Research Article Open Access
Separation Anxiety, Social Phobia and Generalized Anxiety Disorders in the Chilean Epidemiological Study of Children and Adolescents
Flora de la Barra1*, Benjamin Vicente2, Sandra Saldivia2, Roberto Melipillan21East Psychiatry Department, University of Chile, Chile
2Psychiatry Department, University of Concepcion, Chile
- *Corresponding Author:
- Flora de la Barra
East Psychiatry Deptment
University of Chile, Chile
Tel: 5695321155
E-mail: torbarra@gmail.com
Received Date: April 05, 2013; Accepted Date: May 08, 2014; Published Date: May 15, 2014
Citation: de la Barra F, Vicente B, Saldivia S, Melipillan R (2014) Separation Anxiety, Social Phobia and Generalized Anxiety Disorders in the Chilean Epidemiological Study of Children and Adolescents. J Child Adolesc Behav 2:133. doi:10.4172/2375-4494.1000133
Copyright: © 2014 de la Barra F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Child and Adolescent Behavior
Abstract
The prevalence, correlates, comorbidity and service use of three anxiety disorders in a broad sample of Chilean children and adolescents is reported in this study. The disorders studied were Separation anxiety (SAD), Generalized anxiety (GAD) and Social anxiety. Data were obtained from an extensive epidemiological study of psychiatric disorders in the community. DSM-IV diagnoses were assessed by means of the DISC-IV interview, demographic and family variables through the family assessment device and family history screen instrument, as well as the services provided by the Service Assessment Instrument. Prevalence with significant impairment for Separation anxiety was 4.8%, for social phobia, 3.7%, for generalized anxiety 3.2%, and 8.3% for any of the three disorders. Associated risk variables were as follows: low family income, family psychopathology, living with only one parent, maltreatment. A positive evaluation of family functioning was a protective factor against disorders. A high degree of comorbidity between the three anxiety disorders and with other groups of disorders was observed. The services were used by 22.3% of the children and adolescents diagnosed with any of the three anxiety disorders and within them, school based services were the most used. Findings are discussed and compared with other studies
Keywords
Anxiety disorders in children; Adolescents; Epidemiology; Prevalence studies
Introduction
Anxiety symptoms are common in childhood and adolescence, ranging from normative symptoms or sub-syndromal symptoms to full blown disorders. Structured interviews specially designed for theses ages are commonly utilized to determine the presence of categorically defined anxiety disorders. On the other hand, most studies are based on the epidemiology of anxiety disorders in general. Hence, rates for “any anxiety disorder” range from 15 to 20%. A recent review indicates an average 12-month prevalence of 8%, with ranges from 2% to 24% [1,2]. The United States of America National Comorbidity Survey (NCS-A) has reported 31.9% lifetime prevalence in adolescents 13- 18 years old and 8.35 % with severe impairment [3]. More recently, the research has been focused on specific anxiety disorders, such as longitudinal and laboratory studies which have shown consistently that different types of anxiety disorders have different correlates, predictors and courses. Therefore, the existing classification systems consider these narrow categories. DSM-IV-TR, the system in use when this study was carried out considers: Simple Phobias, Social Phobia, Generalized Anxiety Disorder [GAD], Post Traumatic Stress Disorder [PTSD], Obsessive-compulsive disorder [OCD], agarophobia and Panic Disorder. Separation Anxiety disorder [SAD] is classified in the Section “Disorders usually first diagnosed in infancy, childhood and adolescence”, in a category of “Other disorders of infancy, childhood or adolescence” together with Selective Mutism [4].
The prevalence of psychiatric disorders in the community can vary as a result of differences in the studied age groups, instruments, information sources and diagnostic classifications used [5]. In addition, most studies have been carried out in western industrialized countries and there is a lack of these studies in South American countries. A metaanalysis of studies performed in different countries by means of the Well-being Assessment (DAWBA) interview also showed variations: rates that ranged from 1.8% to 12.7% [5]. Estimations using the NIMH Diagnostic Interview Schedule for Children version IV (DISC-IV) ranged from 8.8% in New Zealand 11 year-olds to 50.5% for 9-17 year olds in 5 areas of the United States and Puerto Rico [4,5]. The addition of impairment criteria makes rates more consistent across studies and some anxiety disorders such as simple phobias fall dramatically [2,5-7]. In all the studied countries, anxiety disorders present high prevalence and early onset. Most studies indicate female preponderance in anxiety disorders that emerges at 6 years of age and increases along the life span [8-10].
In both cross-sectional and longitudinal studies, a high level of comorbidity has been found between the different anxiety disorders in clinical and community samples. High comorbidities with depression [O.R.: 8.2], conduct disorder [O.R. 3.1] and Attentional Deficit/ Hyperactivity Disorder (ADHD) [O.R. 3.0] have also been reported [2,5-7,9].
Many correlates have been found in children and adolescents with anxiety disorders such as: female gender, low educational level, low family income, family aggregation of depression and anxiety disorders, maternal depression, neuroticism traits and inhibited temperament in early childhood, as well as individual differences in children’s physiological regulation. Early adversity is found to be associated with many psychiatric disorders, including anxiety. Functional brain abnormalities have been detected in youth with anxiety disorders, such as hypersensitivity of the amygdala, though it is not clear if they correspond to correlates or vulnerability factors. Longitudinal studies on infants with behavioural inhibition followed to adolescence stress the importance of the circuit connecting the amygdala to the lateral ventral pre frontal cortex in attention bias to threat in the pathway to anxiety disorders. Parenting style can also act as a risk factor or mediator [2-14].
