Siblings’ with Fatal Congenital Ichthyoses: A Case Report
Received: 06-Oct-2021 / Accepted Date: 20-Oct-2021 / Published Date: 27-Oct-2021 DOI: 10.4172/2572-4983.1000002
Abstract
Objective: Ichthyoses are cornification disorders in which irregular epidermal separation and desquamation result in a faulty epidermal membrane. Harlequin Ichthyoses (HI) is a rare and extreme type that led to neonatal death. It is caused by mutations in the ABCA12 gene, and the inheritance pattern is autosomal recessive. This case report contributes significantly to medical knowledge to suspect and diagnose similar patients.
Case report: We present a case of Harlequin Ichthyoses that is diagnosed postnatal by clinical review. Extreme ectropion, eclabium, and malformed ears are present in the neonate. As a result of Harlequin Ichthyoses complications, the neonate died. There is history of similar illness in previous sibling who died in neonatal age. The present study is the first to report two cases of fatal HI from successive pregnancies in the same woman who has consanguinity marriage.
Conclusion: The severe form of harlequin Ichthyoses is often lethal in the perinatal period, and it is commonly a product of consanguineous parents. Definitive diagnosis is essential for long-term management as well as counseling to the parents, if they are considering having children together.
Keywords: Harlequin ichthyoses; Consanguinity; Autosomal recessive
Introduction
The ichthyoses, also called disorders of keratinization or disorders of cornification, are a heterogeneous group of disorders characterized by a generalized scaling of the skin of varying severity. The great majority of ichthyoses are inherited [1].
Ichthyosis vulgaris and X-linked ichthyosis are the most common types of ichthyosis. Autosomal Recessive Congenital Ichthyosis (ARCI) is a heterogeneous group of nonsyndromic disorders of keratinization, which includes Lamellar Ichthyosis (LI), Congenital Ichthyosiform Erythroderma (CIE), and Harlequin Ichthyosis (HI) [2,3].
It is rare, and individual subtypes have an average population frequency of 1: 200000 individuals, except in areas where consanguinity is more common [4]. Early diagnosis is required for immediate management and prevention of fluid-electrolyte balance as well as prevention of secondary infections.
Definitive diagnosis is essential for long-term management as well as counseling to the parents of affected infant if they are considering having children together [5].
Case Presentation
We present a 39 hours old male neonate who is born from 22 years old Para II mother with full term gestation. The mother has ANC follow up only once. Maternal baseline investigation (VDRL, HBSAG, and HIV) are normal.
The delivery was via SVD at local health center with unknown Apgar score but cried immediately. Parents were in consanguinity (cousins), and they have similar condition of ichthyosis in the previous sibling, who was female neonate died at 4th day of life.
Physical examination revealed a newborn weighing 2.5 kilograms with tachypnea (69 breaths per minute), Subcostal, intercostal retraction and good bilateral air entry. The cardiovascular system was essentially normal with a heart rate of 160 per minute with the first and second heart sounds heard and no murmur.
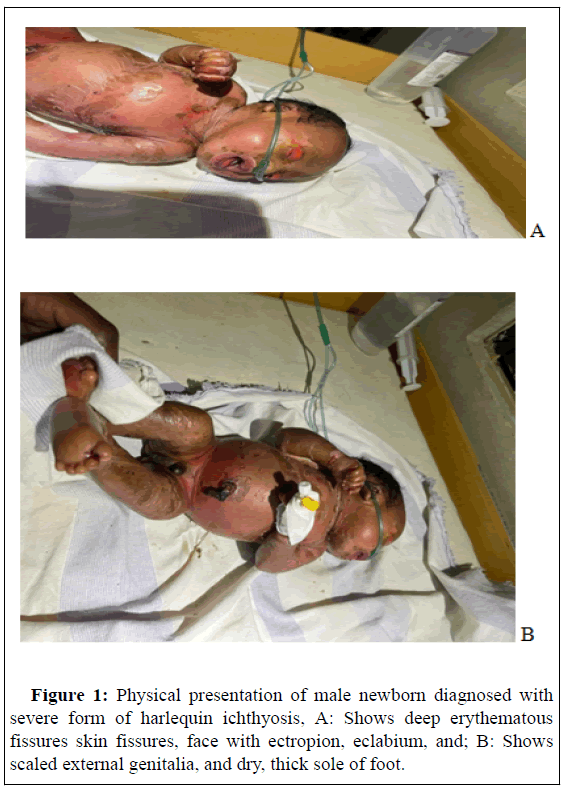
Abdominal examination was normal with no organomegally and a patent anus. The main clinical findings were on the skin as shown in the accompanying photographs of the infant (Figures 1A and 1B).
The baby was covered in a thick“leathery”skin interspersed with erythematous fissures more prominent in the areas of skin folds with tight skin on upper and lower extremities. There is eversion of the eyelids (ectropion).
In addition, the pinnae of the ears were mal formed. The mouth was taut and maintained in a persistently open position similar to a “fish mouth” with eversion of the lips (eclabion).
