Silent Myocardial Infarction and Diabetic Cardiovascular Renal Dysfunctions in young Women Age 32: Case Report and Literature
Received: 01-Jan-2018 / Accepted Date: 09-Jan-2018 / Published Date: 17-Jan-2018
Abstract
Diabetes Mellitus (DM) as ominous presumptive diagnostic of chronic kidney disease (CKD) worsening to endstage renal damage (ESRD) is one of the spontaneous elicit in general health affair. The longstanding diabetes in young ages firmly evokes the exceptional cardiovascular risk factors manifestation and the initiative progression of diabetic micro angiopathies and macro angiopathies. The latent pathophysiological mechanisms are strongly provocative of chronic heart failure and myocardial infarction by the potential contributor of hyperglycemia in the hemodynamic derangements confounding to the natural history of diabetes with vulnerable silent symptoms.
Keywords: Coronary heart disease; ST elevation; Myocardial infarction; Diabetic nephropathy, Chronic kidney disease, Risk of premature death
Introduction
Cardiovascular disease represents the frequent leading cause of global death affecting the young population worldwide [1]. At clinical entity silent MI annually experience CHD with the approximate of 9.8 million per year predicting the unrecognized symptoms related to the occurrence of either ambulatory myocardial ischemia or sudden death with 60-70% cases asymptomatically [2]. The kidney disease outcomes initiative on clinical practice guidelines proves the threshold of ischemic chest pain is a powerful venue of cardiovascular morbidity and all cause-mortality [3] with the classification of hemo dynamic modifications independently estimate glomerular filtration rate (eGFR) in the scheme of arbitrary renal stages altering albuminuria, glomerular hyperfiltration and hyperglycemia in renal damage. Consequently CKD as a clinical syndrome equivalent to CHD investigate the urinary excretion proteins and TGF-beta 1 initially in nephropathy as a diagnostic value in clinical parameters of previous MI in diabetic individuals [4].
In the Framingham heart study, the estimation of silent ischemia detection on large scale misinterpret by atypical angina following normal ECG in the undetectable prevalence of general population <45 years young men and women including the illness of metabolic impairments, eGFR fall, advanced CKD on dialysis, chronic inflammations and prothrombic complications in the acceptable clinical autopsy studies [5]. Additionally diabetic kidney disease progress with the albuminuria status and serum creatinine measurements on screening at initial conventional method in pubertal diabetic interval challenging hyperglycemia on clinical nephropathy [6].
According to the Epidemiological studies, poor prognosis of CHD in CKD cases at less ratios make the diagnostic differences by the interpretation of ECG changes, risk factor profiles, pain perception, cardiac biomarkers and MI perfusions evaluation in the objective of stable angina culminate the presentation of constant changes in troponin values presenting the attributes of premature CHD with the conclusion of progressive atheromatous plaques and calcifications on the likelihood of sepsis, anemia, platelet aggressiveness, nitric oxide abnormal metabolism, arterial stiffness, calcium-phosphate homeostasis, endothelial dysfunctions, recreational drugs, history of multiple traumas and surgeries. Classically, we present the case of inferior MI in young women with type 2 diabetes evolutions of 10 years and previous heart failure risk to death prolonging the complications of dyslipidemia progress to the advancement of diabetic nephropathy accelerating membrano-proliferative glomerulonephritis.
Case Presentation
A 32 year old female present to Emergency Department with severe chest pain, palpitation and vomiting for 3 days. She has been diagnosed with the previous episodes of heart failure and traditional risk factors of CAD in medical history. She described her chest pain with tightedness and flank dull pain at both the areas of kidneys with back pain.
On physical examination, Cardiac sounds were normal on auscultation with no tenderness on palpation, no intra-abdominal rebound masses, no neck stiffness, no jugular vein enlargement, no dysmenorrhea, no clubbing, no family history of CAD and no hypertension. She was profound sweating on presence with weight loss, urine retention, fatigability and restlessness from 1 week. Her medications at the time of review include Aspirin, Statin, Metformin, Insulin, Diuretics and Omeprazole.