Longitudinal studies indicate a moderate homotypic continuity for anxiety disorders, but they also carry an elevated risk for developing other anxiety disorders, depression, substance abuse and other disorders. Both anxiety and depression cross-predict each other developmentally. Follow up studies indicate that girls internalizing symptoms increase whereas symptoms in boys decrease from late childhood to mid adolescence [9,11,12].
A study of psychiatric disorders in children and adolescents in Chile was performed in order to contribute to the knowledge of these aspects in the country. A cross-sectional method was used to assess psychiatric disorders with full diagnostic criteria plus significant impairment in the community. The aim of this study is to report the findings about the anxiety disorders evaluated in the context of this broader research: prevalence, associated factors, comorbidity and service use.
Method
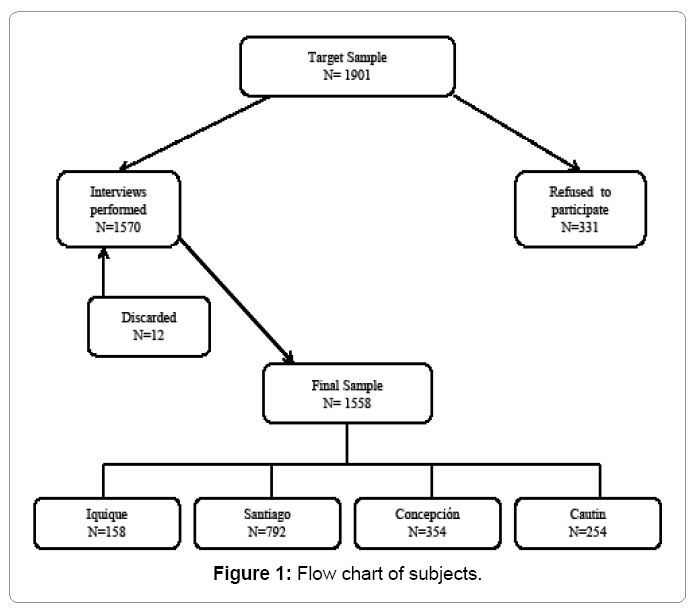
Participants: A stratified household sample representative of the country’s children aged 4–11, and adolescents aged 12–18 was obtained from attendees at primary care centres at Concepción, Chile. Chile is administratively divided into 51 provinces, grouped in 15 regions, with a population of nearly 17 million. From these, 5.3 million were under 19 years of age, according to 2002 census. Most of Chile’s population, 89%, is represented by urban dwellers. Figure 1 shows the flow chart of subjects.
The sample of children and adolescents was selected from four geographically distinct provinces. They were chosen, because of their condition of being representative of the distribution of the national population, where a former prevalence study of psychiatric disorders in adult population had been previously carried out. The provinces were: Santiago, Concepcion, Iquique and Cautin. One third of the nation’s population resides in the capital city, Santiago. On the other hand, Concepcion is located in Central Chile and it is the second largest city. Iquique is located in the north of the country, in a desert region with many isolated towns. The province of Cautin, is sited in southern Chile, and their population is mainly located in rural areas.
Distribution was as follows: 50.9% males and 49.1% females; 52.9% children 4-11 years of age and 47.1% adolescents 12-18 years of age. The sub-sample of children with psychiatric disorders was 560.
Procedures: In Chile, provinces are subdivided into municipalities, (comunas in Spanish), then into districts, and finally into blocks. In this study, each of these blocks was randomly selected. The number of available households in each block was calculated and the number required in each block was also determined. The households were chosen clockwise, starting from the first one on the northeast corner by means of a computer algorithm specially designed for this purpose. Twelve homes per block were identified and 5 were surveyed. Selection of either child or adolescent to be interviewed was based on their birth date, as close to the interview date as possible. If more than one child had the same birth date, ties were resolved by a coin toss or the use of a Kish table in the event of more than one tie.
The sites were completed in the following order: Cautin, Santiago, Iquique, and Concepcion. The survey was conducted by the University of Concepcion’s Department of Psychiatry and University of Chile’s East Mental Health Department between April 2007 and December 2009.
Written informed consent was obtained from the adult responsible for each child. In order to assure confidentiality, the data analysis team did not have access to any identifying information. The adult responsible for each child or the adolescent was offered the opportunity to receive the diagnostic results by certified letter based on the DISCIV upon request. Identified cases were recommended to look for treatment in the local mental health network. Unfortunately, this did not guarantee that treatment would effectively take place as it depended on the caretaker or the adolescent following the recommendations and availability of mental health resources. The project of the present study was approved by two Ethical Research Committees: the University of Concepcion and the National Fund for Science and Technology [FONDECYT], the Chilean State funding institution.
Measures: The presence of a psychiatric disorder was assessed by means of the DISC-IV, a highly structured interview that yields DSMIV and ICD-10 diagnoses which can be used by non-professional persons. DISC-IV was designed in the National Mental Health Institute (NIMH) in the United States of America and submitted to several revisions since 1979 to fit the different classification systems. Its efficiency, validity and reliability have been extensively reviewed, and it has been used in many prevalence studies across different countries. The Spanish version was validated in Puerto Rico, and adapted and revalidated for Chile [15,16].
