Research Article Open Access
Single Anastomosis Gastro Ileal Bypass with Pyloric and Gastric Plication (SAGI PGP): A New Innovative Bariatric Operation
Ferman Faris Mohammed1* and Rafil Abdel Alwahab Aldaaod2
1General Surgery Branch, Department of General Surgery, Kurdistan Board of Medical Specialties, Hawler Medical University, Germany
2General Surgery Branch, Diploma of General Surgery, Kurdistan Board of Medical Specialties, Baghdad Medical City, Germany
- Corresponding Author:
- Ferman Faris Mohammed
General Surgery Department, Kurdistan Board of Medical Specialties
Hawler Medical University, Sinzheimer Street 14
Baden, Wurttemberg, 76530, Germany
Tel: +9647504638287
E-mail: mailto:farman.mbchb@yahoo.com
Received Date: June 27, 2016; Accepted Date: July 18, 2016; Published Date: July 24, 2016
Citation: Mohammed FF, Aldaaod RAA (2016) Single Anastomosis Gastro Ileal Bypass with Pyloric and Gastric Plication (SAGI PGP): A New Innovative Bariatric Operation. J Gastrointest Dig Syst 6:455. doi:10.4172/2161-069X.1000455
Copyright: © 2016 Mohammed FF, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License; which permits unrestricted use; distribution; and reproduction in any medium; provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
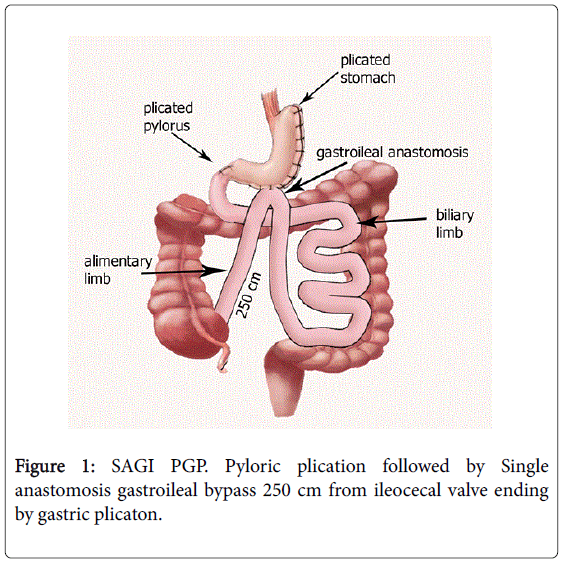
Objectives: Objective is to analyze the operation results of 270 patients in 2013, 2014 and 2015. Setting: Soran Private Hospital/Department of general &laparoscopic surgery/ErbilIraq. Methods: The mean BMI of patients is 43.5 kg/m2 with female patient were 165 and male patients were 115. Type 2 DM was presenting in 68 patients. Hypertension in 48 Hypercholesterolemia in 104, Hypertriglyceridemia in 178 and sleep apnea in 20, polycystic ovarian syndrome in 34 patients. Case study was possible for 240 patients in the 1st year post operation and 200 patients for the 2nd year and 130 in the 3rd year. Results: EWL is above 90% at first year, 85% at year 2. All diabetic patients return to normal blood sugar level usually at the first month with no need for any kind of anti-diabetic medication. Conclusion: SAGI PGP is a novel operation with the least complication that can happen in any other type of bariatric surgeries and the best EWL that can be expected. This technique is combination of single anastmosis gastroileostomy with gastric and pyloric placation. It is a simplified version of biliopancreatic diversion duodenal switch. SAGI PGP is a new combination of bariatric techniques which introduce gastric placation the new simple but yet very effective diversion component which is replacing the duodenal switch and other difficult diversion modalities. Gastric placation is also considered a new territory in bariatric operations and it combination with malasorbative component is rarely done so we try to explore this area and to reach the best results for our patients.