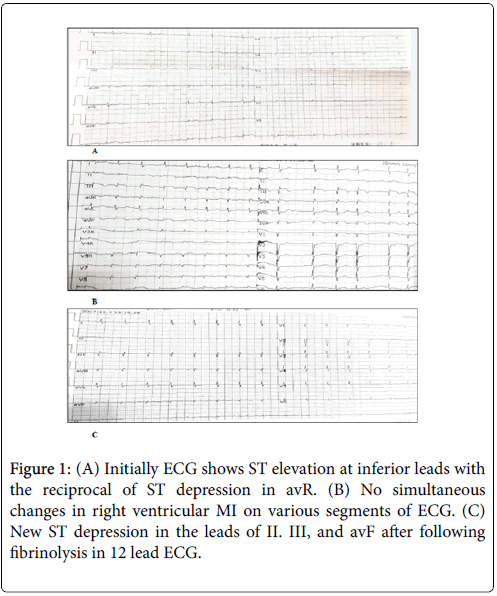
At Admission, BP was 85/60 mmHg and her heart rates 66 bpm. ECG showed normal sinus rhythm with ST elevation in leads II, III and avf with the reciprocal of ST segment depression in leads V1-V6 (Figure 1A). The crucial step for ruling out myocardial injury, clinical diagnosis begins with the measurement of cardiac enzymes (Table 1). Moreover on the primary assessment of troponin elevation and NTproBNP impairment assess the specificity and sensitivity limitations on trans-thoracic echocardiography revealing hypokinesia with an LVEF of 48% motion index on homogenous contrast reflecting MI tension on inferior wall suspecting intracardiac thrombosis and pulmonary embolism.
| DAYS | CK-MB | MYO | cTnI | Glu | NT-ProBNP |
|---|---|---|---|---|---|
| Admission | 13.66 ng/mL (0-5) | 122.63 U g/L (0-110) | 27.16 ng/mL (0-0.78) | 15.60 mm/L (3.5-6.1) | 4302.00 pg/mL |
| Day 2 | 8.45 ng/mL (0-5) | 72.43 U g/L (0-110) | 21.45 ng/mL (0-0.78) | 17.16 mm/L (3.5-6.1) | 11380.00 pg/mL |
| Day 4 | 2.73 ng/mL (0-5) | 63 U g/L (0-110) | 18.46 ng/mL (0-0.78) | 15.05 mm/L (3.5-6.1) | 15030.00 pg/mL |
| Day 6 | 1.42 ng/mL (0-5) | 47.05 U g/L (0-110) | 2.54 ng/mL (0-0.78) | 10.15 mm/L (3.5-6.1) | 9002.00 pg/mL |
| Day 8 | 1.31 ng/mL (0-5) | 39.43 U g/L (0-110) | 0.67 ng/mL (0-0.78) | 10.03 mm/L (3.5-6.1) | 289200 pg/mL |
Table 1: Clinical values of Combined Detection of 5 Indicators in the Diagnosis of Acute MI.
In the suspection of fibrinolysis and thrombo embolism, thoracic ultrasonography TUS certainly performed prior to the normal chest imaging previously and false positive predictive value in D-dimer test (Table 2). On the emergency based history of angina, bilateral thoracic probe examine the presence of the left sided non-specific pleural lesion of more than 5 mm on screening. It provokes the follow up of thrombolytic with the association of hypotension. Therefore, anticoagulation includes low-molecular- weight heparin therapy (LMWH) and tPA produce successful reperfusion within 12 h noninvasively.
| Lab test | Result | Standard range | Significance |
|---|---|---|---|
| PT | 11.10 sec | (9-13) sec | Normal |
| APTT | 28.20 sec | (20-40) sec | Normal |
| Fibrinogen | 5.31 g/L | (2-4) ng/mL | Elevated |
| TAT | 53.60 ng/mL | (0-4) ng/mL | Elevated |
| D-dimer | 1.91 mg/L | (0-0.55) mg/L | Elevated |
Table 2: Quantitative D-dimer Assay for Pulmonary Embolism Diagnostic Test.