Interviews took place at home, in a private space without others present and with the parent or primary caretaker of children aged 4-11 (74.8% mother, 9.3% father, 7.8% grandparent, 5.1% sibling, 3.0% other) present. In the case of 12-18 year old, the interview was conducted directly with the adolescent and nobody else present. Interviewers were psychology graduate students who received two days intensive group training on the instruments use, followed by several pilot administrations, individually supervised by a researcher. During every time in which the field-work was taking place, each completed interview was reviewed by the research team, and discrepancies were addressed with interviewers in order to obtain clarifications or corrections. Due to budget restrictions, the researcher team had to select the disorders considered more prevalent and clinically relevant to be evaluated: social phobia, separation anxiety disorder, generalized anxiety disorder (GAD), eating disorder, major depressive disorder, dysthymia, schizophrenia, ADHD, oppositional-defiant disorder (ODD), conduct disorder, alcohol use disorders, cannabis use disorders, nicotine dependence, and other substance use disorders. Other diagnoses were excluded, as well as other anxiety disorders.
The four impairment algorithms contained in the DISC-IV interview were ascertained according to the extent in which symptoms in six domains had stressed the child or affected his or her school achievement, or relationships with caretakers, family, friends or teachers. Impairment criteria A required that at least one of the impairments is given an intermediate or severe rating (sometimes or many times; bad or very bad); criteria B indicated that at least two intermediate or severe impairments; criteria C, at least one impairment in the severe category; and criteria D required that criteria B or C is present, i.e., at least two intermediate or one severe ratings. Criteria D was used in this analysis as the measure of impairment (15).
Service utilization, private and public sector for emotional, behavioural, psychiatric, and substance use problems in the past 12 months were investigated. School-based services included counselling, special educations, or other interventions for behavioural issues were also taken into account. Formal mental health services included both inpatient psychiatric treatment and outpatient treatment by a mental healthcare professional. Other medical services were defined as care delivered by the formal healthcare system that was not provided by a mental healthcare professional. Social services included institutions that provide assistance for behavioural or emotional problems outside the healthcare system or schools, such as a juvenile program, prison, or family programs. Other services include counselling from religious leaders, traditional or other healers, as well as social groups. Information about use of mental health services were based on the Service Assessment for Children and Adolescents [SACA] [17]. This instrument was developed jointly by Washington and UCLA Universities. It assesses the types of mental health services children use, the treatments they receive within service settings, the reasons for service use, and the quality of such services. The instrument proved to be reliable by indicating high concordance between parents and children or youths reports. The Spanish version was developed in Puerto Rico by Canino el al. [13].
In addition, family functioning was examined by means of the 12- item global functioning scale of the Family Assessment Device (FAD) [18]. This is a 60-item self-report questionnaire developed to assess the six dimensions of the McMaster Model of Family Functioning. Reliability and validity has been documented for all its scales. It has been translated into the respective languages in many countries and used to differentiate functional from dysfunctional families in nonclinical and clinical samples. It was adapted and validated for Chile by a joint working group from the Universities of Navarra Spain, and Los Andes, Chile. In this research we used a sub-scale, which measures overall health or pathology in the family [19].
Family psychiatric history was obtained using the Family History Screen [20]. It is a brief questionnaire collecting lifetime information about 15 psychiatric disorders and suicide in respondents and firstdegree relatives. It was validated by many research teams and tested in the Columbia University of New York for main psychiatric diagnoses. Family income was measured on the basis of the amount in which the family was above the poverty line as defined in Chile on November 2009 in $4.249.46 US per year in rural areas, and $6,334.32 U.S. in urban areas. The family income was analyzed as a categorical variable: poverty > 2 =family income twice over poverty line]; poverty > 5 [5 times over poverty line]; poverty > 8 [income 8 times over poverty line]. Homes where participation was refused were not replaced; replacement was performed only for those homes without children or adolescents.
Statistical analyses: The additional data collected that were not part of the DISC-IV were entered into a STATA 11.0 database (STATA Corp LP, College Station, TX), using double digitations for quality control. Data were entered twice and then paired in order to detect eventual inconsistencies. If these inconsistencies reached more than 4%, the variable was re-entered. DISC-IV yields 12 months DSM-IV diagnoses. Prevalence rate estimates and the corresponding standard errors were obtained using STATA computer program and the complex sample design.
Logistic regression was used to examine association of mental disorders with socio-demographic variables and other potential risk factors. The predictors tested were: age [childhood vs. adolescence], gender, income status of the family, family psychopathology, perception of family functioning, with whom the child lives, school dropout, maltreatment, sexual abuse, severe family illness and death of a near relative. First-order Taylor series linearization was used to calculate odds ratios, 95% confidence intervals, and p values. In order to analyse the effect on prevalence of all predictors that were studied, a multivariate logistic regression analysis was performed. When implementing this analytic strategy, we followed recommendations proposed by Heeringa, West and Berglund, [21]. Thus, a bivariate analysis was firstly performed between each one of the predictors and the criteria variables [diagnosis]. In the case of a categorical predictor [poverty, family structure], bivariate analyses were carried out using F Rao Scott association test, selecting the predictors that showed significance value of p<0.25. This level of significance is recommended when many variables are placed in a bivariate analysis, as a first step of selection. On the other hand, for numerical predictors, a logistic regression analysis was used, selecting predictors with p<0.05. In the next step, a logistic regression was carried out using only those predictors selected in the former stage. For each variable, significance level of p<0.05, p<0.01 or p<0.001 were selected.
