Self-reported Mental Health Status in Patients with Acute Coronary Syndrome: A Strong Predictor of Readmission, of Subsequent Anxiety and Depression and of Poor Risk Factor Modification?
Received: 27-Jul-2017 / Accepted Date: 10-Aug-2017 / Published Date: 16-Aug-2017
Abstract
Purpose: The aim of the study was to examine the association between low self-rated mental health before phase II cardiac rehabilitation (CR) and the risk of readmission, anxiety or depression and successful risk factor modification status 12 months after acute coronary syndrome (ACS).
Methods: A prospective follow-up study among patients with ACS verified by angiograms. The patients were 18-80 years of age, had ejection fractions ≥ 40% and had not previously received CR. The patients completed questionnaires on Mental Component Summary (MCS) score and on Hospital Anxiety and Depression Scale (HADS) both before phase II CR, 4 and 12 months after ACS. The patients were assigned into four quartiles according their initial MCS score and compared, using patients in the top quartile as reference group.
Results: At baseline the mean MCS score was 49.5 (SD 11.3) for the 201 included patients. The patients with the lowest MCS score had a higher risk of readmission compared to patients in the highest MCS score quartile (1st vs. 4th quartile) of 52% vs. 28% (OR 0.68, 95% CI 0.52-0.89), anxiety 60% vs. 10% (OR 0.41, 95% CI 0.29-0.56), and depression 44% vs. 0 (OR 0.28, 95% CI 0.17-0.46), respectively, and of achieving recommended blood pressure 62% vs. 82% (OR 0.68, 95% CI 0.51-0.90).
Conclusion: Low self-reported mental health before phase II CR is associated with an increased risk of readmission for cardiovascular disease, for development of anxiety and depression and for not achieving blood pressure targets at 12 months after ACS.
Keywords: Readmission; Mental component summary; Hospital anxiety and depression scale; SF-12
24238Introduction
Cardiac rehabilitation (CR) is the sum activities to help the patients to the best possible physical, mental and social condition after a cardiac event [1]. Non-adherence to exercise-based comprehensive CR is associated with an increased risk of readmission, overall mortality and cardiac mortality [2]. Great effort has been put in trying to increase adherence to CR through addressing barriers of adherence [3] and exploring various models and content of CR, but this has proven an enormous challenge [4].
Myocardial infarction (MI) can affect the self-rated health related quality of life (HRQL) [5] and is also followed by an increased risk of depression [6], anxiety [7] and suicide [8]. Persistent angina symptoms seem to be associated with anxiety and depression [9].
Low mental HRQL post-MI has been associated to young age, low baseline HRQL, sedentary lifestyle, depression and to low social support [10]. Also low self-rated mental health was associated to a reduced probability of returning to work after acute or elective percutaneous coronary intervention [11] plus increased risk of both new cardiovascular events and of death [12].
Simple and accurate screening tools used at best before discharge may help clinicians identify patients who are particularly prone to CR non-adherence and to have a poor outcome following acute coronary syndrome (ACS). Self-rated mental health status can be assessed by using the well-established disease-generic SF-12 questionnaire as the Mental Component Summary (MCS) score [13,14].
The aim of this study was to examine the association between self-rated mental health status based on MCS score before phase II CR and the subsequent risk of readmission, anxiety or depression and risk factor modification status 12 months after ACS.
Materials & Methods
Study design
We designed a follow-up study based on a randomized controlled trial comparing phase II CR in two different settings, providing in principle the same care. Detailed information on the trial protocol and the results has previously been published [15,16].
Setting
Before hospital discharge, our patients were randomized to phase II CR programme either after a shared care model (SC-CR) with the general practitioner in charge of the programme and lifestyle modification lessons at the community-based municipal health care centre or to the usual CR programme within the hospital outpatient clinic (H-CR). The municipalities involved were Aarhus, Viborg, Skive, Silkeborg, Samsoe, Favrskov and Skanderborg all located in the Central Region, Denmark with 660.000 inhabitants. The overall rate of full programme adherence to CR in the SC-CR and H-CR groups were 53% and 54% respectively [17]. Full programme adherence was defined as participation in all components; dietary advice, exercise training, clinical assessment by a doctor, patient education and smoking cessation. (Five of five if smoker, four of four if non-smoker). Participation in one component was defined as attending 50% or more of the sessions in the component.
