Septic Keratosis Obturans: A Stealth Public Health Threat
Published Date: 29-Dec-2016 DOI: 10.4172/2161-119X.1000283
253848Author’s Note
The following paper is designed to be a training monograph for general health professionals involved in cerumen management. Here is presented the septic keratosis obturans, which is commonly confused with impacted cerumen. This insidious form presents with a cerumen veneer, is rarely accompanied with complaints of pain or discomfort, and as will be shown below, can turn deadly in its final stages when one’s immunology attempts to vascularize the septic mass. Since 1978 the author and associates have noted that because of a dramatic and steady increases in chronic disease in the population, that the incidence of this phenomena has likewise increased. However, the healthcare field is still responding as if it is business as usual and is a simple cerumen accumulation. The explanations given here come from a study conducted from 2002 to 2006 from a file base of more than 3000 patients in an Occupational Therapy/Hearing Health practice in Colorado [1]. This paper is intended to provide how the phenomena might be described to consumers and to the healthcare community, in general.
Introduction
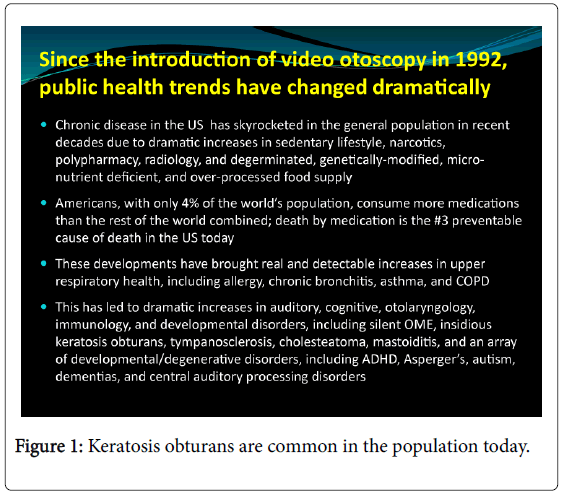
Often confused with ordinary earwax accumulations, insidious septic keratosis obturans appears to be increasingly common in the United States population today (Figure 1) [2]. Incidence is assumed to arise from increased prevalence in the general population of tooth/jaw sepsis, sinus infection, polypharmacy, metabolic disorders, autoimmune disorders, and chronic diseases, in general [3-6].
Healthy bodies exhibit an outer layer of tissue in the external auditory canal (EAC) called the stratum corneum, which is a thick and slowly moving keratin layer migrating outward from the umbo (center) of the ear drum at the rate of about 1mm per day. It carries with it dead skin tissues, debris, bacteria, fungi, and earwax. This is the self-cleaning mechanism of human ears or, historically, humans would be a deaf species indeed [7,8].
When acidosis conditions set in—as a result of chronic dehydration, environmental toxicities, untreated sepsis of the jaw or teeth, upper respiratory distress, intestinal infections, or from infected implanted prostheses—the EAC keratin layer often begins to peel up from the epithelial layers below and wrap around itself over and over, trapping inside it a milieu of collected bacteria, dead skin cells, and debris over the course of months and years [9].
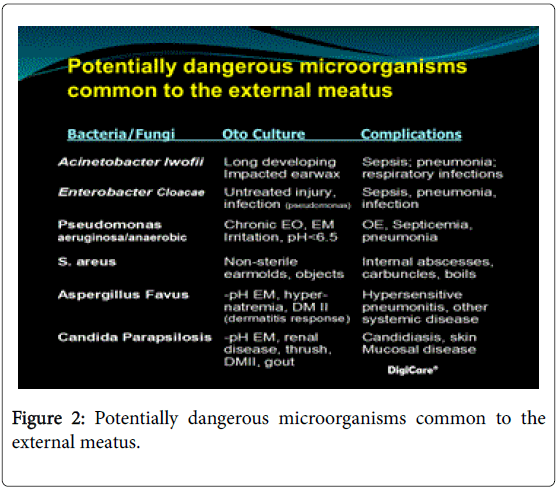
In many cases the keratosis obturans can become septic with an admixture of live bacteria, fungi, amoeba, and viruses (Figure 2) to see a typical microbial assay of a septic keratosis obturans). The author refers to this as the ear’s equivalent of an ingrown toenail, where bacteria is trapped in space unreachable by one’s immune system [10,11].