Results
The overall prevalence of psychiatric disorders plus disability was 22.5%. Considering broad categories, disruptive disorders showed the highest prevalence [14.6%, SE=1.1] and Anxiety disorders showed the second prevalence rates [8.3%, SE=0.9]. Depressive disorder rates were 5.1% [SE=0.9]. The rest of the disorders showed low prevalence (Table 1). The most prevalent specific anxiety disorder evaluated was Separation Anxiety [4.8%, SE=0.6]. Social phobia rates were 3.7%, SE=0.8 and Generalized Anxiety 3.2%, SE=0.5. In a descriptive preliminary analysis by age and gender, the three anxiety disorders were found to be more prevalent in females. Separation Anxiety was higher in adolescents than children, social phobia was equally prevalent in children and adolescents, and generalized anxiety disorders were slightly higher in children (Table 2).
| Psychiatric disorder + impairment D | % | SE |
|---|---|---|
| Anxious disorders | 8.3 | 0.9 |
| Depressive disorders | 5.1 | 0.9 |
| Disruptive disorders | 14.6 | 1.1 |
| Substance use/abuse | 1.2 | 0.4 |
| Feeding disorders | 0.2 | 0.1 |
| Schizophrenia | 0.1 | 0.1 |
| Any disorder | 22.5 | 1.6 |
Table 1: 12 -month prevalence rates of psychiatric disorders including impairment in Chile. N=1558.
| Total | Male | Female | Age 4-11 | Age 12-18 | |
|---|---|---|---|---|---|
| % SE | % SE | % SE | % SE | % SE | |
| Any of the three anxiety disorders | 8.3 0.9 | 5.8 0.9 | 11.0 1.7 | 9.2 1.1 | 7.4 1.4 |
| Social Phobia | 3.7 0.8 | 1.8 0.7 | 5.7 1.5 | 3.5 0.9 | 3.9 1.2 |
| Generalized anxiety disorder | 3.2 0.5 | 1.2 0.5 | 5.3 0.9 | 3.8 1.0 | 2.6 1.0 |
| Separation anxiety disorder | 4.8 0.6 | 4.0 0.8 | 5.7 0.9 | 6.1 0.9 | 3.4 1.0 |
| Total | Male | Female | Age 4-11 | Age 12-18 |
Table 2: 12-month prevalence rates of anxiety disorders including impairment in Chile. N= 560.
The statistical significance of these differences was calculated in the bivariate and logistic multivariate regressions that followed.
The results of the bivariate analysis of associated factors showed that feminine gender was a risk factor for Social Phobia and GAD but not for Separation Anxiety [O.R.=1.36, C.I.=0.73-2.52]. Age differences did not reach significance in the bivariate analysis for any of the three disorders, therefore were not included in the logistic regression. Having a family income 5 times higher than poverty line was protective for any anxiety and SAD. Income 8 times over poverty cut-off protected from any anxiety and GAD. A positive evaluation of family functioning lowered the risk for all anxiety disorders except GAD. Family psychopathology increased the risk for SAD. Living in a one-parent family was a risk factor for GAD, and living with other persons predisposed to social phobia. Maltreatment increased the risk for all anxiety disorders and sexual abuse to all except GAD. Stressful situations such as severe illness or death of a relative did not increase risk for any anxiety disorders, nor did school dropout (Table 3a).
| Any anxiety | Social Phobia | GAD | Separation anxiety disorder | Any disorder | |
|---|---|---|---|---|---|
| F (OR) | F (OR) | F (OR) | F (OR) | F (OR) | |
| Gender | 8.76** | 7.66** | 12.39** | 1.83+ | 3.60+ |
| Age | 1.17 | 0.08 | 0.45 | 3.21+ | 15.50*** |
| Poverty | 4.24* | 1.38 | 2.22+ | 2.05+ | 0.21 |
| Family psychopathology | 10.72** | 2.91+ | 3.57+ | 4.97* | 59.18*** |
| Family structure | 4.44* | 2.66+ | 3.65* | 2.80+ | 18.09*** |
| School dropout | 0.67 | 1.23 | 0.01 | 0.06 | 0.53 |
| Family functioning | (0.45)** | (0.31)*** | (0.41)+ | (0.49)* | (0.48)*** |
| Maltreatment | (2.67)*** | (2.46)* | (2.39)* | (2.47)* | (4.67)*** |
| Sexual abuse | 22.54*** | 8.47** | 2.03+ | 5.92* | 22.89*** |
| Severe family illness | 1.25 | 0.71 | 0.27 | 0.32 | 1.17 |
| Death of near relative | 0.37 | 0.04 | 0.21 | 0.11 | 1.67+ |
a: F Rao-Scott test; b: Odds Ratio, logistic regression
+: p < 0.25; *: p < 0.05; **: p < 0.01; ***: p < 0.001
Table 3a: Bivariate analysis between predictors and anxiety diagnoses.
In the logistic regression analysis (Table 3b) feminine gender maintained the effect of increasing risk for Social phobia [O.R= 2.83, C.I.=1.09-7.35, p<0.05] and GAD [O.R= 4.16, C.I.=1.59-10.94, p<0.01]. Income 5 times [O.R.=0.37, C.I.=0.18-0.76, p=0.01] or 8 times above the poverty line [O.R.= 0.35, C.I.=0.15-0.83, p=0.05] had a protective effect for Separation Anxiety. Family psychopathology was a risk factor for any of the three anxiety disorders [O.R. 2.93, C.I. 1.29-6.65, p<0.05], but not for specific disorders. Living with only one parent increased risk for GAD [O.R.=2.27, CI=1.20-4.28, p=00.05]. A positive perception of family functioning proved to be protective for social anxiety [O.R.=0.45, C.I.=0.22-0.89, p=0.05]. Maltreatment did not increase risk, but sexual abuse increased risk for any of the three anxiety disorders [O.R.=2.21, C.I.=1.18-4.13, p=0.05].