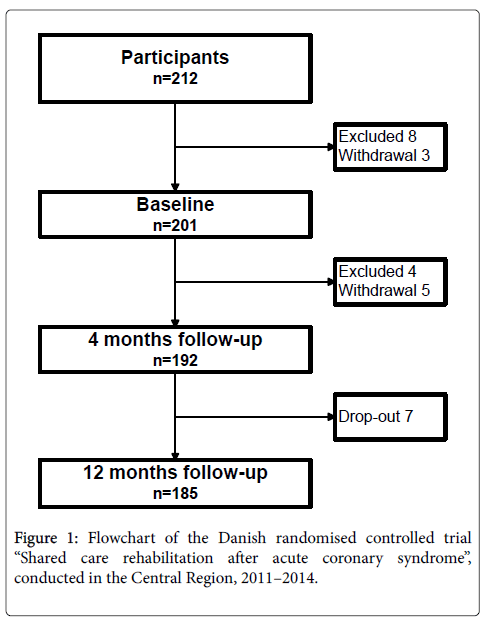
Inclusion lasted from October 10th 2011 to March 24th 2013. Fourmonth follow-up was carried out between February 2nd 2012 and August 31st 2013 as soon as phase II CR was completed or 5 months after admission, if CR was delayed or if bypass surgery was needed. 12 months follow-up was between October 2012 and March 2014. The flowchart of the study population is shown in Figure 1.
Participants
Patients hospitalized due to ACS in four coronary units, two at Aarhus University Hospital and the Central Hospital Unit, Viborg and Silkeborg Regional Hospitals were screened. Inclusion criteria were: admission with ACS, and angiographically documented coronary thrombosis or stenosis, age 18 to 80 years, left ventricular ejection fraction ≥ 40%, no prior CR, no severe physical or mental comorbidity, resident in one of the participating municipalities listed above, and consent to both hospital-based CR and shared care CR before randomisation.
Data
Data were collected prospectively at four times according to protocol: during admission, before the beginning of phase II CR– approximately 2 weeks after discharge, 6 weeks after ACS, when phase II CR was completed (4 months after ACS) and finally 12 months after ACS, as shown in Figure 1. Patients were asked to use internet-based questionnaires, but paper questionnaires were available, if preferred. Reminders were sent by email twice and patients who had still not responded were further encouraged to respond by a telephone call.
The study was conducted in accordance with good clinical practice and with the ethical standards described in the Helsinki declaration. The Central Denmark Region Committees on Biomedical Research Ethics j.nr M-20110135 and the Danish Data Protection Agency approved the study protocol j.nr. 2011-41-6533 changed to 2014-41-3342 in 2014.
Mental health status
Mental health status was estimated by the MCS score and from Hospital Anxiety and Depression Scale (HADS). The MCS score was obtained using the validated Danish version of the disease generic SF-12 version 2 health survey on self-rated health to asses quality of life during the previous 4 weeks [13,14]. SF-12 consists of 12 items and it covers 8 subscales. It can be divided into a physical component summary (PCS) and the MCS. A norm-based scoring algorithm was used to calculate the SF-12 scores. The six items of the PCS are in the computation of the MCS, but it is mainly comprised by the six mental items (‘Vitality’, Social Function’, Role-Emotional’ (2 items) and ‘Mental Health’ (2 items). The construct validity in MCS has been proven good [18].
HADS is a 14-item questionnaire with seven items covering anxiety (HADS-A) and seven items covering depression (HADS-D) during the previous 2 weeks. Each item is answered on a 0-3 rating scale and a total score of 0-21 respectively. Reliability (HADS-D, Cronbach´s α≈0.80) has proven satisfactory in validation of HADS in patients with myocardial infarction [19,20]. A score of HADS-A or HADS-D ≥ 8 six weeks after ACS lead to consult with the doctor in charge of the CR course, since HADS-D ≥ 8 has a 65% sensitivity and 90% specificity in identifying depression among patients with myocardial infarction compared to structured interview with a physician [20].
Clinical data
Data on 24 h ambulatory blood pressure, blood samples, weight, waist circumference, adherence to lifestyle recommendations, and use of preventive medications were obtained from patient files and at follow-up visits. Information on comorbidity and sociodemography was obtained during the primary hospital admission.
