Serial Measurement of Anterior and Posterior Uterocervical Angles as a Predicting Tool for Spontaneous Preterm Birth
Received: 05-May-2022 / Manuscript No. roa-22-63011 / Editor assigned: 07-May-2022 / PreQC No. roa-22-63011 (PQ) / Reviewed: 20-May-2022 / QC No. roa-22-63011 / Revised: 23-May-2022 / Manuscript No. roa-22-63011 (R) / Published Date: 30-May-2022 DOI: 10.4172/2167-7964.1000380
Abstract
Introduction:This study aimed to evaluate the association between sonographic markers including anterior and posterior uterocervical angles (UCA) in the first and second trimester and the mean difference of UCA measured in the first and second trimester with the occurrence of the spontaneous preterm birth (PTB) in the pregnant women.
Methods:Ultrasonographic measurements of the angle among the anterior and posterior inferior uterine segment and the cervix were done in singleton pregnancies in gestational age (GA) of 13 and 14 weeks and repeated in 28th weeks of gestation. Participants were followed until delivery and GAs were documented.
Results: Among 216 pregnant women, 31 participants had PTB. The mean of anterior and posterior UCA in the PTB group was more than term group, significantly; at the same trimester (0.001>p). The mean difference between first and second trimester anterior UCA was greater in the PTB group (7.0±4.2vs4.7±1.6, p=0.008). The cut-off value according to ROC analysis in predicting PTB for anterior UCA at the first trimester was 95.5º and for the second trimester was 105.5º. Cut-off values for Posterior UCA at first and second trimester were 96.5º and 104.5º, respectively. The Pearson analysis revealed a significant negative relationship between anterior and posterior UCA at first and second trimesters and gestational age at birth.
Conclusion:Anterior and posterior UCAs measured in the first and the second trimester has the potential to serve as predicting markers for the sPTB. Between the aforementioned markers, anterior UCA when is measured in the second trimester is more valuable (the best AUC for sPTB).
Keywords
Introduction
Premature birth (PTB) refers to the live birth before 37 weeks of gestation and is considered the principal cause of perinatal mortality and morbidity and one of the most important causes of long-term morbidity and increased health costs [1, 2]. About 70% of all PTBs occur spontaneously (not induced for clinical reasons) [3]. History of PTB, black race, short cervix, low body mass index (BMI), comorbidities and positive fetal fibronectin test are known risk factors for sPTB [3, 4].
Regarding the role of cervix in pregnancy, cervical incompetence can be associated with pregnancy loss or sPTB. Ultrasonographic analysis of the cervix by itself including cervical length (CL), funnelling, mean acoustic attenuation [5], cervical inconsistency index [6], cervical glandular area [7], dynamic changes and elastoscan of the cervix are considered as markers evaluated for assessment of cervical incompetence [8]. On the other hand, some predicting models of sPTB used CL in combination with clinical and laboratory markers to predict the probability of PTB [9, 10].
In recent years, investigations proposed uterocervical angle (UCA), measured by transperineal or transvaginal ultrasound as a novel predictor for sPTB in singleton and twin pregnancies. UCA is defined as the angle between the lower uterine segment and the cervix. It’s been shown to be wider in pregnancies complicated by sPTB [11]. According to this theory, the widening of UCA represents a more linear and direct anatomical relationship between the uterine outlet and the cervix, but an acute angle results in an anatomical geometry that decreases the force on cervix [12].
But current data about this marker are not sufficient and prospective studies with standard methods have been strongly recommended to diminish heterogeneity and achieve more reliable conclusion [11, 13]. So, we conducted this study to evaluate the association between uterocervical angles (anterior and posterior) in the first and second trimesters and occurrence of PTB. On the other hand, we evaluated the association between mean differences of first and second trimester UCA and the occurrence of PTB.
Materials and Methods
This prospective and observational study was conducted between April 2019 and April 2020 in Shohada-ye-Tajrish hospital (Tehran, Iran) affiliated with Shahid Beheshti University of Medical Sciences. The study protocol was approved by the institutional review board and ethical committee of the University. Pregnant women who were referred to our radiology department for routine first trimester pregnancy ultrasound examinations and meet the inclusion criteria were included. Written informed consents were signed by all participants.