| Any anxiety | Social Phobia | GAD | Separation anxiety disorder | Any disorder | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | IC | OR | IC | OR | IC | OR | IC | OR | ||
| Gender | ||||||||||
| Male | 1 | 1 | 1 | 1 | 1 | |||||
| Female | 1.80* | (1.09-2.99) | 2.83* | (1.09-7.35) | 4.16** | (1.59-10.94) | 1.36 | (0.73-2.52) | 1.38 | |
| Age | ||||||||||
| 4-11 | - | - | - | - | - | - | 1 | 1 | ||
| Dec-18 | 0.43 | (0.18-1.03) | 0.40*** | |||||||
| Income (poverty line) | ||||||||||
| <= 2 | 1 | - | - | 1 | 1 | - | ||||
| > 2 | 0.56 | (0.29-1.10) | 0.6 | (0.20-1.84) | 0.51 | (0.20-1.26) | ||||
| > 5 | 0.37** | (0.18-0.76) | 0.44 | (0.12-1.63) | 0.27* | (0.08-0.92) | ||||
| > 8 | 0.35* | (0.15-0.83) | 0.23 | (0.05-1.06) | 0.39 | (0.13-1.14) | ||||
| Family psychopathology | 1 | 1 | 1 | 1 | 1 | |||||
| Yes | 2.93* | (1.29-6.65) | 1.82 | (0.67-4.92) | 3.7 | (0.78-17.57) | 3.02 | (0.84-10.90) | 2.48*** | |
| Lives with | ||||||||||
| Both parents | 1 | 1 | 1 | 1 | 1 | |||||
| One parent | 1.65 | (0.92-2.97) | 1.97 | (0.72-5.41) | 2.27* | (1.20-4.28) | 1.4 | (0.65-3.03) | 2.22*** | |
| Others | 2.01 | (0.86-4.70) | 2.79 | (0.76-10.17) | 2.4 | (0.41-13.96) | 2.16 | (0.81-5.76) | 1.61 | |
| Positive evaluation of family functioning | ||||||||||
| 0.67 | (0.38-1.20) | 0.45* | (0.22-0.89) | 0.64 | (0.16-2.58) | 0.68 | (0.29-1.56) | 0.67* | ||
| Maltreatment | 1.29 | (0.57-2.89) | 0.84 | (0.20-3.55) | 1.18 | (0.47-2.98) | 1.59 | (0.48-5.22) | 3.23** | |
| Sexual abuse | 2.21* | (1.18-4.13) | 2.37 | (0.62-9.10) | 1.23 | (0.21-7.34) | 2.05 | (0.81-5.17) | 2.60*** | |
| Death of relative | ||||||||||
| No | - | - | - | - | - | - | - | - | 1 | |
| Yes | 0.81 | |||||||||
-: predictor excluded in bivariate analysis
*: p < 0.05; **: p < 0.01; ***: p < 0.001
Table 3b: Multivariate logistic regression for anxiety diagnoses (plus impairment D). N=560.
There was high comorbidity among Anxiety disorders. The most prevalent association was GAD and SAD, followed by GAD and Social Phobia (Table 4a).
| Social phobia | Separation anxiety | Generalized Anxiety | |
|---|---|---|---|
| Social phobia(N=58) | ------- | 32.30% | 30.50% |
| Separation anxiety (N=76) | 24.60% | ------- | 38.10% |
| Generalized anxiety (N=51) | 34.80% | 57.10% | ------- |
Table 4a: Percentage of Comorbidity between anxious disorders.
Comorbidity along with other disorders was also very high. Social Anxiety showed the highest comorbidity: 49.8% with disruptive disorders and 39.5% with depressive disorders. GAD showed 39.1% comorbidity with disruptive disorders and 38.4% with depressive disorders. Separation Anxiety was comorbid with Depressive disorders in 28.9%, and with disruptive disorders in 24.7%. Having any of the three anxious disorders showed 4.6% comorbidity with substance abuse (Table 4b).
| Depressive | Disruptive | Substance abuse | |
|---|---|---|---|
| Disorders | |||
| Any anxious disorder | 36.1 | 35.6 | 4.6 |
| Social phobia | 39.5 | 49.8 | 0 |
| Generalized anxiety disorder | 38.4 | 39.1 | 0 |
| Separation anxiety | 28.9 | 24.7 | 0.8 |
Table 4b: Percentage of comorbidity among anxiety disorders and other groups of
disorders (with impairment D). N=560.
There were no significant differences among the different anxiety diagnoses regarding service use (Table 5). 41.7% of the children with any of the three anxiety disorders attended some service for their care, compared to 21.5% with other diagnoses [O.R.=2.64, C.I.=1.37-5.08, p<0.01].
| School | Mental Health | Other Medical | Social Service | Other Service | Total Service | |
|---|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Any anxious disorder | 1.04 (0.48-2.26) | 0.93 (0.48-1.79) | 0.62 (0.10-3.90) | -- | 0.60 (0.27-1.31) | 1.02 (0.53-1.95) |
| Social phobia | 1.32 (0.44-3.98) | 1.47 (0.65-3.34) | 1.35 (0.24-7.67) | -- | 0.11 (0.01-1.11) | 1.23 (0.53-2.88) |
| Generalized anxiety | 0.63 (0.19-2.07) | 1.40 (0.45-4.35) | 1.00 (0.12-8.32) | -- | 1.26 (0.30-5.28) | 1.12 (0.43-2.95) |
| Separation anxiety | 1.14 (0.48-2.69) | 1.47 (0.65-3.30) | 1.41 (0.22-8.93) | -- | 1.19 (0.50-2.84) | 1.43 (0.62-3.28) |
*: p < 0.05
Table 5: Relationship between anxiety disorders (plus impairment) and service use. N= 560.