Outcomes
Based on the patients’ perceptions of their mental health status two weeks after discharge they were divided into quartiles according to MCS score. The outcome measures during the 12 m after admission for ACS were:
• Readmission for cardiovascular disease (ACS, arrhythmia, stroke, heart failure).
• Anxiety and depression assessed by HADS.
• Risk factor modification on total cholesterol, LDL cholesterol, blood pressure, HbA1c, BMI, waist circumference, smoking status, and physical activity.
Statistical Analysis
Nielsen et al. divided participants into quartiles according to MCS score and demonstrated an association between low MCS score and an increased risk of new cardiovascular events or death [12]. We used the same division into quartiles score (First quartile had the lowest score; fourth quartile had the highest score) to increase clinical interpretability and to investigate if a dose-response relationship could be established.
The association between baseline score of MCS and baseline characteristics was assessed using χ2 statistics for categorical variables, analysis of variance for continuous variables and Kruskal-Wallis tests when conditions for analysis of variance were not fulfilled.
The associations between baseline score of MCS and the risk of readmission, anxiety and depression assessed by HADS and risk factor moderation status at 12 months were analysed using logistic regression with estimation of crude odds ratios, including 95% confidence intervals (95%CI). To examine if the association between low MCS score and the risk of readmission or if risk factor moderation status was mediated through the development of depression or anxiety, we also performed additional analyses after first excluding patients with depression and secondly patients with depression or anxiety. In addition we performed multivariable logistic regression analyses with adjustment for age, sex, vocational education, depression and anxiety using patients in the top half of MCS score as a reference group on the endpoints showing an association to low MCS score when patients with depression or anxiety were excluded (readmission and blood pressure). Patients withdrawing from the study before the baseline visit were censored as withdrawals. Patients lost to follow-up were censored as dropouts.
Data analysis was performed in STATA 12.1.
Results
Table 1 shows the baseline characteristics of the 201 patients included in the analysis by quartiles of baseline MCS score. The overall mean MCS score was 49.5 (SD 11.3). The quartile with the lowest MCS score ranged from 19.3 to 42.3, mean was 34.9. This quartile also scored lowest on the PCS, included more women and had a lower mean age than the quartile with the highest MCS score. More patients from the quartile with lowest MCS score displayed symptoms of anxiety and depression and patients from the lowest quartile were often smokers, were less physical active and more had a waist circumference above the recommendations.
| Baseline score of MCS | |||||
|---|---|---|---|---|---|
| Variables | 1st quartile n=50 | 2nd quartile n=50 | 3rd quartile n=50 | 4th quartile n=51 | p-value |
| Mental health (MCS), mean (min-max) |
34.9 (19.3-42.3) | 47.5 (42.6-53.1) | 57.0 (53.2-60.1) | 63.9 (60.3-70.1) | 0.0001 |
| Physical health (PCS), mean (min-max) |
39.9 (16.8-59.0) | 42.9 (16.7-58.5) | 46.2 (15.4-57.8) | 47.2 (13.3-55.4) | 0.0001 |
| Age, mean (min-max) | 57 (30-78) | 59 (44-77) | 59 (44-79) | 65 (40-77) | 0.0023 |
| Sex, (males %) | 62 | 70 | 80 | 86 | 0.01 |
| Diagnosis (STEMI) | 42 | 52 | 44 | 39 | 0.61 |
| Cohabitation status-alone | 16 | 20 | 18 | 14 | 0.79 |
| Vocational education | 0.48 | ||||
| - None/short courses | 20 | 30 | 18 | 32 | |
| - Handcraft | 31 | 19 | 27 | 23 | |
| - Short and middle | 20 | 31 | 27 | 22 | |
| - High | 24 | 18 | 23 | 35 | |
| Total Cholesterol<4 mmol/l | 24 | 19 | 16 | 12 | 0.19 |
| LDL cholesterol<1.8 mmol/l | 14 | 10 | 10 | 8 | 0.49 |
| HbA1c<6.5% | 82 | 93 | 68 | 81 | 1.00 |
| BP<135/85 mmHg | 74 | 77 | 71 | 76 | 1.00 |
| BMI<30 | 67 | 85 | 82 | 82 | 0.10 |
| Waist M/F<102/88 cm | 36 | 50 | 54 | 61 | 0.02 |
| Smoking at admission | 54 | 50 | 42 | 22 | 0.00 |
| Exercise ≥ 30 min ≥ 5 days/week | 36 | 48 | 42 | 76 | 0.00 |
| HADS-A≥ 8 | 50 | 24 | 5 | 0 | 0.00 |
| HADS-D≥ 8 | 28 | 10 | 5 | 0 | 0.00 |
Table 1: Baseline characteristics and status on lifestyle moderation targets plus symptoms of anxiety/depression of 201 patients admitted with first time acute coronary syndrome in 2011-2013 by quartiles of mental health status (MCS: Mental Component Summary score from the Short-Form 12 V.2). PCS: Physical Component Summary; HADS-A/D ≥ 8; Hospital Anxiety and Depression Scale Anxiety/Depression subscore ≥ 8. BP: 24- hour ambulatory blood pressure, BMI: Body mass index. All variables except for PCS, MCS and age were reported as proportions (%). The associations were assessed using χ2 statistics for categorical variables, analysis of variance for continuous variables and Kruskal-Wallis tests when conditions for analysis of variance were not fulfilled.
