Research Article Open Access
Short-term Survival and Morbidity of Extremely premature Infants Born between 20 Weeks and 24 Weeks+6 Days Gestation
Souhail Alouini1*, Rasonandrianina Bienvenue Solange1, Anna Ramos1, Nabil Ayass2 and Rado Randriamboavonjy31Department of Obstetrics and Gynaecology, Regional Hospital Center of Orleans, France
2Department of Resuscitation and Neonatal Medicine, Regional Hospital Center of Orleans, France
3Department of Statistics of University hospital Center Befelatanana, Antananarivo, Madagascar
- *Corresponding Author:
- Souhail Alouini
Department of Obstetrics and Gynaecology
Regional Hospital Center of Orleans
France
Tel: +33688395759
E-mail: alouini.s@orange.fr
Received date: March 23, 2017; Accepted date: April 03, 2017; Published date: April 08, 2017
Citation: Alouini S, Solange RB, Ramos A, Ayass N, Randriamboavonjy R (2017) Short-term Survival and Morbidity of Extremely premature Infants Born between 20 Weeks and 24 Weeks+6 Days Gestation. J Preg Child Health 4:311. doi:10.4172/2376-127X.1000311
Copyright: © 2017 Alouini S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Pregnancy and Child Health
Abstract
Objective: To evaluate the morbidity and mortality of extremely premature infants (EPIs) born between 20 weeks and 24 weeks+6 days gestation at hospital discharge. Methods: This was a retrospective study that included all extremely preterm births between 2006 and 2012 at a tertiary maternity care centre with a neonatal intensive care unit. Results: Seventy-eight EPIs were born during the study period out of 30,000 deliveries (0.26%). Thirty-nine EPIs (50%) survived and had a mean length of hospital stay of 43 days. The mean weight of EPIs was 723 ± 179 g. The rate of survival of EPIs increases with gestational age. Forty-nine EPIs (62%) exhibited neonatal respiratory distress (NNRD), which evolved into a bronchopulmonary dysplasia in 28 cases (35%); 33 EPIs (42%) had a maternofetal infection, while 20 (26%) experienced ventricular hemorrhage. Ten EPI (13%) displayed enterocolitis and 17 (22%) had retinopathy. No EPIs born before 22 weeks gestation survived Twenty-four EPIs left the hospital with their mothers after being scheduled for a routine paediatric follow-up visit and 15 were transferred to another hospital: 10 for surgical treatment of patent ductus arteriosus and 5 to be closer to their mothers. Conclusion: The survival rates of EPIs between 20 and 24 weeks of gestation are high. NNRD, infections, and neurological and retinal complications were the main causes of morbidity. The results of this active management study of extremely preterm births were satisfactory at the short follow-up visits. Antenatal corticosteroids and magnesium sulfate administration should be discussed beginning at 22 weeks of gestation.
Keywords
Extremely premature infants; Bronchopulmonary dysplasia; Ventricular haemorrhage retinopathy; Maternal foetal infection.
Introduction
Over the past several years, advancements in antenatal and neonatal care have improved the survival rates of extremely premature infants (EPIs) with increasingly low gestational ages [1]. However, obstetrical and paediatric teams are regularly faced with technical and ethical problems regarding the resuscitation of infants at the limits of viability. The gestational age or fetal weight at which antenatal care and neonatal resuscitation should be initiated continues to change [2,3]. The main goal for these EPIs is to ensure a viable infant without severe neurological handicaps.
The frequency of EPIs born at less than 27 weeks gestation (WG) varies between 0.3 and 0.7% [4-6]. The mortality and morbidity rates are high for babies of extremely premature gestational age both in the short and long term. In some cases, their survival is complicated by severe neurological handicaps [7]. Some studies have shown that the morbidity and mortality of EPIs increase as their gestational age decreases [8]. There is debate concerning neonatal resuscitation of EPIs with gestational ages between 22 and 24 WG. Some obstetrical and paediatric teams limit neonatal resuscitation to palliative care before 24 weeks [9,10]. However, in practice, the results of neonatal resuscitation of EPIs are sometimes unpredictable but are often solicited at the parent’s request even when the prognosis seems poor.