In regards with Gastrointestinal aspects, the alarming signs of dehydration, nausea, vomiting, fatigue and back pain warrant the examination of a comprehensive metabolic panel and amylase, lipase testing for the consideration of gastroenteritis or acute pancreatitis. The normal values result self-limiting bacterial infections by the management of fluid replacement, Calcitonin and supportive care.
As the patient on type 2 diabetes expansion on clinical estimation follow urinalysis on palpation of the bladder and oliguria. According to the quantitative measurements on total protein positive test, the exercising ECG reviewed on high standards verify the reciprocal changes in pathologic Q waves and hyper acute T waves in nonfatal angina attack reflect preload independently as shown in Figure 1B Apart from the renal profile, further globulin tests were progressed on the basis of laboratory evidences as shown in Tables 3 and 4 decline in eGFR, leucocytosis and elevated cholesterol conclude the pathogenesis of contrast induced nephropathy in association of nephrotoxic drugs eliminating the advanced staging of kidney damage other than glomerulonephritis and residual renal dysfunctions.
| Lab test | Result value | Standard range | Significance |
|---|---|---|---|
| ALB | 22.72 g/L | 40-55 g/L | Low |
| GLB | 19.13 /L | 20-40 g/L | Low |
| Urea | 13.80 mmol/L | 2.6-7.5 mmol/L | High |
| Creatinine | 78U mmol/L | 41-73 mmol/L | High |
| K | 5.74 mmol/L | 3.5-5.3 mmol/L | High |
| Na | 134 mmol/L | 137-147 mmol/L | Low |
| Cl | 106.00 mmol/L | 99-110 mmol/L | Normal |
| Ca (adj) | 3.20 mmol/L | 2.10-2.37 mmol/L | CKD |
| Mg | 0.66 mmol/L | 0.75-1.02 mmol/L | Low |
| eGFR | 117.40 mL/min | >90 mL/min | High |
Table 3: Comprehensive Metabolic Panel with eGFR Blood Test.
| Laboratory test | Result values | Reference range |
|---|---|---|
| WBC | 14.9610^7 /L | 3.5-9.5 /L |
| PLT | 413.00 x 10^9 /L | 125-350 /L |
| AST | 45.00 U/L | 13-35U /L |
| LDL-Ch | 5.04 mmol/L | 1.9-3.1 /L |
| TG | 8.11 mmol/L | 3.1-5.2 /L |
| Hb | 136.00 g/L | 115-150 g/L |
| Hct | 13% | 37-48% |
| Glu | 15.60 mmol/L | 3.5-6.1 mml/L |
| TP | 41.90 Ug/L | 65-85U g/L |
Table 4: Complete Blood Count Test Results.
On the basis of ANA negative investigation, monoclonal immunoglobulin IgG determines the pre-malignancy in renal insufficiency with plasmapheresis at high risk of multiple myelomas (Table 5). Here in the diagnosis of proteinuria and myeloma related diseases, Bence Jones test reveal false negative results in concentrated urine. At result, vitamin K status in CKD sub clinically link to the formation of arterial calcification in the high moderations of atherosclerosis constitute the notable limitations on independent peritoneal dialysis to maintain the equivalent nutrition at the less comorbidity of young age in CKD.
| Fractions | % | Reference % |
| Albumin | 34.1 | (48.1-59.5) |
| Alpha | 5.5 | (2.3-4.9) |
| Alpha 2 | 19.7 | (6.9-13.0) |
| Beta | 20.6 | (13.8-19.7) |
| Gamma | 20.1 | (10.1-21.9) |
Table 5: Serum Protein Electrophoresis to diagnose M protein.