The growing bacteria inside the mass can inspire a cascade of proinflammatory cytokines, causing general inflammation, increased allergy, headache, and/or general discomfort throughout the body [12]. Over a period of years, the milieu grows until it has formed one, two, three, even four or more of these keratin-covered masses, leading in its final stages to vascularization of the obturans itself. Once vascularized, the body can respond in a manner not unlike an appendicitis or vascularized abscessed tooth at about year five or six of the obturans’ growth.
In this article we are not referring to an external canal cholesteatoma, a condition that is often confused with a keratosis obturans. Nor is the author referring to the more acute and better recognized form of keratosis obturans that is characterized by pain and swelling [13], but instead a more commonly encountered form that is at once insidious and undetectable by consumers even to the point of near-total occlusion of the external ear canal.
However, upon removal, it can become painful, and usually comes as a total surprise to the individual who, up to this point, has only been told by observing health professionals that it was “simply earwax and you might want to have it removed one of these days”, without noting the potential criticality of the manifestation.
Following is a pictorial explanation of what is too often mistaken by attending or observing health professionals as impacted earwax. In reality, however, it can be a septic keratosis obturans:
When a drop in cellular pH exceeds the body’s ability to maintain healthy levels—as a result of poor diet, de- hydration, environmental toxicities and/or untreated sepsis of the jaw or teeth, upper respiratory distress, intestinal infections, or from infected implanted prostheses— the EAC keratin layer begins to peel up from the epithelial layers below and wraps around itself over and over, trapping inside it a milieu of collected bacteria and dead cells over the course of months and years. In many cases today it becomes dangerously septic (to see what is often inside the obturans). This is the ear’s equivalent of an ingrown toenail [3,4].
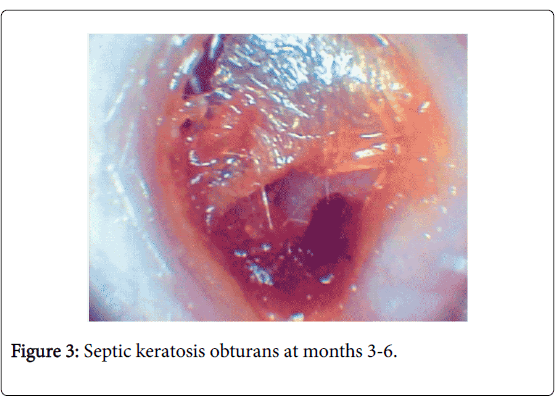
Months 3-6: The keratin begins to insidiously peel away from the underlying skin when cellular pH (re the Krebs’s cycle) of the body falls into acidosis state. The misdirected desquamated keratin continues to migrate into the space of the external canal, trapping desquamated skin cells, debris, bacteria, fungi, yeasts, pseudomonas, etc., eventually becoming septic, but remaining insulated from one’s vascular system. In our observations, this formation seems to be related to the onset of diabetes type 2, tooth/jaw sepsis, egregious polypharmacy, and/or chronic upper respiratory infection. It is not a self-initiating phenomena, nor does it seem to occur as a result of just one underlying cause or contributor (Figure 3).
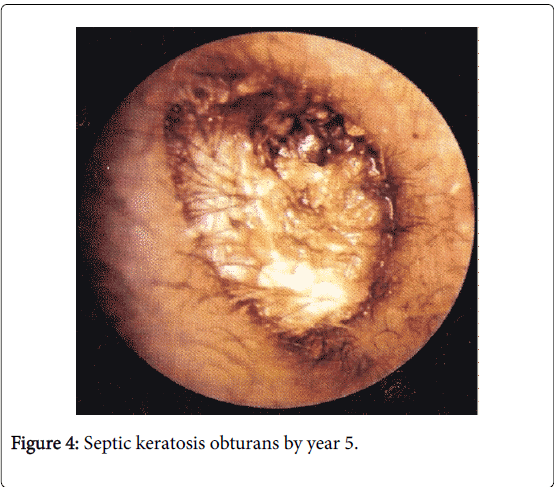
By Year 5: Now, it has grown into three, four or more obturans in succession. Unresolved, they can grow into External Ear Cholesteatomas, drawing bone fragments from the mastoid bone around it, eventually hollowing out a large cavity out of the EAC. If the mass vascularizes, and septicemia reaches the blood system, lab tests will indicate an acute diverticulitis-like septicemia. Immediate gentle removal is required. (Note: Often an advanced Obturans presents with a cerumen veneer, masking its serious nature to the observer. In the case at left, the individual did not complain of occlusion until a softening solution was applied) (Figure 4).