Because we are confronted regularly by the birth of EPIs, we conducted a study in our maternity ward to evaluate the health status and short-term morbidity and mortality of EPIs born between 20 WG and 24 weeks and 6 days gestation.
Methods
We carried out a retrospective study that included all extremely premature births of 20 weeks to 24 weeks+5 days gestation between 1 January 2006 and 31 December 2012 in the maternity ward of the Regional Hospital Center of Orleans. This is a level 3 maternity care facility that offers neonatal reanimation.
Fetal deaths in utero, abortion for fetal abnormalities or incomplete charts were excluded from the study. The data were anonymously collected from the patients’ medical records. An anonymous number was assigned to each chart. In cases with a threat of premature birth (TPB), maternal investigations including a hemogram, a C-reactive protein (CRP), a vaginal swab for bacteria a bacteriological exam of the urine, and an ultrasound exam of the cervix were performed. The fetus also was examined using ultrasound. The beginning of the pregnancy was calculated from the start of the mother’s last menstrual period and the crown length was measured by pelvic ultrasonography during the first trimester of pregnancy.
Exclusion criteria concerned fetuses with imprecise gestational ages, fetal deaths in utero, abortion for fetal abnormalities, and incomplete charts. A tocolysis with Atosiban or calcic inhibitors was administered in the absence of contraindications. Antibiotics were also given when there was suspicion of fetomaternal infection. A corticosteroid treatment was discussed according to the gestational age, fetal weight and prognosis.
We collected the following general characteristics of the studied population: maternal age, body-mass index (BMI), parity, number of fetuses, and any pathologies of the pregnancy. We also gathered information regarding maternal and fetal treatments and the mode of delivery.
In the new-borns, we also studied the presentation before delivery, the weight, the sex, Apgar score and the umbilical arterial cord pH at birth. Neonatal resuscitation and duration of hospitalization were reported as well as the results of new-born exams (lab exams, ultrasonographic exams, cerebral magnetic resonance imaging (MRI), ophthalmoscopic examination, and electro-encephalogram). Followup included short-term well-being, mortality, and morbidity. The collection and analysis of the data were realized using R, version 2.11.1 (2010-05-31). As this was an anonymous retrospective study on charts, no consent procedures were required from individual patients.
Results
This study investigated 164 EPIs delivered from 1 January 2006 to 31 December 2012. Maternal characteristics of EPIs (Table 1). The mean maternal age was of 27 ± 6 years. Most women were multiparous. Twenty per cent of pregnancies were twin pregnancies. Twenty-eight pregnant women (35,9%) had an in utero transfer.
| n patients | Rate (%) | Mean ± SD | |
|---|---|---|---|
| Age (years) | 27.4 ± 5.7 | ||
| <20 | 8 | 10.26 | |
| [20âÂ?Â?30] | 46 | 58.92 | |
| [30âÂ?Â?40] | 21 | 26.92 | |
| = 40 | 3 | 3.85 | |
| Parity | |||
| Primiparous | 31 | 39.74 | |
| Multiparous | 45 | 59.85 | |
| BMI | 25.72 ± 6.58 | ||
| BMI<18 | 5 | 6.41 | |
| BMI 18âÂ?Â?25 | 45 | 57.89 | |
| BMI = 25 | 28 | 35.9 | |
| Twin pregnancies | 15 | 19.23 | |
| Rate of caesarean section | 20 | 25.64 |
Table 1: General characteristics of mothers (BMI=Body Mass Index; SD=Standard Deviation).