Keywords
Morbid obesity; Surgery; Biliopancreatic diversion; Doudenal switch; Single Anastomosis; Sleeve gastrectomy; Metabolic surgery; SAGI-PGP; Gastric plication; SADI-S; Laparoscopic sleeve gastrectomy; Roux-en-Y gastric bypass
Introduction
Bariatric operations are still new science that need to be explored extensively and to be practiced excessively so that we can reach to the best required results and the least complications and morbidities that we could face with such elective surgeries although it should not be considered elective when it can improve and prevent the all possible health related problems associated with morbid obesity and metabolic syndrome but since it is a new science it need more thorough analysis and flexible changing in its regulation based on trail and error. Our team in soran private hospital in Erbil, Iraq had about five year experience in all the classic bariatric operations. Along the years we try a lot of modalities such as laparoscopic sleeve gastrectomy (LSG) and laparoscopic adjustable gastric banding (LAGB). Nevertheless both of these operations are still considered very popular [1,2] but the results were never promising as the secondary failure rate was more than 50% of our patients and the complication such as leak from the sleeve side were catastrophic and it has lead to death of two of our patients. And for (LAGB) the primary and secondary failure were higher than those of LSG failure. A large number of patients undergo revision after LAGB. There is a well-known risk in conversion to LSG or Roux-en-Y gastric bypass (RYGB) in that the stapler may cut the scar on the stomach after band explantation, thus causing possible staple line instability [3]. Other consequences for the patients from a prolongation of the hospital stay to reoperations, gastric band slippage. In the long-term, complications might impair quality of life, leading us to question our work and to search for other solutions. In order to reduce the risk of gastric leak, Talebpour et al. developed laparoscopic gastric plication (LGP), also creating a sleeve-like stomach [4]. On the other hand, malabsorptive operations evolved from jejunoileal bypass (JIB) through biliopancreatic diversion (BPD) to combined, restrictive and malabsorptive procedures such as biliopancreatic diversion with duodenal switch (BPD-DS) or (SADI-S) [5].
The single- or one-anastomosis gastric bypass, perhaps better known under the somewhat misleading name, the “mini gastric bypass,” was introduced by Robert Rutledge [6] in 2001. This alternative in the field of metabolic surgery has gained increasing attention lately due to its simplicity and claimed safety and effectiveness [7]. However, there is much controversy surrounding this method, mainly concerning the possible harmful and in the long-term even carcinogenic effects of bile reflux in the gastric pouch [8,9].
The results of (LGP) were far better than those of (LSG), (LAGB) or Mini Gastric bypass the complication were far less but still it was not the ideal operation and it was consisting solely of the restrictive component which leads in one case to fundus sliding outside of suture row and blowout of dilated displaced fundus leading to fistula formation and death. Other complication is mentioned in the original study but we fortunately didn’t encounter it [10]. The main problem with LGP is the high intraluminal pressure and gastric edema which lead to fatal complications sometimes and hence our surgical team come to the idea of combining the LGP with other malasorbative component based on (BPD), in which only one anastmosis is performed and occlusion of the pylorus performed instead of (DS) to create this new technique which called Single Anastmosis Gastric Ileal bypass with Pyloric and Gastric Plication (SAGI-PGP) (Figure 1).
Methods and Patients
Patients with previous history of bariatric surgeries were excluded. We perform the operation as a two-surgeon procedure with the patient at a 30-degree reverse rendelenberg position. The surgeon stands between the patient’s legs with one assistant on the patient’s left side. After penetrating into the abdominal cavity with versus needle through the umbilicus, insufflation of carbon dioxide is commenced with a set point at 14 mmHg. Five or six ports incisions done in the classic way [10].
The epigastric region is exposed by lifting the left lobe of the liver with a liver retractor. The separation of the omentum from the greater curvature begins on the greater curvature at the body of the stomach till the fundus above and till the antrum below using the harmonic scalpel (Ultracision, Ethicon Endo-Surgery, Inc., Johnson & Johnson) till the bursa omentalis is entered then aLigaSure® vessel sealing device (Covidien, Dublin, Ireland), then occlusion of the pylorus with single three knots stitch of 00 coated polyester which can be done with minimal to no loss of blood (Figure 2).