The inclusion criteria were:
1. Singleton pregnancy
2. Gestational age (GA) of 14 weeks
3. Intact membranes
4. Ages between 18 to 50 years and
The exclusion criteria were as follows:
1. Refusal to sign informed consent or continue the study at any stage
2. Inability to follow the participant until delivery
3. Being in active labor at the time of examination
4. History of the previous manipulation of cervix
5. History of preterm labor
6. Undergoing the preterm labor regarding the clinical indications (preeclampsia, intrauterine growth restriction (IUGR), placental abruption and so on)
7. Pregnancy problems such as poly or oligohydramnios, fetal anomaly, miscarriage or uterine infections
Patients’ demographic information, obstetric history and pregnancy data were recorded in their first visit. All participants underwent the transvaginal ultrasound examination of the cervix in 14 weeks of gestation and then in 28 weeks and include anterior UCA and posterior uterocervical angle (posterior UCA).
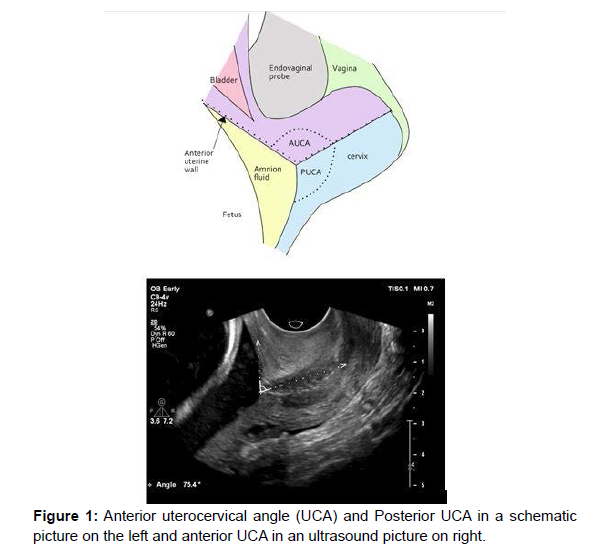
For drawing the anterior UCA, the first line is drawn from the internal to the external os, and then the second angle line is drawn through the anterior wall of the lower uterine segment, the angle between these lines is considered as anterior UCA. In presence of funneling, the first line of UCA was drawn in the same way, but the second line was drawn from the internal os to the lower half of the lower segment of the uterus. For drawing the posterior UCA, the first line is drawn from internal os to external os, and then the second line is drawn along the posterior wall of the lower segment of the uterus. The angle between these lines is equivalent to posterior UCA. UCAs’ differences are also calculated by subtraction of two angles (Figure1).
All examinations were performed by an attending radiologist with 3 years of experience using a 6-9 MHz vaginal transducer (Philips Healthcare, Affiniti 50 ultrasound machine).
Participants were followed up to delivery. If the mother returned to our center for her labor, the delivery data was recorded and if they didn’t, the outcome of the pregnancy and gestational age were asked during a phone call. Labor before 37w was considered as preterm labor.
Statistical analysis
All quantitative data are presented as means ±SD. An independent student t-test was used for comparison of the mean of parametric data between these two groups. Descriptive data were applied for the investigation of frequencies among patients’ group. The Chi-Square test was used to compare percentages or frequencies of data between the groups. Pearson correlation test was used to examine the relationship between quantitative variables and Spearman correlation test was applied to examine the ranking variables. The effect of an independent variable on the level of dependent variables was also investigated using multiple linear regressions. ROC curve was provided to measure sensitivity and specificity of UCA values. Data were analyzed using SPSS software (IBM SPSS, Version 22), and a p<0.05 was considered as significant.