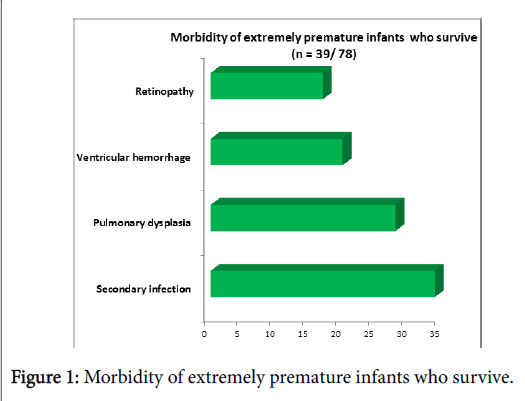
Table 1 shows the maternal characteristics of women who experienced extremely premature birth. Among the maternal pathologies that caused the premature birth, 14 involved a premature rupture of the membranes complicated by chorioamnionitis and 11 had vasculo placental or hypertensive disorders. Stuck twin syndrome was diagnosed in 4 cases; while 3 had gestational diabetes and 1 presented with placenta prevail. In all other cases, no etiology of the premature birth was found. The results concerning findings of EPIs are summarized in Tables 2 and 3 (Figure 1).
| n new-borns | Rate (%) | Mean ± Standard deviation | |
|---|---|---|---|
| Birth weight (g) | -78 | 723 ± 179 | |
| <500 | 10 | 13 | |
| [500âÂ?Â?800] | 39 | 50 | |
| = 800 | 29 | 37 | |
| Female | 28 | 36 | |
| Male | 50 | 64 | |
| Apgar<7 at 1 min | 69 | 88 | 4 ± 3 |
| Apgar<7 at 5 min | 60 | 5 ± 4 | |
| Umbilical artery cord pH | 45 | 58 | 7.26 ± 0.13 |
| pH>7.16 | 29 | ||
| pH<7.05 | 4 | ||
| 7.05<pH<7.16 | 12 | ||
| Neonatal intensive care | 56 | 72 | |
| Hospitalization duration (days) | 42 ± 52 | ||
| <20 | 42 | 54 | |
| [20âÂ?Â?50] | 8 | 10 | |
| [50âÂ?Â?100] | 14 | 18 | |
| = 100 | 14 | 18 | |
| Survival | 39 | 50 | |
| Mortality | 39 | 50 |
Table 2: Characteristics of EPIs born between 20 WG and 24 weeks +6 days (n=78).
| 20âÂ?Â?20+6 WG | 21âÂ?Â?21+6 WG | 22âÂ?Â?22+6 WG | 23âÂ?Â?23+6WG | 24âÂ?Â?24+6 WG | |
|---|---|---|---|---|---|
| (n=10) | (n=7) | (n=15) | (n=20) | (n=26) | |
| No corticosteroids | |||||
| Pulmonary dysplasia (n=28) | 0 | 0 | 6 (40%) | 10 (50%) | 12 (46%) |
| Secondary infection (n=34) | 0 | 0 | 8 (53%) | 11 (55%) | 15 (58%) |
| Ventricular hemorrhage (n=20) | 0 | 0 | 4 (27%) | 8 (40%) | 8 (31%) |
| Retinopathy | 0 | 0 | Â 8 (55%) | 6 (30%) | 3 (12%) |
| (n=17) | |||||
| Survival by gestational age | 0 | 0 | 6 (40%) | 11 (55%) | 22 (84%) |
| (n=39) | |||||
| Overall survival from 22 WG (n=39) | 0 | 0 | 15% | 28% | 56% |
Table 3: Morbidity and mortality of EPIs.
Seventy-eight EPIs out of 30,000 births (0, 26%) were included in this study. Eighty-five EPIs were excluded from the study: 50 for abortion due to fetal abnormalities and 35 for in utero fetal death.
In total, 17 of 78 (21.7%) EPIs were born between 20 WG and 21 weeks+6 days gestation. Fifteen EPIs (19.2%) were born between 22 WG and 22 weeks+6 days gestation. Twenty EPIs (25.6%) were born between 23 WG and 23 WG and 26 EPIs (33.3%) were born between 24 WG and 24 weeks+6 days gestation (Figure 1). Thirty-nine out of 78 (50%) EPIs survived.
Out of all EPIs born between 22 WG and 22 weeks+6 days gestation, 40% survived, while 55% born from 23 WG to 23 weeks+6 days gestation and 84% delivered between 24 WG and 24 weeks+6 days gestation lived. The mean birth weight was 723 ± 179 grams, and 12.8% of the EPIs weighed less than 500 g. In addition, 55% of EPIs received antenatal corticotherapy.