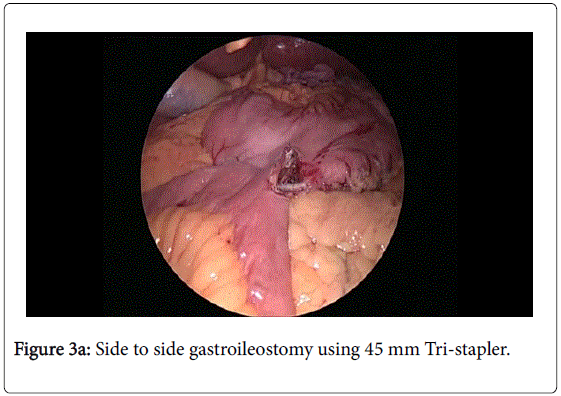
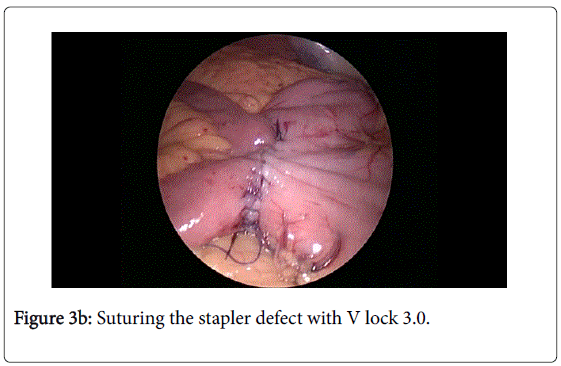
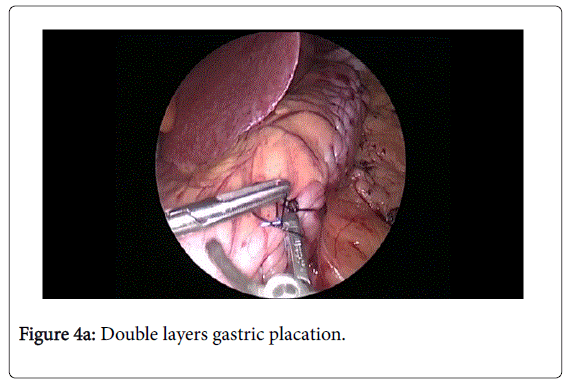
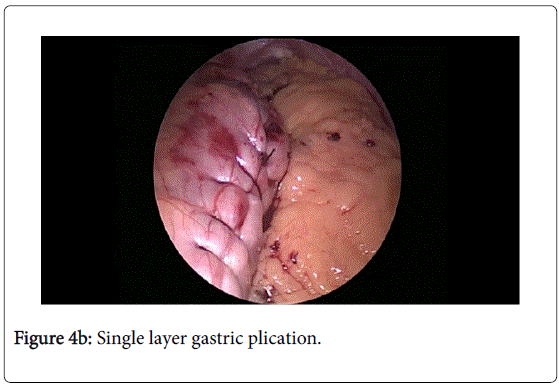
The ileocecal junction is identified and 250 cm is measured upward then we create side to side gastroileostomy using 45 mm Tri-stapler and suturing the stapler defect with V lock 3.0 (Figures 3a and 3b) followed by gastric plication above the fundus till before the gastojejunostomy site after inserting 54 French bougie using continuous coated 00 polyester suturing with the possibility of either single or double layer variation (Figures 4a and 4b). One drain is systematically left.
The gall bladder is not removed unless otherwise indicated [11]. The operation time is about 1:30 to 2 hours. Patients start drinking on the second postoperative day, and they are discharged on the third to the fourth postoperative day. Lower limb pneumatic compression, prophylactic heparin, and antibiotic therapy were advised in all cases.
The usual dietary regimen of metabolic surgery is administered with emphasis on early mobilization and lifestyle modification [12]. Barium meal was done for the first twenty patients showing no leak and complete occlusion of the pylorus.
Results
The mean BMI of patients is 43.5 kg/m2 with female patient were 165 and male patients were 105. Type 2 DM was presenting in 68 patients. Hypertension in 48 Hypercholesterolemia in 104, Hypertriglyceridemia in 178 and sleep apnea in 20, polycystic ovarian syndrome in 34 patients.
We were able to follow 240 patients of the 270 through at the first year, 230 in the second year and 200 in the third year. EWL is about 90% at year one, 85% at year 2 which is more excellent than what we expected and was maintained over 100% during the third postoperative year.
All diabetic patients return to normal blood sugar levels and the median glycemic level was 97. The patients who were on oral hypoglycemic drugs respond more dramatically and effectively than those who were on insulin therapy. No further anti-diabetic medications were required almost immediately after the operation with insulin prescribed only for 15 patients during their hospital stay (Table 1).
| Preoperative | Postoperative | |||||
|---|---|---|---|---|---|---|
| Mean | Range | Abnormal | Mean | Range | Abnormal | |
| Glucose (mg/dl) | 222 | 95-350 | 95 | 97 | 65-101 | 0 |
| HbA1ca % | 8.9 | 5.8-12 | 80 | 5.05 | 4.1-6 | 0 |
Table 1: Glycemic profiles. Comparison between pre and postoperative values of the diabetic patients.
No mortality seen in any patient till now. No intraoperative complications encounter us. Two patients presented with small perforation about 2 cm at the distal loop below anastomosis during the 4th and 7th month respectively. 3 patients presented with stomal ulceration at the site of anastomosis. They were treated conservatively.
Blood analysis was performed at the third month after surgery then after the sixth and then every year. Mild anemia seen in 10 patients the median range was 14.4 mg/dl. Mild protein deficiency seen in 7 patients in the 3rd month after operation and all of them returned to normal level in the second year with median range for protein in 7,3.