Results
In the beginning 234 mothers were enrolled in the study. During the follow-up period 18 mothers were excluded (6 participants underwent preterm labor because of clinical indications and 12 women refused to return for the follow up studies)
Finally, a total of 216 mothers with a mean age of 27.92 ± 4.64 years were included in the study. Thirty-one mothers (14.4%) exhibited spontaneous preterm birth (PTB group), while 185 (85.6%) mothers had normal birth (term group).
There was no significant difference between the PTB and term groups regarding the mean body mass index (BMI) and maternal age. The frequent distribution of parity, number of abortions and smoking habits of mothers didn’t show significant differences between groups (Table 1).
| Preterm group | Term group | P-value | ||
|---|---|---|---|---|
| Number | 31 | 185 | ||
| Maternal age (Years) | 28.0±3.7* | 27.9±4.7 | 0.858 | |
| BMI (kg/m2) | 24.3±2.3* | 23.8±2.8 | 0.289 | |
| Number of parities | 0 | 26 (83.9%) | 115 (62.2%) | |
| 1 | 5 (16.1%) | 50 (27.0%) | 0.08 | |
| 2 | 0 | 15 (8.1%) | ||
| 3 or more | 0 | 5 (2.7%) | ||
| Number of abortions | 0 | 28 (90.3%) | 153 (82.7%) | |
| 1 | 3 (9.7%) | 29 (15.7%) | 0.74 | |
| 2 or more | 0 (.0%) | 3 (1.6%) | ||
| Smoking history | Hookah+Cigarettes | 0 (.0%) | 1 (.5%) | |
| Cigarettes | 1 (3.2%) | 6 (3.2%) | ||
| Hookah | 0 (.0%) | 1 (.5%) | 0.95 | |
| Non-smoker | 30 (96.8%) | 177 (95.7%) |
Table 1: Comparison of demographics, party, number of abortions and smoking history between preterm and term groups.
The mean of anterior UCA and posterior UCA in preterm group was significantly more than term group at the same trimester (p<0.001) (Table 2).
| Preterm group | Term group | P-value | |
|---|---|---|---|
| First trimester anterior UCA | 108.4±9.0* | 89.6±8.2 | <0.0001 |
| Second trimester anterior UCA | 115.4±8.7 | 94.4±8.3 | <0.0001 |
| First trimester Posterior UCA | 106.3±9.2 | 87.3±11.6 | <0.0001 |
| Second trimester Posterior UCA | 110.4±20.1 | 92.7±10.2 | <0.0001 |
| Anterior UCA difference | 7.0±4.2 | 4.7±1.6 | 0.008 |
| Posterior UCA difference | 4.0±1.0 | 5.3±1.0 | 0.723 |
| *Values are expressed as mean± standard deviation | |||
Table 2: Comparison of anterior uterocervical angles (UCA) and posterior UCA in preterm and term group.
The mean difference of first and second trimester anterior UCA was significantly higher in the PTB group (p<0.001) but no significant difference was noted between the groups regarding the mean difference of first and second trimester posterior UCA between two groups (p=0.54, Table 2).
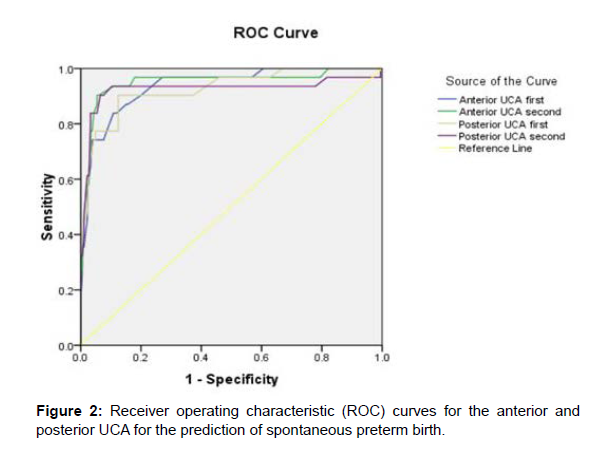
According to the receiver operating characteristic (ROC) curve, the cut-off value for anterior UCA at first trimester exam in predicting preterm delivery had 96.8% sensitivity and 80% specificity in 95.5º (area under the receiver operating characteristic curve (AUC): 0.937, 95% CI, 0.89-0.98). The best cut-off value for anterior UCA at 28th week scan in predicting preterm delivery was 105.5º (sensitivity: 90.3%, specificity: 94.1%, AUC: 0.951, 95% CI, 0.89-1.003). This cut-off for posterior UCA at first scan in predicting preterm delivery with sensitivity: 90.3%, specificity: 86.5%, AUC: 0.926, 95% CI, 0.87-0.98, was 96.5º. The More predictable cut-off value in predicting preterm delivery by posterior UCA second scan was 104.5º with 90.3% sensitivity and 92.4% specificity (AUC: 0.925, 95% CI, 0.84-1.003) (Figure 2).