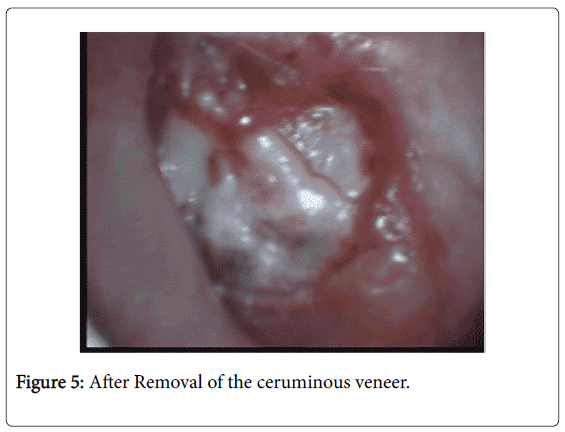
After removal of the ceruminous veneer: When the outer debris and earwax veneer are removed by mild syringing of warm antiseptic water, revealed is the first of several ker- atosis obturans. There one finds a series of membranous accumulations filled with trapped debris and growing bacteria. In the case illustrated here, there were four of these in succession, each one difficult to remove without first softening with MiraCell® Botanical Solution. They were already causing proinflammatory cytokine response elsewhere in the body and were interacting with sepsis in the teeth and jaw (Figure 5).
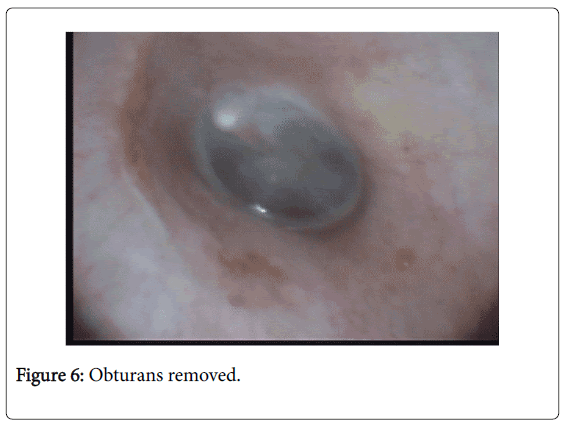
Obturans removed: A normal eardrum is usually revealed when the final obturans is removed. An investigation of the removed objects will reveal the kinds of serious bacteria and fungi listed in a slide (Figure 2). Upon removal, a prescription by the individual’s physician may be indicated for Cortisporin Ear Drops, Neomycin/Hydrocortisone or Augmentin/Hydrocortisone Ear Drops (applied 3-4 times daily for 7-10 days) followed by a two-week course of MiraCell® (or ProEar® solution by MiraCell®) botanical solution, used daily. In all cases, the cause(s) of the obturans need to found and treated (Figure 6).
Discussion
What sets off a keratosis obturans?
As mentioned earlier, a drop in the body’s cellular pH into acidosis state can cause the keratin tissue to peel up from underlying tissues in the ear canal. Today, about 120 million Americans are pre-diabetic (about 81 million) or full-blown diabetics mellitus type 2 (about 39 million, counting undiagnosed cases). Our clinical research screening protocol detects keratosis obturans in up about 25-35% in such individuals. In addition, it is often found to be co-occurring with other health conditions, such as tooth sepsis, long-term acid reflux and use of acid reflux medications, hypertension, gout, high triglycerides, IBS, and rheumatoid and osteoarthritis conditions [14-18].
Keratoses are often closely aligned to the head and neck region relative to infections in the teeth and jaw. Sepsis of the jaw appears to immunologically interact with sepsis of keratosis in the ears.
Other causes that can inspire keratosis formation are:
• A serious bout of acute pneumonia, esp. fungal type, or other serious infection. Ingrown toenail and diverticulitis may also interact.
• Septic debris developing in or around implanted prostheses, such as artificial joints, shoulders, hips, knees, feet or implants in the back.
• Trauma, accident, emotional distress, or toxic exposure. “Cotton Swab Trauma” or embedment of foreign object have been implicated.
• Certain medications, especially those that suppress immune system or affect the liver, epithelium or blood vessel integrity.
• Toxic effects of tobacco, alcohol, heavy metals or drug use.
How does One Avoid Relapse?
Every case is different and are advised to consult with their physician on what may be best for them. However, here are some general guidelines to start the discussion:
• Change diet & nutrition to conform to the SIRCLE® Pro- gram, which helps one raise their cellular pH to 7.35-7.45 and addresses unhealed injuries and stressors that contribute negatively to one’s health [19].