Moderate to severe vitamin D3 deficiency seen in all the patients responding very well to treatment. It was expected to see the Vitamin D3 deficiency in a lot numbers in our patients since vitamin D3 deficiency is endemic in our area [13].
53% of the patients especially the female patients undergo telogen effluvium usually at 4th to 6th and it returned to normal hair cycle at the end of the sixth month. No vitamin B12 or Vitamin A, E deficiency observed in our patients (Table 2).
| 1st year | 2nd year | 3rd year | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | Range | Abnormal | Mean | Range | Abnormal | Mean | Range | Abnormal | |
| Hemoglobin g/dl | 14.4 | 10.8–18 | 8.3 | 14 | 10.8-17.3 | 11 | 13.3 | 11.6-15 | 9 |
| Hematocrit (%) | 45 | 30–60 | 10 | 39.8 | 31.8-47.8 | 12 | 39.5 | 34.2-46.5 | 0 |
| Iron (μg/dl) | 89 | 28–150 | 18 | 96 | 32-160 | 9 | 99 | 33-165 | 6 |
| Proteins (g/dl) | 7.3 | 5.7–8.9 | 7 | 7 | 6.2-7.9 | 5 | 6.3 | 5.7-7.2 | 0 |
| 25-OH-Vitamin D3(ng/ml) | 6.5 | 3.5–11 | 240 | 74 | 25-34 | 80 | 48 | 27-79 | 5 |
| Vitamin B12 (pg/ml) | 820 | 140–1,500 | 4 | 385 | 13-6317 | 2 | 376.5 | 183-570 | 0 |
| Folic acid (ng/ml) | 7.7 | 1.3 – 12.8 | 16 | 10.25 | 1.5-19 | 12 | 8.25 | 1.6-14.9 | 9 |
| Calcium (mg/dl) | 8.7 | 7.2–10.2 | 6 | 9.8 | 8.5-11.1 | 0 | 10.25 | 10-10.5 | 0 |
Table 2: Post-operative hematological analysis.
6 patients developed gallstone in the 1st post-operative year however it was treated surgically. Diarrhea was infrequent and food relative and no complication associated with it. Not any patient complained of serious biliary reflux symptoms.
Discussion
SAGI PGP is a revolutionary new technique that is based on the biliopancreatic diversion (BPD) [14,15] and it is similar to single anastomosis duodenal ileal bypass with sleeve gastrectomy (SADI-S) but without DS and replacing the sleeve with Gastric Placation.
The reason for developing a new technique or for modifying a preexisting one was to simplify the procedure, to decrease the potential complication rate, and to maintain or even to improve, if possible, the outcomes of the original operation. The simplicity of this operation is exceeding a lot of its predecessors operations by far a lot and its results are astonishing with minimal complications that can be addressed to this operation.
Principles of biliopancreatic diversion (Biliopancreatic diversion was modified in the late 1980s by Douglass Hess [16] when he described an operation based both on Scopinaro’s procedure and on DeMeester’s duodenal switch [17]. The sleeve gastrectomy proposed by Hess had the potential benefit of the preservation of the gastric antrum and the pylorus; in this way, acid and intrinsic factor secretion would be maintained and so iron, calcium, vitamin B12 and protein absorption would be better than after a classical BPD without jeopardizing weight loss. These were theoretical advantages which have been scarcely, if ever, demonstrated in the clinical practice [18,19].
Since gastric plication eliminates the risk of a staple line leak or bleeding, this procedure seems a favorable alternative to conventional sleeve gastrectomy in case stapling the stomach is considered a high risk [15] and hence we replaced the sleeve with gastric placation.
To sum it up, advantages of LGP over other restrictive methods are as follows. First, the patient is independent postoperatively with easy follow up; which means the patient is free from any obligatory postoperative procedures e.g. balloon size regulation in gastric banding. No foreign body reaction is the next advantage of LGP as only two or three prolen or nylon threads are used with no use of mesh or band. Moreover, less cost due to no need for stapler or band and short period of postoperative hospitalization are very important factors for patients. Less complication such as leakage, infection or erosion should be noted since this method is the most conservative procedure among other bariatric surgeries with no resection or anastomosis. If needed, this method is reversible during first 6 weeks just by cutting the suture lines and easily releasing the mild adhesions [10].