The Pearson correlation analysis revealed a significant and negative relationship between anterior and posterior UCA at first and second trimesters and gestational age at birth. Higher mean values of anterior and posterior UCA at first and second trimesters were significantly associated with lower gestational age (p<0.001).
Pearson correlation analysis between mean difference of the first and second anterior and posterior UCA values and gestational age showed while higher mean difference of the first and second anterior UCA was significantly associated with lower gestational age at birth (r= -0.284 and p<0.001), no significant association was observed between the mean difference of first and second posterior UCA and gestational age at birth (r = 0.001, p = 0.986).
Discussion
In this study, we evaluated the association of anterior and posterior UCA for occurrence of PTB. To our knowledge, this is the first study that evaluated the mean of anterior and posterior UCA either at first or second trimesters and we found that it was significantly higher in women with preterm deliveries than those with normal deliveries. Our study demonstrated that anterior UCA in the second trimester is the best predictor of preterm delivery with a cut-off value of 105.5º. Also, the mean difference of first and second trimester anterior UCA was higher in PTB group.
The cervix has a complex physiological and anatomical role in the normal pregnancy and it has an essential role in the pathophysiology of the labor [14]. As the pregnancy advances pressure of the pelvic organs, amniotic fluid and the growing fetus on the internal os increases and it can affect cervical function. It could be stated that a blunt angle between the cervix and the uterus will result in more direct anatomical relationship between them and gives more direct force on the internal os that results in expansion of the internal os. Conversely, sharper angle between the cervix and the uterus will decrease the pressure transferred to the internal os and cervix [15-17]. It’s been reported that as pregnancy advances anterior UCA angle changes that could be related to the increase in the size of the pregnancy products [18].
Some retrospective studies suggested the anterior UCA as a predicting marker for the PTB. In a retrospective control casecontrol study Sochacki-Wojcicka et al. showed that median anterior UCA in pregnancies with PTB was wider than control group in the first trimester (preterm group: 115.5º control group: 85º) and second trimester (preterm group: 126º and control group: 91.5º) and the differences were statistically significant (P <0.05) [18]. Dziadosz et al. reported that UCA ≥95º was associated with PTB (<37 weeks of gestation) with the sensitivity of 80% and a UCA ≥105º with the sensitivity of 81% predicted PTB (<34 weeks of gestation) when the angles were measured during the second trimester (between 16 0/7- 23 6/7 weeks) [19]. Considering the anterior UCA measured in the second trimester, our results are in line with aforementioned studies. In our study the mean anterior UCA in preterm group (115.4º) was significantly wider than the normal group (94.4º) and the best cut-off value for anterior UCA in predicting preterm delivery was 105.5º with the sensitivity of 90.3%, and specificity of 94.1%. Lynch et al conducted a study on 114 women with twin pregnancy and concluded that UCA greater than 110º is related with PTB. However, second trimester UCA has a low likelihood ratio. Our study is performed in a prospective manner and doesn’t have some limitations of the retrospective studies. There is a potential for information and selection bias in retrospective studies. One of the limitations of these studies on this subject is that measurements are performed on stored images that mainly have been taken for the measurement of the CL. Therefore, some images are not optimal for the evaluation of UCA and some cases should be excluded.