The Apgar score was >7 at 5 min in 46% of cases. Forty-five EPIs out of 78 (58%) had had an umbilical cord artery pH assessed at birth. The pH of these 45 (9%) were <7.05. However, 19 pH ua was not performed because the umbilical cord was too thin and therefore difficult to puncture or because the obstetric-pediatric teams were busy with neonatal resuscitation.
Fifty-six EPIs (71.8%) were admitted the neonatal intensive care unit and had an orotracheal intubation during the first or the fifth minute of life.
All EPIs born before 22 weeks of gestation did not survive. Out of these 39 EPIs, 13 were stillborn or not resuscitated, 10 had respiratory failure, 6 suffered from chorioamnionitis, 4 experienced sepsis, 4 had cerebral hemorrhage, 1 was a case of peritonitis caused by digestive perforation and 1 experienced umbilical cord strangulation.
Neonatal Morbidity
Forty-nine of 78 (62%) EPIs presented with a hyaline membrane disease (HMD), and 39% evolved to a bronchopulmonary dysplasia (BPD). Thirty-three (42%) EPIs were infected before or during birth and 35 (45%) developed an infection afterwards. The most frequent causative bacteria involved in new-born infections were staphylococcus coagulase negative bacteria.
Thirty-eight (49%) EPIs presented with cerebral hemorrhage. Intraventricular hemorrhage was more frequent in those born between 23 and 24 WG (50%). Seventeen (22%) EPIs presented with retinopathy (RP), and this condition was more frequent for babies born between 22 and 23 WG (55%). The rate of RP decreased as the gestational age increased.
Ten (13%) EPIs had an ulcero-membranous entercolitis. Peritonis developed after a perforation in 5 cases (6%) that were surgically managed. Additionally, 19 EPIs (24%) presented with a persistence of the arterial channel. A surgical cure was necessary in 10 of these cases (13%).
The mean length of hospitalization in the neonatal intensive care unit (NICU) was 42 days; 54% of cases stayed for less than 20 days (Table 3). Twenty-four EPIs were discharged from the hospital to routine pediatric follow-up. Five EPIs experienced a surgical cure of a persistent arterial channel.
Discussion
In our study, about half of the new-borns delivered between 20 WG and 24 weeks+6 days survived. When the age class of 20–21 WG+6 days was excluded, there were 39 survivors out of 61 (64%) births.
In their Swedish study (2004–2007), Felmann et al. [4] reported a survival rate ranging from 9.8% at 22 weeks to 85% at 26 weeks. Suciu et al. [11] found that 35% of babies born in Romania between 25 and 28 weeks survived. In our study, the short-term survival rates were better. This difference may be explained by the fact that our study is more recent; therefore, new-borns have benefited from progress in obstetrics management and neonatal resuscitation.
Approximately 50% of our new-borns improved following an antenatal corticosteroid treatment, which leads to a better survival rate along with a tocolytic treatment and the administration of surfactant to the new-born [4]. Given the important rate of survival starting at 22 weeks, a corticosteroid treatment should be discussed for all EPIs born at 22 weeks and after.
In our study, the survival rate increased with gestational age starting at 22 weeks. Other authors have reported similar results [4,11]. Therefore, neonatal resuscitation could begin at 22 weeks and may allow a large number of EPIs to survive.
The arterial umbilical cord pH was normal in the majority of cases that were collected. Despite quick management of some new-borns, the umbilical cord pH was low. It was correlated with intrauterine growth restriction, fetal infection, or fetal heart rate abnormalities during labour. These premature infants probably had fewer reserves and more difficulty tolerating uterine contractions.
The Apgar score was greater than 4 at 5 minutes for most EPIs. The majority of EPIs also underwent orotracheal intubation. The mean weight of EPIs (723 g) in our study was similar to those reported by other studies for new-borns of equivalent gestational ages (4). For example, Cabaret et al. [10] found that the mean weight varied between 640 and 765 g for babies born between 22 WG and 25 weeks +6 days, gestation and the survival rate was 13/32.