The first modification was the replacement of DS with pyloric placation and thus reducing operative time greatly and minimizing the damage that can be inflicted on the duodenum. In DS the duodenum is divided in its first portion, leaving an approximately 2 cm length of duodenum intact beyond the pylorus. This end of the duodenum is then anastomosed to the distal 250 cm of ileum. This anastomosis is often done in an end-to-end fashion with a circular stapler. It is the most difficult portion of the DS procedure, and leak rates are slightly higher than with other anastomoses [20] so by replacing the DS with pyloric plication we are greatly simplifying the operation, also Reducing the number of intestinal anastomoses should have some advantages over previous procedures, i.e., less probability of postoperative leaks or anastomotic strictures, a decrease in the operative time and consequently less anesthetic derived complications, and as the mesentery is not opened, there should be a lower probability of postoperative obstructions.
So by combining these two modifications together in a single operation we are reaching to the best possible outcome that we could we think of and that it is possible to achieve.
Conclusion
SAGI PGP is groundbreaking new technique for reducing the excessive body weight and elimination of metabolic syndrome with the least complications postoperatively and less blood loss and minimal operative time compared to BPD-DS and to SADI-S Moreover, it is also more physiological and the operation can be modified and adjusted according to the medical condition, body mass index and patient’s desire and it is very cost effective operation; therefore, it should be considered absolutely as a standard procedure alongside other bariatric surgeries
References
- Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, et al.(2004) Bariatric surgery: asystematic review and meta-analysis. JAMA 292: 1724-1737.
- Buchwald H, Williams SE (2004) Bariatric surgery worldwide 2003. ObesSurg 14: 1157-1164.
- Gagner M, Gumbs AA (2007) Gastric banding: conversion to sleeve, bypass, or DS. SurgEndosc21: 1931-1935.
- Talebpour M, Amoli BS (2007) Laparoscopic total gastric vertical plication in morbid obesity. J LaparoendoscAdvSurg Tech 17: 793-798.
- Sánchez-Pernaute A, Herrera MA, Pérez-Aguirre ME, Talavera P, Cabrerizo L, et al. (2010) Single anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S). One to three-year follow-up. ObesSurg 20: 1720-1726.
- Rutledge R (2001) The mini-gastric bypass: Experience with the first 1,274 cases. ObesSurg 11: 276-280.
- Carbajo M, García-Caballero M, Toledano M, Osorio D, García-Lanza C, et al. (2005) One-anastomosis gastric bypass by laparoscopy: Results of the first 209 patients. ObesSurg 15:398-404.
- Fisher BL, Buchwald H, Clark W (2005) Mini-gastric bypass controversy. ObesSurg 11: 773-777.
- Johnson WH, Fernanadez AZ, Farrell TM, Macdonald KG, Grant JP, et al. (2007) Surgical revision of loop (“Mini”) gastric bypass procedure: Multicenter review of complications and conversions to Roux-en-Y gastric bypass. SurgObesRelat Dis 3:37-41.
- Talebpour M, Motamedi SM, Talebpour A, Vahidi H (2012) Twelve year experience of laparoscopic gastric plication in morbid obesity: development of the technique and patient outcomes. Ann SurgInnov Res 6: 7.
- Tsirline VB, Keilani ZM, El Djouzi S, Phillips RC, Kuwada TS, et al. (2014) How frequently and when do patients undergo cholecystectomy after bariatric surgery?SurgObesRelat Dis 10: 313-321.
- Integrated Health Nutritional Guidelines (ASMBS).
- Naeem Z (2010) Vitamin D Deficiency-An Ignored Epidemic. Int J Health Sci (Qassim) 4: V–VI.
- Scopinaro N, Gianetta E, Civalleri D, Bonalumi U, Bachi V (1979) Bilio-pancreatic bypass for obesity: I. An experimental study in dogs. Br J Surg66:613-617.
- Scopinaro N (2006)Biliopancreaticdiversión: mechanisms of action and long-term results. ObesSurg 16:683-689.
- Hess DS, Hess DWS (1998) Biliopancreatic diversion with a duodenal switch. ObesSurg 8: 267-282.
- DeMeester TR, Fuchs KH, Ball CS, Albertucci M, Smyrk TC, et al. Experimental and clinical results with proximal end-to-end duodenojejunostomy for pathologic duodenogastric reflux. Ann Surg206: 414-424.
- Dolan K, Hatzifotis M, Newbury L (2004) A clinical and nutritional comparison of biliopancreatic diversion with and without duodenal switch. Ann Surg 240: 51-56.
- Marceau P, Biron S, Hould FS, Lebel S, Marceau S, et al. (2009) Duodenal switch improved standard biliopancreatic diversion: a retrospective study. SurgObesRelat Dis 5: 43-44.
- Schauer PR, Schirmer B (2009) The Surgical mangement of obesity schwartz principles of General Surgery.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 14518
- [From(publication date):
August-2016 - Apr 07, 2025] - Breakdown by view type
- HTML page views : 13575
- PDF downloads : 943