Prospective studies showed the same results and proposed the association between wider angle and PTB. Farràs Llobet et al.in a prospective cohort study on 1453 singleton pregnancies measured the anterior UCA in singleton pregnant women between 19 and 22.6 weeks. The investigation showed that the model provided by a combination of CL, anterior UCA and history of SPTB is the best one in predicting the PTB (area under the curve: 0.64 and 95% CI: 0.55-0.72) They conclude that mid-trimester UCA is a poor index for prediction of PTB [20].Khamees also reported a cross-sectional prospective article on 167 high risk women. A UCA more than 105º was related to higher risk of PTB [21].
In another prospective cohort study Sawaddisan et al. reported that UCA in the sPTB group (123.4º) was significantly wider than those with term birth (104.3º) while the measurements were performed between 19.5-24 weeks of gestation. According to the ROC analysis curve the optimum UCA cut-off value was ≥110º, (sensitivity: 83.3% and a specificity: 61.2%, positive predictive value: 16.7% and negative predictive value: 97.5%) [22].
The main strength of our study was the measurement of posterior UCA and also the serial measurement of the posterior UCA and anterior UCA in the first and second trimesters and evaluation and comparison of the association of the angles and PTB in each trimester. On the other hand, the difference of the same angle in the first and second trimester was calculated and its association with the PTB was evaluated as an indicator of changes during the time. Another strength for this study is its prospective nature while the most of the previously performed studies are retrospective and therefore have limitations [13].
Limitations
We have several limitations in our study, first of all the gestational age at birth as the final outcome of the pregnancy was evaluated by a phone call in some cases and we had to rely on the mothers’ answers. The second limitation was that we just considered some factors that affect the PTB and we know that more known factors exist that we didn’t consider. Another limitation is that we didn’t measure the cervical length that could be used in different manners of combination and comparison with UCA in predation of PTB.
Conclusion
Anterior and posterior UCAs measured in the first and the second trimester has the potential to serve as predicting markers for the sPTB. Between the aforementioned markers, anterior UCA when measured in the second trimester is more valuable (the best AUC for SPTB). Moreover, difference between UCAs in first and second trimesters can have a remarkable negative relation in occurring sPTB. Further studies considering more risk factors of sPTB and adding the value of cervical length are needed.
Acknowledgement
This article has been extracted from the thesis written by Dr. Leyla Torabzade in School of Medicine Shahid Beheshti University of Medical Science (Registration No: IR.SBMU.MSP.REC.1399.055).
References
- Phillips C, Velji Z, Hanly C, Metcalfe A (2017) Risk of recurrent spontaneous preterm birth: a systematic review and meta-analysis. BMJ Open 7: e015402.
- Waitzman NJ, Jalali A, Grosse SD (2021) Preterm birth lifetime costs in the United States in 2016: An update. Semin Perinatol 45: 151390.
- Goldenberg RL, Culhane JF, Iams JD, Romero R (2008) Epidemiology and causes of preterm birth. 371: 75-84.
- Mazaki-Tovi S, Romero R, Kusanovic JP, Erez O, Pineles BL, et al. (2007) Recurrent preterm birth. Semin perinatol 31: 142-158.
- Guerrero QW, Feltovich H, Rosado-Mendez IM, Carlson LC, Hallcor TJ (2019) Quantitative ultrasound biomarkers based on backscattered acoustic power: potential for quantifying remodeling of the human cervix during pregnancy. Ultrasound Med Biol 45: 429-439.
- Parra-Saavedra MA, Gómez LA, Barrero A, Parra G, Vergara F, et al. (2011) Cervical consistency index: a new concept in uterine cervix evaluation. Donald Sch J Ultrasound obstetrics gynecology 5: 411-415.
- Pizzella S, El Helou N, Chubiz J, Wang LV, Tuuli MG, et al. (2020) Evolving cervical imaging technologies to predict preterm birth. Semin Immunopathol 42: 385-396.
- Köbbing K, Fruscalzo A, Hammer K, Möllers M, Falkenberg M, et al. (2014) Quantitative elastography of the uterine cervix as a predictor of preterm delivery. 34 :774-780.