The most used were services delivered in the school system [22.3%], compared to 11.0% of children with other non-anxious disorders [O.R.= 2.32, C.I.=1.03-5.25, p<0.05]. The second most used services were those delivered in specialized mental health facilities: 18.4% vs. 8.5% used by children and adolescents with other diagnoses [O.R.=2.44, C.I.=1.39-4.29, p<0.01]. They attended other medical services only in 4% of the cases, compared to 1% used by children with other psychiatric diagnoses (Table 6).
| Disorders | School | Mental Health | Other Medical | Social | Other | Total |
| % | % | % | % | % | % | |
| OR (CI) | OR (CI) | OR (CI) | OR (CI) | OR (CI) | OR (CI) | |
| Non-Anxiety | 11.00% | 8.50% | 2.90% | 0.40% | 2.10% | 21.50% |
| 1 | 1 | 1 | ------- | 1 | 1 | |
| Anxiety | 22.30% | 18.40% | 4.40% | 0.00% | 3.80% | 41.90% |
| 2.32* (1.03-5.25) | 2.44** (1.39-4.29) | 1.54 (0.29-8.10) | ------ | 1.88 (0.62-5.64) | 2.64** (1.37-5.08) | |
| *p<0.05 | **p<0.01 |
Table 6: Comparisons of service use for anxiety disorders vs. other non-anxiety disorders (N=1558).
Discussion
In this study, we report a prevalence of 8.3% in Separation Anxiety, social anxiety and generalized anxiety disorders within a study of a broad range of psychiatric disorders in Chilean children and adolescents [22]. As only those three anxiety disorders were evaluated, we cannot compare with “any anxiety “reported in other studies. Only some studies report prevalence of specific narrow categories of anxiety disorders. Studies also show differences in the time lapse evaluated, ages of the children and adolescents, and instruments used for calculating prevalence.
The prevalence rates found for the three anxiety disorders in Chile are higher than most other studies, whatever instrument used as evaluation tools. However, rates for social phobia are lower than the United States and Mexico. The three anxiety disorders evaluated in this study are more prevalent in girls than in boys, coinciding with all the other studies [3,13,24,26,30,31].
Our results indicate that anxiety disorders taken as a group are the second most prevalent disorders. On the other hand, disruptive disorders are higher. This finding is similar to that from Puerto Rico [13] and North Carolina [30], but different from the NCSR-A in the United States [3] and Mexico City [30] where Anxiety disorders were the more prevalent psychopathology and in Bangladesh [23] these two groups have similar prevalence.
In the current study we found several risk and protective factors in the bivariate analysis, but some of them lost significance on the logistic regression. Feminine gender remained significant as a risk factor for Social phobia and GAD, family psychopathology and sexual abuse for any anxiety disorder, and living with one parent for GAD. Higher family income retained the protective effect for SAD and the child’s perception of good family functioning lowered risk for social phobia. Reviews of Epidemiology of anxiety disorders in children and adolescents report predictors for anxiety disorders that were also found in our study: low household income, family psychopathology and a history of neglect or abuse [5,6]. The exception is ethnicity, which we did not evaluate as an associated factor. The NCS-A study, Mexico City and Puerto Rico study found no interaction between individual and parental demographic correlates and anxiety disorders except gender and age [3,13,30].
Meta-analysis of comorbidity for anxiety disorders conclude that there is high comorbidity between GAD and Depression, among the phobias and GAD with Social phobia. They also document comorbidity of anxiety disorders in general with disruptive disorders [9,12]. Our findings of high comorbidity among all the different anxiety disorders as well as affective and disruptive disorders coincide with those reports. Comorbidity between anxiety disorders and substance abuse was lower than other studies, and can be explained by our lower rates of substance abuse [3,13].
Of the children with impairing anxiety disorders, 41.9 looked for assistance: 22.3% in school and 18.4% in mental health services. In the British Child and Adolescent Mental Health Survey, 58% of the children and adolescents with diagnosed psychiatric disorders had been in contact with social, special needs, educational, justice or mental health services, but only 23% had been assisted in mental health services [32]. In the National comorbidity Survey-Adolescent Supplement, 36,2% of US adolescents with psychiatric diagnoses received services for their illness, whereas 17.8% with anxiety disorders received assistance: social phobia 12.15%, SAD 8.8% and GAD 43.8%. Treatment for Anxiety disorders tended to increase with age and minority ethnic groups received less assistance than their white counterparts. Specialized mental health services were the main locus of mental health care, although school based services were also important treatment settings. [33]. In Puerto Rico, 49.6% of children with psychiatric disorder plus severe impairment received assistance [13]. In North Carolina, 6.0% of children with psychiatric diagnoses had used some service for mental care in the last three months. Behavioural diagnoses used more services than Depression or anxiety and the school was the most widespread provider of mental health services [30]. In Mexico City, 13.7% of children with a DSM-IV diagnosis had received services for mental health. Those with substance abuse reported the highest service use, and anxiety disorders the lowest. Health based services were the most frequent, mainly specialized in mental health, while school based services were the second most used [34].
In a survey on 66 countries carried out by WHO it was reported that only seven of them provided mental health continued care, but all reported that schools were an important entry point for child mental health services [35]. This organization issued a plan to improve assistance for mental health problems in general. Other studies have reported lower rates of service use in developed countries [36]. In a review of the global mental health gap in services, the World Health Association reports that it exceeds 50% in all countries of the world, reaching up to 90% in the least developed countries [37-39].
In our sample, other medical facilities including primary care are of less importance in treatment of anxiety disorders, and social services practically do not intervene. This reflects the weakness of mental health resources in other levels of medical care apart from specialized units, and the scarce participation of social workers in mental health programs in the country. It also underlines the lack of training in mental health actions for non-specialized professionals in Chile. Nevertheless, children suffering from anxious disorders are being treated more than children with other type of psychopathology in our country.