Treatment and outcome
The baby was evaluated by the pediatrician at NICU and the clinical diagnosis of harlequin ichthyoses was made. The family was counseled and the baby was admitted to the Neonatal Intensive Care Unit (NICU) where she was kept in an incubator. Although the baby had adequate sucking reflex, in order to prevent any incidence of aspiration, she was started with IV maintenance fluids, intravenous antibiotics and Continuous Positive Airway Pressure (CPAP) was delivered via Bubble-CPAP. Skin was cleaned with normal saline. Liquid paraffin and emollients were gently applied to the whole cutaneous surface every two hours. Antibacterial eye drops and sterilized cotton eye pads were applied. The baby developed respiratory distress within a few hours of birth, despite the supportive management. The baby died on the third day of life due to respiratory distress. The parents were psychologically supported, the disease spectrum was explained to them, and genetic counseling was recommended for future pregnancies.
Discussion
Ichthyoses are a very heterogeneous group of more than 20 diseases manifested by very dry, rough and scaling skin. They belong into a group of rare diseases-keratodermies. The extent and severity of the disease varies significantly from symptoms such as soft, peeling skin up to extensive generalized involvement, sometimes involving other organs apart from the skin as well [6,7]. The great majority of ichthyoses are inherited. Ichthyosis vulgaris and X-linked ichthyosis are the most common types of ichthyosis, with an estimated incidence of 1 in 250 births and 1:6000 male births, respectively [8,9].
Autosomal recessive congenital ichthyoses, which include lamellar ichthyosis, congenital ichthyosiform erythroderma, and harlequin ichthyosis. Of these disorders, HI is the most clinically distinct and genetically homogeneous entity, resulting from loss of function mutations in ABCA12. In contrast, LI and CIE represent a spectrum of disorders due to mutations in TGM1, ALOXE3, ALOX12B, NIPAL4, CYP4F22, ABCA12, PNPLA1, and other yet unidentified genes. No clear genotype-phenotype correlation has been possible in these disorders, since mutation in the same genes may present with widely divergent phenotypes [10].
Although we had no capacity to do genetic testing to determine the phenotype, the clinical presentation of this patient suggests a harlequin ichthyoses.
Babies born with harlequin ichthyoses present significant challenges to care providers in developing countries like ours that include unavailability of prenatal diagnostic tests, post-natal genetic tests, required drugs and counseling of the parents. Despite limited resources we were able to provide supportive care to the baby until its final moments. If resources allow, the parents were advised on close follow up upon the next pregnancy. This is the first reported case in Ethiopia.
Conclusion
Harlequin icthyoses is a rare genetic condition of the skin. Most cases were merged to meet on the same causative factor, the consanguinity. Genetic counseling, genetic screening, and prenatal diagnosis must be advised to susceptible parents to avoid recurrence of the condition especially in case of consanguinity. Supportive therapy remains the mainstay of management; however, these neonates do not have a very good prognosis.
Consent
Patient confidentiality has been maintained and written consent for the publication of patient details and clinical pictures have been obtained from the patient’s father and can be furnished when required.
References
- Oji V, Tadini G, Akiyama M (2010) Revised nomenclature and classification of inherited ichthyoses: Results of the first ichthyosis consensus conference in Sorèze 2009. J Am Acad Dermatol 63: 607.
- Hernández-MartÃn A, González-Sarmiento R, De Unamuno P (1999) X-linked ichthyosis: An update. Br J Dermatol 141:617.
- Wells RS, Kerr CB (1966) Clinical features of autosomal dominant and sex-linked ichthyosis in an English population. Br Med J 1:947.
- Bale SJ, Richard G (1993) Autosomal recessive congenital ichthyosis. Neonatal Netw 18:37-46.
- Akcakus M, Gunes T, Kurtoglu S, Ozturk A (2003) Collodion baby associated with asymmetric crying facies: A case report. Pediatr Dermatol 20: 134-136.
- Ak iyama M, Shimizu H (2008) An update on molecular aspects of the non-syndromic ichthyoses. Exp Dermatol. 17: 371-82.
- Colacchio K, Deng Y, NorthrupV, Bizarro MJ (2012) Complications associated with central and non-central venous catheters in a neonatal intensive care unit. J Perinatol 32:941-6.
- Nadroo Am, Glass RB, Lin J, Green RS, Holzman IR (2002). Changes in upper extremity position cause migration of peripherally inserted central catheters in neonates. Pediatrics 110:131-6.
- Newberry DM, Young TE, Robertson T, Levy J, Brandon D(2014) Evaluation of neonatal peripherally inserted central catheter tip movement in a consistent upper extremity position. Advances in Neonatal Care 14:61-8.
- RodrÃguez-Pazos L, Ginarte M, Vega A, Toribio J (2013) Autosomal recessive congenital ichthyosis. Actas Dermosifiliogr 104:270.
Citation: Yinges S (2021) Siblings’ with Fatal Congenital Ichthyoses: A Case Report. Neonat Pediatr Med S9:002. DOI: 10.4172/2572-4983.1000002
Copyright: © 2021 Yinges S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Conferences
42nd Global Conference on Nursing Care & Patient Safety
Toronto, CanadaRecommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3672
- [From(publication date): 0-2021 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 2926
- PDF downloads: 746