- Carter J, Seed PT, Watson HA, David A, Sandall J, et al. (2020) Development and validation of predictive models for QUiPP App v. 2: tool for predicting preterm birth in women with symptoms of threatened preterm labor. 55: 357-367.
- Tekesin I, Eberhart L, Schaefer V, Wallwiener D, Schmidt S (2005) Evaluation and validation of a new risk score (CLEOPATRA score) to predict the probability of premature delivery for patients with threatened preterm labor. Ultrasound Obstet Gynecol 26: 699-706.
- Hessami K, Kasraeian M, Sepúlveda-Martínez Á, Parra-Cordero MC, Vafaei H, et al. The Novel Ultrasonographic Marker of Uterocervical Angle for Prediction of Spontaneous Preterm Birth in Singleton and Twin Pregnancies: A Systematic Review and Meta-Analysis. Fetal Diagn Ther 2021:1-7.
- Sur B, Misra S, Dash S (2017) Evaluation of the anterior cervical angle of the uterus to predict spontaneous preterm birth. Int J reprod contracept obstet gynecol 6: 2323-2327.
- Llobet AF, Martí LR, Higueras T, Fernández IZ, Portalés AG, et al. (2018) The uterocervical angle and its relationship with preterm birth. J Matern Fetal Neonatal Med 31: 1881-1884.
- Melamed N, Hiersch L, Meizner I, Bardin R, Wiznitzer A, Yogev Y et al. (2014) Is measurement of cervical length an accurate predictive tool in women with a history of preterm delivery who present with threatened preterm labor? 44: 661-668.
- Myers KM, Feltovich H, Mazza E, Vink J, Bajka M, et al. (2015) The mechanical role of the cervix in pregnancy. J Biomech 48: 1511-1523.
- Yao W, Yoshida K, Fernandez M, Vink J, Wapner RJ, et al. (2014) Measuring the compressive viscoelastic mechanical properties of human cervical tissue using indentation. J Mech Behav Biomed Mater 34: 18-26.
- Yoshida K, Jiang H, Kim M, Vink J, Cremers S, et al. (2014) Quantitative evaluation of collagen crosslinks and corresponding tensile mechanical properties in mouse cervical tissue during normal pregnancy. PLoS One 9: e112391.
- Sochacki-Wojcicka N, Wojcicki J, Bomba-Opon D, Wielgos M (2015) Anterior cervical angle as a new biophysical ultrasound marker for prediction of spontaneous preterm birth. Ultrasound Obstet Gynecol 46: 377-378.
- Dziadosz M, Bennett T-A, Dolin C, Honart AW, Pham A, et al. (2016) Uterocervical angle: a novel ultrasound screening tool to predict spontaneous preterm birth. 215: 376.
- Llobet FA, Higueras T, Calero IZ, Martí LR, Maiz N, et al. (2020) Prospective evaluation of the uterocervical angle as a predictor of spontaneous preterm birth. 99: 1511-1518.
- Khamees RE, Khattab BM, Elshahat AM, Taha OT, Aboelroose AA (2021) Uterocervical angle versus cervical length in the prediction of spontaneous preterm birth in singleton pregnancy. Int J Gynaecol Obstet 156: 304-308.
- Sawaddisan R, Kor-Anantakul O, Pruksanusak N, Geater A (2020) Uterocervical angle measurement for preterm birth prediction in singleton pregnant women with no history of preterm birth and normal cervical length: A prospective cohort study. Eur J Obstet Gynecol Reprod Biol 252: 30-35.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Torabzade L, Mahboubi-Fooladi Z, Khazaei M (2022) Serial Measurement of Anterior and Posterior Uterocervical Angles as a Predicting Tool for Spontaneous Preterm Birth. OMICS J Radiol 11: 380. DOI: 10.4172/2167-7964.1000380
Copyright: © 2022 Torabzade L. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 2249
- [From(publication date): 0-2022 - Mar 29, 2025]
- Breakdown by view type
- HTML page views: 1810
- PDF downloads: 439