In our EPIs, HMD represented the first cause of neonatal morbidities followed by the primary or secondary infections of the new-born. Approximately 1 of 4 HMD cases evolved into bronchopulmonary dysplasia. Cerebral haemorrhaging occurred approximately every fourth time, while retinopathies were present every fifth time.
Neurological and retinal lesions are correlated with a severe handicap [12]. The frequency of these lesions decreases with increasing gestational age. All these morbidities are found in the literature with variable frequencies according to gestational age [4,7,13]. For Kate et al. [7], the frequency of BPD was much higher at 61%, but their study was older than ours, and neonatal care may have improved since then. Pinto Cardoso et al. [14] reported that the rate of BPD in EPI remained stable between 2000 and 2010.
In their study, Suciu et al. [11] found that 26% of EPIs presented with retinopathy. In the Epipage study, 2% of EPIs experienced a moderate or severe visual deficiency after five years [8]. According to some other studies, the frequency of neurological lesions varies between 10 and 50% [4,7,14,15] in these infants.
Concerning the prognosis of EPI:
In the EXPRESS study group [15], 47% of EPIs born before 27 weeks survived to the age of 1 year without severe morbidity. For Farooqi et al. [12], only 10 to 30% of EPIs born prior to 26 weeks will have significant behavior or memory disorders at 11 years of age. The majority of EPI will experience satisfactory development.
Among the causes of death, infection occurred approximately every fourth time following chorioamnionitis or septic shock. The rate of infections can be explained by the great frequency of the premature rupture of membranes in our study and of the immaturity of the immune system of the EPIs. Moreover, many components of neonatal resuscitation may cause secondary infections (intubation, urinary catheters, and intravenous perfusions). The treatment of these infections may be improved by using more targeted antibiotic therapy.
In our study, the mortality rate during infant hospitalization (50%) was slightly higher than the 40% reported by other investigations [13,16-18]. This variation may be because we included very early births up to 20 WG. The causes of death in these EPIs were mainly neurological and respiratory, which were similar to the results of most previous studies [6,9,13].
The leading maternal cause of premature birth before 26 WG was a premature rupture of the membranes followed by hypertensive and vascular disorders of pregnancy. These results are in agreement with those of other studies [4,13].
Limitations of the Study
Our results represent short-term findings. However, although our study was retrospective, we identified a high rate of survival of EPIs after 22 weeks. Paediatric follow-up visits with these children are in place to manage and diagnose or eventually treat some complications, especially neurological impairments. Other studies have shown that the majority of new-borns who make it through the early neonatal critical period will survive without major lesions or defects or with only moderate difficulties [15,19,20].
Conclusion
The survival rate of EPIs between 20 WG and 24 weeks+6 days gestation is important and increases with gestational age. Neurological, respiratory, and infectious neonatal morbidities remain high, but many of them are curable with the therapeutic progress of neonatal resuscitation. The results of our study are encouraging in the shortterm and indicate the possibility for active neonatal resuscitation beginning at 22 weeks with significant survival rates. A median and long-term follow-up study of these infants has already begun. In addition, antenatal corticotherapy using magnesium sulphate should be discussed foe EPIs beginning at 22 weeks, as well as treatment with surfactants.
References
- Serenius F, Ewald U, Farooqi A, Holmgren PA, HÃ¥kansson S, Sedin G (2004) Short-term outcome after active perinatal management at 23-25 weeks of gestation. A study from two Swedish perinatal centres. Part 3: Neonatal morbidity. Acta Paediatr 93: 1090-1097.
- Leuthner SR (2014) Borderline viability: Controversies in caring for the extremely premature infant. Clin Perinatol 41: 799-814.
- Moriette G, Rameix S, Azria E, Fournié A, Andrini P, et al. (2010) Outcome of infants born before 28 weeks of postmenstrual age and definition of a gray zone. Arch Pediatr 17: 518-526.