Treatment
Management is initiative with the long-lasting insulin therapy in type 2 diabetes with the combination of Sulfonylurea and Metformin to control hyperglycemia. Secondly use of diuretics to restore electrolyte imbalance and Vitamin C for the nauseate feeling. Thirdly Diazepam orally for the anxiety and cardiac therapy Cedilanid for hemodynamic stability, Dopamine hydrochloride for improving the cardiac functions, Hydroxylamine and MgSO4 to control frequent arrhythmias, Clopidogrel 150 mg + Aspirin 100 mg with heparin therapy of LMWH in the preventions of heart failure and recurrent myocardial infarction. Lastly IV Sodium bicarbonate+ insulin+ 50% Dextrose for hyperkalemia and Atorvastatin of 20 mg oral/day for LDL reduction.
On the Ninth day, ECG changes (Figure 1C), ST resolution and T wave inversion after the pharmaceutical drugs. Additionally Calcium gluconate for cardiac improvement on stable renal function and timely dialysis may be required on renal failure and severity of hypermagnesemia. Lately the IV human albumin infusion as a therapeutic plasmapheresis in the indication of hypovolemic shock.
Discussion
The DIAD (Ischemia detection in asymptomatic Diabetics) [5,7] assumes the importance of greater incidence in long standing type 2 diabetes mellitus focus on the factor of occlusion in arteries on the possibility of judicious analyses with no support of scientific data in the management of anti-ischemic medications at frequent CAD cases. Hence, the investigations of massive consequences intermediate undoubtedly on clinical scoring as addressed for the issue of positive prognostic screening program in the upcoming studies. American Diabetes Association (ADA) recommend the measures of Beta blockers or re-vascularization medical therapy on aggressive intensive treated cases on investigating the annual review of abnormal resting ECG with the lesser degrees of ischemia intervention can improve the prognosis on cardiovascular events. The nontraditional factors of hyper coagulation and clotting mediators [8] pronounce the elevation of high risk on thrombic events statistically with the complications of CKD underlying the unclear etiology predominantly result congestive heart failure, ESRD, hemorrhagic stroke and relative risk of peripheral artery disease proportional to sudden cardiac death. Thus, an appropriate medical therapeutic management needed in terms of risk factors incidental preventions in adult onset diabetes [9].
In primary prevention study at Helsinki Heart Study [10] show poor outcomes in Diabetic individuals with CHD identifying high risk of aggressiveness in dyslipidemia treatment for the maintenance of LDL and Total protein target the statin drugs as a pharmacological intervention for the trials as a first choice in young diabetic nephropathy patients. The General Practice Research thrombosis Prevention trial [11] on the secondary prevention confirm the benefit of Aspirin treatment in the establishment of atherosclerotic disease in prospective trials reduced the risk of CHD and non-fatal events on the clinical recommendation of anti-platelet therapy can also be used as a preventive strategy to overt the nephropathy in <30 years age individuals. Therefore large phase prospective studies and trials are required to explain the issues of uncertain protein restriction in the adherence of management in routine setting care in diabetic nephropathy.
Observational Studies in the demonstration of direct effect on CVD risk factors deteriorate the kidney functions in hyperglycemia. The Reduction of End points in Non-insulin-dependent Diabetes with the Angiotensin II Antagonist Losartan (RENAAL) and Irbesartan Diabetic Nephropathy Trial (IDNT) studies include the trial of Losartan and Iresartan as a renoprotective in the combination of Ramipril and Telmisartan initiate the defensive effect on proteinuria as compared to the therapy of (VA NEPHRON-D) study of Losartan and Lisinopril on macroalbuminuria >300 mg/day. Thus, the supportive directions on definite limitations of safety concerns utilize the consideration of Renin Angiotensin Aldosteron System (RAAS) lessens micoalbuminuria 30-300 mg/day in normic diabetes cases [12].
Hyperglycemia as a therapeutic potent in diabetes, the epidemiological early analysis illustrate the fundamental controversy of minimal outcomes in macrovascular hazards can ascend the occasion of CVD risk factors, extravagant mortality rates and vigorous symptoms with the median of HbA1c%. The Action in Controlling Cardiac Risk factors in Diabetes (ACCORD) present the current affirmation of delaying vascular complications related to the consequences of CKD staging 3-4 can be patently achieved by the optimal goal of HbA1c and hypoglycemia incidents. Accordingly, a tight control on hyperglycemia is permeable to convert the high risk of hyperfiltration and glomerular hypertrophy partially on HbA1c <7% and apparent supremacy to control the normal ranges with the treatment of insulin in the maintenance of proteinuria on reduced value.