Table 2 shows status on the patients 12 months after ACS again according to the baseline score. In the study population anxiety or depression in at least one questionnaire from baseline to 12 months follow-up were reported by 34% (HADS-A ≥ 8) and 22% (HADS-D ≥ 8), respectively, but unevenly distributed between lowest and highest quartile based on MCS score. For anxiety 60% vs. 10% and for depression 44% vs . 0%, respectively. The readmission rate was 38% in total, but 52% in the group with lowest MCS score and 28% in the group with highest MCS score (OR 0.68, (95% CI 0.52–0-89)). A greater percentage of the patients with highest MCS score reached recommended treatment target on blood pressure 82% vs . 62% OR 0.68, (95% CI 0.51–0.90), and on BMI 84% vs . 64% OR 0.68, (95% CI 0.51–0.93). Both PCS and MCS mean score vary, however the ranges overlap.
| Baseline score of MCS in quartiles | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 12 months after acute coronary syndrome | 1st n=50 | 2nd n=50 | 3rd n=50 | 4th n=51 | OR | 95% CI | ||||||
| MCS mean (min-max) | 37.1 (11.2-58.3) | 40.2 (22.1-54.9) | 45.6 (18.9-55.9) | 50.1 (37.3-59.0) | 2.78 | 1.89-4.08 | ||||||
| PCS mean (min-max) | 39.1 (24.4-57.2) | 43.4 (25.3-58.0) | 44.9 (20.9-53.9) | 47.3 (33.3-55.6) | 2.33 | 1.63-3.32 | ||||||
| HADS-A ≥ 8 - 12 months, (%) | 42 | 1.0 | 36 | -0.2 | 17 | -0.6 | 6 | -0.2 | 0.47 | 0.34-0.67 | ||
| - Once during 12 months, (%) | 60 | 48 | 20 | 10 | 0.41 | 0.29-0.56 | ||||||
| HADS-D ≥ 8 - 12 months, (%) | 20 | 0.5 | 9 | -0.2 | 6 | -0.2 | 0 | 0 | 0.39 | 0.22-0.71 | ||
| - Once during 12 months, (%) | 44 | 16 | 10 | 0 | 0.28 | 0.17-0.46 | ||||||
| Readmission, (%) | 52 | 44 | 28 | 28 | 0.68 | 0.52-0.89 | ||||||
| Total Cholesterol<4 mmol/l, (%) | 61 | -1.2 | 64 | -1.1 | 65 | -1.1 | 74 | -1.2 | 0.83 | 0.63-1.09 | ||
| LDL cholesterol<1.8 mmol/l, (%) | 50 | -0.9 | 30 | -1.1 | 45 | -1.2 | 41 | -1.1 | 1.05 | 0.81-1.36 | ||
| HbA1c<6.5%, (%) | 92 | 0.2 | 80 | 0.5 | 91 | 0.1 | 84 | 0.3 | 1.13 | 0.76-1.68 | ||
| BP<135/85 mmHg, (%) | 62 | 3.1 | 53 | 4.4 | 68 | -0.7 | 82 | 0 | 0.68 | 0.51-0.90 | ||
| BMI<30, (%) | 64 | -0.2 | 79 | 0 | 76 | 0.3 | 84 | -0.5 | 0.68 | 0.51-0.93 | ||
| Waist M/F<102/88 cm, (%) | 39 | -2.4 | 57 | -1.3 | 58 | -1.0 | 70 | -2.3 | 0.72 | 0.55-0.94 | ||
| Daily smoking, (%) | 20 | -34 | 26 | -24 | 21 | -21 | 10 | -12 | 0.80 | 0.57-1.11 | ||
| Physical activity ≥ 30 min ≥ 5 days/week, (%) | 36 | 0.6 | 44 | 0.2 | 47 | 0 | 48 | -1.0 | 0.85 | 0.66-1.10 | ||
Table 2: Association between baseline mental health status (Mental Component Summary (MCS) score of SF-12) and status on adherence to the components of cardiac rehabilitation and on readmission, anxiety, depression and on lifestyle moderation targets 12 months after acute coronary syndrome. HADS-A/D ≥ 8; Hospital Anxiety and Depression Scale Anxiety/Depression subscore ≥ 8, BP: 24 h ambulatory blood pressure, BMI: Body mass index. The second number in the columns is the change from baseline to 12 months. Changes from baseline are reported in percentages. We used logistic regression analysis with estimation of crude odds ratios, including 95% confidence intervals (95%CI).