The results of this study should be analysed taking into consideration its strengths and weaknesses. The main assets are the community setting, strict methodology, use of several internationally validated measurements, adequate sample size and broad age range included. The design is cross-sectional, evaluating the past 12 months, so there is no follow up and no conclusions can be made of development in time. The inclusion of only one informant probably affects prevalence, as it happens with most of the published surveys. Another possible weakness is that we did not add a second impairment measure apart from the one contained in the DISC-IV interview, which could have lowered the prevalence. The exclusion of other anxiety diagnoses leads to under estimation of the real prevalence of “any anxiety disorders”.
To our knowledge, this is one of the few reports on epidemiology of categorical psychiatric disorders in the community in a Latin American country in a large comprehensive sample. Another large research is the Mexican study, a comprehensive analysis of a very big city [31]. Thus, we expect to have made a contribution to trans-cultural psychiatric epidemiology [35-37]. Global results and further analyses on ADHD have been published [22,40].
Summary
Our findings show that anxiety disorders have high prevalence rates in Chile, and should be a concern for health and educational authorities. Correlates are similar to those reported in meta-analyses of epidemiological studies in other countries where socioeconomic and family factors were shown to increase risk [5,6]. Comorbidity rates are also similar to other studies [2,5-7,9]. Service provision is similar to other reports, which add to the existing world-wide gap in assistance. The data from this research is being considered for planning in the ministries of Health and Education, as well as in local programs. The information presented can contribute to the improvement of mental health programs in our country, where a strong, though under financed public health system assists nearly 70% of the population. The private practice is under served too, as insurance companies deliver insufficient reimbursement, compared to physical illness. Our findings of service use by anxious children and adolescents needs to be taken into account in order to provide more assistance in primary care, accompanied by continuous training done by mental health specialists, with the aim of reducing the gap. The information can also be relevant for the educational public system, where some preventive mental health programs are given, as well as remedial education. Coordination between health and education systems shows much need for improvement. Epidemiological studies of psychiatric disorders in children and adolescents in developing countries are scarce, and this is also the situation in Latin America. Therefore, we hope to add to the current knowledge on the topic. For global mental health initiatives, it is important that developing countries contribute with relevant information.
Acknowledgements
This study was funded by the National Science and Technology Research Fund (FONDECYT) Grant Nº 1070519.
Conflicts of interest
The authors declare they have no conflicts of interest
References
- Copeland W, Shanahan L, Costello EJ, Angold A (2011) Cumulative prevalence of psychiatric disorders by young adulthood: a prospective cohort analysis from the Great Smoky Mountains Study. J Am Acad Child Adolesc Psychiatry 50: 252-261.
- Merikangas KR, Nakamura EF, Kessler RC (2009) Epidemiology of mental disorders in children and adolescents. Dialogues ClinNeurosci 11: 7-20.
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, et al. (2010) Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication--Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry 49: 980-989.
- American Psychiatric Association (2000) Diagnostic and Statistical Manual of mental Disorders. Fourth Revision.
- Beesdo K, Knappe S, Pine DS (2009) Anxiety and anxiety disorders in children and adolescents: developmental issues and implications for DSM-V. PsychiatrClin North Am 32: 483-524.
- Beesdo-Baum K, Knappe S (2012) Developmental epidemiology of anxiety disorders. Child AdolescPsychiatrClin N Am 21: 457-478.
- Achenbach TM, Rescorla LA, Ivanova MY (2012) International epidemiology of child and adolescent psychopathology I: diagnoses, dimensions, and conceptual issues. J Am Acad Child Adolesc Psychiatry 51: 1261-1272.
- Clauss JA, Blackford JU (2012) Behavioral inhibition and risk for developing social anxiety disorder: a meta-analytic study. J Am Acad Child Adolesc Psychiatry 51: 1066-1075.
- Costello EJ, Egger HL, Angold A (2005) The developmental epidemiology of anxiety disorders: phenomenology, prevalence, and comorbidity. Child AdolescPsychiatrClin N Am 14: 631-648, vii.
- Fox NA, Pine DS (2012) Temperament and the emergence of anxiety disorders. J Am Acad Child Adolesc Psychiatry 51: 125-128.
- Bittner A, Egger HL, Erkanli A, Jane Costello E, Foley DL, et al. (2007) What do childhood anxiety disorders predict? J Child Psychol Psychiatry 48: 1174-1183.
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A (2003) Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry 60: 837-844.
- Canino G, Shrout PE, Rubio-Stipec M, Bird HR, Bravo M, et al. (2004) The DSM-IV rates of child and adolescent disorders in Puerto Rico: prevalence, correlates, service use, and the effects of impairment. Arch Gen Psychiatry 61: 85-93.
- Patel V, Maj M, Flisher AJ, De Silva MJ, Koschorke M, et al. (2010) Reducing the treatment gap for mental disorders: a WPA survey. World Psychiatry 9: 169-176.
- Shaffer D, Fischer P, Lucas CP, Dulcan MK, Schwab-Stone ME (2000) NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry 39: 28-38.
- SaldiviaS, Vicente B, Valdivia M, Zúñiga M, Llorente et al. (2008) Validación de la entrevistadiagnósticaestructurada DISC-IV para la identificación de trastornospsicopatológicos en niños y adolescenteschilenos. Rev ChilNeuro-Psiquiat 62, 86.
- Stiffman AR, Horwitz SM, Hoagwood K, Compton W 3rd, Cottler L, et al. (2000) The Service Assessment for Children and Adolescents (SACA): adult and child reports. J Am Acad Child Adolesc Psychiatry 39: 1032-1039.