• Have teeth and jaw carefully examined by an oral surgeon who is intimately familiar with hidden crown/filling/ root canal problems that can harbor septicaemia [20].
• Be examined by an otologist who is knowledgeable in current trends in pseudomonas and keratosis obturans [20].
• If you have an implanted prosthesis, ask your physician about setting up a prophylactic to assure sepsis does not develop again. In most cases, Augmentin 250 mg or 500 mg taken 3 times per day for two or three days every 3 or 6 months has been advised (Rarely Ciprofloxacin) [20].
• To maintain EAC health use MiraCell on a regular basis (Figure 7) [22].
References
- Chartrand MS (2010) Video otoscopy: A quantitative view of the relationship between external ear keratin status and success in adaptation to hearing aids. Rye, CO: DigiCare Behavioral Research.
- Chartrand MS (2015) Incidence of keratosis obturans in an occupational therapy clinic. DigiCare Behavioral Research, Casa Grande, AZ.
- Oral Health America (2006) A state of decay: The oral health of older Americans.
- Rattue G (2012) Autoimmune Disease Rates Increasing. Medical News Today.
- Thorsteinsson AL, Vestergaard P, Eiken P (2014) External auditory canal and middle ear cholesteatoma and osteonecrosis in bisphosphonate-treated osteoporosis patients: A Danish national register-based cohort study and literature review. Osteoporos Int 25: 1937-1944.
- Johnson A, Hawke M (1988) Non-auditory physiology of the external ear. In: Jahn AF, Santos-Sacchi J (eds.) Physiology of the ear. New York: Raven Press, pp:41-58.
- Naiberg J, Berger G, Hawke M (1984) The pathologic features of keratosis obturans and cholesteatoma of the external auditory canal. Arch Otolaryngol 110: 690-693.
- Chartrand MS (2004) The importance of the keratin layer to successful fitting and treatment (Continuing Education). Livonia, Michigan: International Hearing Society.
- Kemp RJ, Bankaitis AE (2000) Infection control for audiologists. In: Hosford-Dunn H, Roeser R, Valente M (eds.) Audiology diagnosis, treatment and practice management. Vol. III, New York: Theime Publishing Group.
- Schulte W, Bernhagen J, Bucala R (2014) Cytokines in Sepsis: Potent Immunoregulators and Potential Therapeutic Targets—An Updated View. Mediators of Inflammation 25: 1937-1944.
- Sundstrom J, Mulligan K (2002) Neuroanatomy interactive syllabus. Chapter 7: Auditory system, University of Washington.
- Persaud RA, Hajioff D, Thevasagayam MS, Wareing MJ, Wright A (2004) Keratosis obturans and external ear canal cholesteatoma: How and why we should distinguish between these conditions. Clin Otolaryngol Allied Sci 29: 577-581.
- Persaud RA, Hajioff D, Thevasagayam MS, Wareing MJ, Wright A (2004) Keratosis obturans and external ear canal cholesteatoma: How and why we should distinguish between these conditions. Clin Otolaryngol Allied Sci 29: 577-581.
- Thorsteinsson AL, Vestergaard P, Eiken P (2014) External auditory canal and middle ear cholesteatoma and osteonecrosis in bisphosphonate-treated osteoporosis patients: A Danish national register-based cohort study and literature review. Osteoporos Int 25: 1937-1944.
- Chartrand MS (2003) Video otoscopy observation and referral: The FDA red flags. The Hearing Professional, pp: 9-14.
- King JE (2007) Sepsis in Critical Care. Crit Care Nurs Clin North Am 19: 77-86.
- Chartrand MS (2016) How to Get Your Health Back & Take Ownership of Your Life, Second Edition. Casa Grande, AZ: DigiCare Behavioral Research
- Chartrand MS (2016) Septic Dental Disorders: Unrecognized Public Health Threat. Casa Grande, AZ: DigiCare Behavioral Research.
- Chartrand MS (2011) Prosthetics Sepsis: Talking Paints for You and Your Doctor. Casa Grande, AZ: DigiCare Behavioral Research.
- Chartrand MS (2002) 960 Patient Observation Study. Orem, Utah: MiraCell, Inc.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 10174
- [From(publication date): 0-2016 - Apr 04, 2025]
- Breakdown by view type
- HTML page views: 9278
- PDF downloads: 896