According to the American Heart Association guidelines, the pharmacotherapy in CKD associated with CVD risk factors include the counsel use of Fibrinolytic, Antiplatelet, Glycoprotein II b/III a receptor antagonist, Anti-coagulants, Beta blockers, ACEIs/ARBs, Aldosterone blocker and Statin can assess the randomized controlled trials of efficacy and welfare to diminish the vascular events in nonchronic dialysis patients. The another Study of Heart and Renal Protection (SHARP) involve the substantial results in combined therapy composite to the dominance in controlling the major atherosclerotic relative risks, intracranial hemorrhage, left ventricular hypertrophy and STEMI intimated the remarkable decline in hospital death and sudden cardiac arrest for least 1 year. Ultimately, pharmacokinetic studies in renal dysfunction require essential regulations for the clinical controlled trials further on extensive population with distinct precise dosing in terminating the predictable adverse outcome pathways.
References
- Department of Health (2000) National Service Framework for Coronary Heart Disease.
- Oberman A, Kouchoukos NT, Holt JH, Russell RO (1977) Long-term results of the medical treatment of coronary artery disease. Angiology 28: 160-168.
- Nesto RW, Phillips RT, Kett KG, Hill T, Perper E, et al. (1988) Angina and exertional myocardial ischemia in diabetic and nondiabetic patients: assessment by exercise thallium scintigraphy. Ann Intern Med 108: 170-175.
- Ishii H, Jirousek MR, Koya D, Tagaki C, Xia P, et al. (1996) Amelioration of vascular dysfunction in diabetic rats by an oral PKC inhibitor. Science 272 : 728-731.
- Kannel WB, Abbott RD (1984) Incidence and prognosis of unrecognized myocardial infarction. An update on the Framingham study. N Engl J Med 311: 1144-1147.
- American Diabetes Association (2004) Nephropathy in diabetes. Diabetes Care 27: S79-83.
- Bansal S, Wackers FJT, Inzucchi SE, Chyun DA, Davey JA, et al. (2011) Five-year outcomes in high-risk participants in the Detection of Ischemia in Asymptomatic Diabetics (DIAD) study: a post hoc analysis. Diabetes Care 34: 204-209.
- Baber U, Bander J, Karajgikar R, Yadav K, Hadi A, et al. (2013) Combined and independent impact of diabetes mellitus and chronic kidney disease on residual platelet reactivity. Thromb Haemost 110: 118-123.
- Seshasai SR, Kaptoge S, Thompson A, Di Angelantonio E, Gao P, et al. (2011) Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med 364: 829-841.
- Koskinen P, Manttari M, Manninen V, Huttunenctk, Heinnonen OP, et al. (1992) Coronary heart disease incidence in NIDDM patients in the Helsinki Heart Study. Diabetes Care 15: 820-825.
- The Medical Research Council's General Practice Research Framework (1998) Thrombosis prevention trial: randomised trial of low-intensity oral anticoagulation with warfarin and low-dose aspirin in the primary prevention of ischaemic heart disease in men at increased risk. Lancet 351: 233-241.
- Hirst JA, Taylor KS, Stevens RJ, Blacklock CL, Roberts NW, et al. (2012) The impact of renin-angiotensin-aldosterone system inhibitors on Type 1 and Type 2 diabetic patients with and without early diabetic nephropathy. Kidney Int 81: 674-683.
Citation: Iftikhar HB (2018) Silent Myocardial Infarction and Diabetic Cardiovascular Renal Dysfunctions in young Women Age 32: Case Report and Literature. Atheroscler Open Access 3: 119.
Copyright: © 2018 Iftikhar HB. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Usage
- Total views: 3471
- [From(publication date): 0-2018 - Dec 20, 2024]
- Breakdown by view type
- HTML page views: 2801
- PDF downloads: 670