Sahoo NK, Thapa A (2014)Stabilisation of cleft maxilla using modified technique during bi-jaw orthognathic surgical procedures with simultaneous use of two stage surgical splints, Medical Journal Armed Forces India 71: S415-S417.
- Maserai AG, Sell D, Habel A, Mars M, Sommerland BC, Wade A (2007)The nature of feeding in infants with un- repaired cleft lip and/or palate compared with healthy noncleft infants. Cleft Palate Craniofac J 44: 321-328.
- Tai K, Park JH, Okadakage S, Mori S, Sato Y (2012) Orthodontic treatment for a patient with a unilateral cleft lip and palate and congenitally missing maxillary lateral incisors and left second premolar. Am J Orthod and Dentofacial Ortho 141: 363-373.
- Olin WH (1964) Dental anomalies in cleft lip and cleft palate patients. Angle Orthod 34:119-123.
- Kang JH, Kang JS, Son WS (1993) A study of the frequency of congenital missing and supernumerary teeth in cleft lip and palate patients. Korean J Orthod 23:319-326.
- Cash AC (2012) Orthodontic treatment in the management of cleft lip and palate. Front Oral Biol16:111-123.
- Burstein FD, Maurice SM, Granger M, Williams JK (2012) Maxillary advancement in patients with severe maxillary hypoplasia: role of adjuvant stabilization techniques and materials. J CraniofacSurg 23:812-816.
- Helm JA, Speidel TM, Denis KL (1987) Effect of timing on long term clinical success of alveolar cleft bone grafts. Am J OrthodDentofacOrthop 92:232-240.
- Geraedts CT, Borstlap WA, Groenewoud JMM, and Stoelinga PJW (2007) Long-term evaluation of bilateral cleft lip and palate patients after early secondary closure and premaxilla repositioning. Int J of Oral and MaxillofacSurg36:788-796.
- Posnick J, Dagys A (1994)Skeletal stability and relapse patterns after Le Fort I maxillary osteotomy fixed with mini-plates: the unilateral cleft lip and palate deformity. PlastReconstrSurg 94:924-932.
- De Silva FOG, Okada HY, CapelozzaFilho L, Suguimoto RM (1998) Orthodontic traction of a permanent canine through a secondary bone graft in a unilateral cleft lip and palate patients. J ClinOrthod 32:417-422.
--
Relevant Topics
- Blepharoplasty
- Bone Anchored Hearing Aids
- Chemical peel
- Cleft Surgery
- Congenital Craniofacial Malformations
- Cosmetic Facial Surgery
- Craniofacial Surgery
- Dental Orofacial Surgery
- Dentoalveolar Surgery
- Head and Neck Reconstruction
- Injectable Cosmetic Treatments
- Lip Reconstruction
- Mandibular Nerve Surgery
- Maxfax Surgery
- Maxillofacial Surgery
- Neck Liposuction
- Oral and Maxillofacial Surgery
- Oral Surgery Surgeon
- Orofacial Surgery Braces
- Pediatric Maxillofacial Surgery
- Rhytidectomy
- Sleep Apnea Orofacial Surgery
- Temporomandibular Joint Disorders
- Upper Jaw Surgery
Recommended Journals
Article Tools
Article Usage
- Total views: 17195
- [From(publication date):
December-2016 - Apr 03, 2025] - Breakdown by view type
- HTML page views : 16104
- PDF downloads : 1091