- EXPRESS Group, Fellman V, Hellström-Westas L, Norman M, Westgren M, et al. (2009) One-year survival of extremely preterm infants after active perinatal care in Sweden. JAMA 301: 2225-2233.
- Delorme V, Bal G, Equy V, David-Tchouda S, Arnould P, et al. (2010) Preterm births circumstances in babies born before 35 weeks in French Alpes: PREMALP study. J Gynecol Obstet Biol Reprod. 39: 387-394.
- Morin M, Arnaud C, Germany L, Vayssiere C (2012) Preterm birth: Evolution 1994 to 2006. Gynecol Obstet Fertil 40: 746-752.
- Costeloe KL, Hennessy EM, Haider S, Stacey F, Marlow N, et al. (2012) Short term outcome after extreme preterm birth in England: Comparison of two birth cohorts in 1995 and 2006. The EPICURE studies. BMJ 345: 1-17.
- Larroque B, Ancel PY, Marret S, et al. (2008) EPIPAGE Study group. Neurodevelopmental disabilities and special care of 5 year old children born before 33 weeks of gestation a 263 longitudinal cohort study. Lancet 371: 813-820.
- Berger TM, Bernet V, El Alama S, Fauchère JC, Hösli I, et al. (2011) Perinatal care at the limit of viability between 22 and 26 completed weeks of gestation in Switzerland. Swiss Med Wkly.
- Cabaret AS, Charlot F, Le Bouar G, Poulain P, Bétrémieux P (2012) Very preterm births (22-26 WG): From the decision to the implement of palliative care in the delivery room. Experience of Rennes University Hospital (France). J Gynecol Obstet Biol Reprod 41: 460-467.
- Suciu LM, Puscasiu L, Szabo B, Cucerea M, Ognean ML, et al. (2014) Mortality and morbidity of very preterm infants in Romania: how are we doing? Pediatr Int 56: 200-206.
- Farooqi A, Hägglöf B, Sedin G, Serenius F (2011) Impact at age 11 years of major neonatal morbidities in children born extremely preterm. Pediatrics 127: 1247-1257.
- Autret F, Kieffer F, Tasseau A, Rigourd V, Valleur D, et al. (2009) Extreme prematurity: Comparison of outcome at 5 years depending on gestational age below or above 26 weeks. Arch Pediatr 16: 976-983.
- Pinto Cardoso G, Abily-Donval L, Chadie A, Guerrot AM, Pinquier D, et al. (2013) Epidemiological study of very preterm infants at Rouen University Hospital: Changes in mortality, morbidity and care over 11 years. Arch Pediatr 20: 156-163.
- EXPRESS Group (2010) Incidence of and risk factors for neonatal morbidity after active perinatal care: extremely preterm infants study in Sweden (EXPRESS). Acta Paediatr 99: 978-992.
- Kermorvant-Duchemin E, Sennlaub F, Behar-Cohen F, Chemtob S (2011) Epidemiology and pathophysiology of retinopathy of prematurity. Arch Pediatr 18 Suppl 2: 79-85.
- Doyle LW (2001) Outcome at 5 years of age of children 23 to 27 weeksâÂ?Â? gestation: refining the prognosis. Pediatrics 108: 134-141.
- Vanhaesebrouck P, Allegaert K, Bottu J (2004) The EPIBEL study: Outcomes to discharge from hospital for extremely preterm infants in Belgium. Pediatrics 114: 663-675.
- Ancel PY, Goffinet G (2015) EPIPAGE-2 writing group survival and morbidity of preterm children born at 22 through 34 weeks' gestation in France in 2011: Results of the EPIPAGE-2 cohort study. JAMA Pediatr 169: 230-238.
- Farooqi A, Hägglöf B, Serenius F (2013) Behaviours related to executive functions and learning skills at 11 years of age after extremely preterm birth: A Swedish national prospective follow-up study. Acta Paediatr 102: 625-634.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 3269
- [From(publication date):
April-2017 - Nov 22, 2024] - Breakdown by view type
- HTML page views : 2576
- PDF downloads : 693