- Epstein NB, Baldwin MN, Bishop DS (1983) The Mc Master Family Assessment Device. J Marital FamTher 9: 171–180.
- Barroilhet S, Cano-Prous A, Cervera-Enguix S, Forjaz MJ, Guillén-Grima F (2009) A Spanish version of the Family Assessment Device. Soc Psychiatry PsychiatrEpidemiol 44: 1051-1065.
- Weissman MM, Wickramaratne P, Adams P, Wolk S, Verdeli H, et al. (2000) Brief screening for family psychiatric history: the family history screen. Arch Gen Psychiatry 57: 675-682.
- Heeringa S West B, Berglund P (2010) Applied survey data analysis. Boca Raton, FL: CRC Press.
- Vicente B, Saldivia S, de la Barra F, Kohn R, Pihan R, et al. (2012) Prevalence of child and adolescent mental disorders in Chile: a community epidemiological study. J Child Psychol Psychiatry 53: 1026-1035.
- Mullick MS, Goodman R (2005) The prevalence of psychiatric disorders among 5-10 year olds in rural, urban and slum areas in Bangladesh: an exploratory study. Soc Psychiatry PsychiatrEpidemiol 40: 663-671.
- Roberts RE, Roberts CR, Xing Y (2006) Prevalence of youth-reported DSM-IV psychiatric disorders among African, European, and Mexican American adolescents. J Am Acad Child Adolesc Psychiatry 45: 1329-1337.
- Carter A,Wagmiller R, Gray S, McCarthy K, Horwitz S et al. (2010) Prevalence of DSM-IV Disorder in a Representative, healthy Birth cohort at School Entry: sociodemographic risks and Social Adaptation. J Am Acad Child Adolesc Psychiatry 49: 686-698.
- Ford T, Goodman R, Meltzer H (2003) The British Child and Adolescent Mental Health Survey 1999: the prevalence of DSM-IV disorders. J Am Acad Child Adolesc Psychiatry 42: 1203-1211.
- Fleitlich-Bilyk B1, Goodman R (2004) Prevalence of child and adolescent psychiatric disorders in southeast Brazil. J Am Acad Child Adolesc Psychiatry 43: 727-734.
- Farbstein I, Mansbach-Kleinfeld I, Levinson D, Goodman R, Levav I, et al. (2010) Prevalence and correlates of mental disorders in Israeli adolescents: results from a national mental health survey. J Child Psychol Psychiatry 51: 630-639.
- Heiervang E, Stormark KM, Lundervold AJ, Heimann M, Goodman R, et al. (2007) Psychiatric disorders in Norwegian 8- to 10-year-olds: an epidemiological survey of prevalence, risk factors, and service use. J Am Acad Child Adolesc Psychiatry 46: 438-447.
- Angold A, Erkanli A, Farmer EM, Fairbank JA, Burns BJ, et al. (2002) Psychiatric disorder, impairment, and service use in rural African American and white youth. Arch Gen Psychiatry 59: 893-901.
- Benjet C, Borges G, Medina-Mora ME, Zambrano J, Aguilar-Gaxiola S (2009) Youth mental health in a populous city of the developing world: results from the Mexican Adolescent Mental Health Survey. J Child Psychol Psychiatry 50: 386-395.
- Ford T, Hamilton H, Goodman R, Meltzer H (2003) Service Contacts Among the Children Participating in the British Child and Adolescent Mental Health Surveys. Child Adolesc. MentHealth 10: 2-9.
- Merikangas KR, He JP, Burstein M, Swendsen J, Avenevoli S, et al. (2011) Service utilization for lifetime mental disorders in U.S. adolescents: results of the National Comorbidity Survey-Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry 50: 32-45.
- Borges G, Benjet C, Medina-Mora M, Orozco R, Wang P (2008) Treatment of mental disorders for adolescents in Mexico City. Bull World Health Organ 86: 757-764.
- World Health Organization (2005) Child mental health services: global concerns-implications for the future. Geneva.
- Sourander A, MultimAki P, Santalahti P, Parkkola K, Haavisto A, et al. (2004) Mental health service use among 18-year-old adolescent boys: a prospective 10-year follow-up study. J Am Acad Child Adolesc Psychiatry 43: 1250-1258.
- World Health Organization (2008) Mental Health Gap Action Program (mhGAP): scaling up care for mental, neurological and substance abuse in low and middle income countries. Geneva.
- Kieling C, Rohde LA (2012) Going global: epidemiology of child and adolescent psychopathology. J Am Acad Child Adolesc Psychiatry 51: 1236-1237.
- Vostanis P (2007) Child Mental Health Services Across the World: Opportunities for Shared Learning. Child AdolescMent Health 12:113-114
- De la Barra FE, Vicente B, Saldivia S, Melipillan R (2013) Epidemiology of ADHD in Chilean children and adolescents. AttenDeficHyperactDisord 5: 1-8.
Relevant Topics
- Adolescent Anxiety
- Adult Psychology
- Adult Sexual Behavior
- Anger Management
- Autism
- Behaviour
- Child Anxiety
- Child Health
- Child Mental Health
- Child Psychology
- Children Behavior
- Children Development
- Counselling
- Depression Disorders
- Digital Media Impact
- Eating disorder
- Mental Health Interventions
- Neuroscience
- Obeys Children
- Parental Care
- Risky Behavior
- Social-Emotional Learning (SEL)
- Societal Influence
- Trauma-Informed Care
Recommended Journals
Article Tools
Article Usage
- Total views: 18789
- [From(publication date):
July-2014 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 14036
- PDF downloads : 4753