In Table 3 first patients with depression and secondly also patients with anxiety were excluded to investigate if low MCS is an independent risk factor. When excluding patients with depression the OR for readmission was 0.74, 95% CI 0.54-1.01) and excluding both anxiety and depression the OR was 0.96, (95% CI 0.66-1.37) for patients with the highest compared to the lowest baseline MCS score. The OR for reaching treatment targets on blood pressure and on BMI only had minor changes although the reduced sample size lead to a lower statistical precision and subsequently statistical non-significant results.
| Comparison of lowest and highest MCS quartile | ||||||
|---|---|---|---|---|---|---|
| 12 months after acute coronary syndrome | No exclusion n=185 (46 vs. 50) OR 95% CI | HADS-D ≥ 8 excluded n=151 (24 vs.50 OR 95% CI | HADS-A/D≥8 excludedn=118 (16 vs. 45) OR 95% CI | |||
| Physical Cumulative Score | 2.33 | 1.63-3.32 | 1.97 | 1.28-3.05 | 1.37 | 0.79-2.37 |
| Readmission | 0.68 | 0.52-0.89 | 0.74 | 0.54-1.01 | 0.96 | 0.66-1.37 |
| Total Cholesterol<4 mmol/l | 0.83 | 0.63-1.09 | 0.90 | 0.66-1.24 | 0.93 | 0.65-1.34 |
| LDL cholesterol<1.8 mmol/l | 1.05 | 0.81-1.36 | 1.07 | 0.79-1.43 | 1.05 | 0.75-1.48 |
| HbA1c<6.5% | 1.13 | 0.76-1.68 | 1.35 | 0.83-2.20 | 1.37 | 0.77-2.44 |
| BP<135/85 mmHg | 0.68 | 0.51-0.90 | 0.65 | 0.47-0.90 | 0.69 | 0.47-1.01 |
| BMI<30 | 0.68 | 0.51-0.93 | 0.72 | 0.51-1.02 | 0.78 | 0.52-1.16 |
| Waist M/F<102/88 cm | 0.72 | 0.55-0.94 | 0.81 | 0.60-1.09 | 0.86 | 0.61-1.21 |
| Smoking at 4 months | 0.80 | 0.57-1.11 | 0.78 | 0.54-1.14 | 0.82 | 0.52-1.27 |
| Physical activity≥ 30 min ≥ 5 days/week | 0.85 | 0.66-1.10 | 0.82 | 0.60-1.11 | 0.73 | 0.50-1.04 |
Table 3: Association between baseline mental health status (Mental Component Summary score of SF-12) and status on readmission and on lifestyle moderation targets 12 months after acute coronary syndrome between lowest and highest MCS quartile. HADS-A/D ≥ 8; Hospital Anxiety and Depression Scale Anxiety/Depression subscore ≥ 8, BP: 24 h ambulatory blood pressure, BMI: Body mass index. With exclusion of HADS-D ≥ 8 and HADS-D ≥ 8 plus HADS-A ≥ 8.
In the multivariable analyses in the supplementary table the baseline MSC score was dichotomized, an association between low MCS score and the risk of readmission and achieving treatment target on blood pressure were seen when adjusting for the potential confounders as age, sex, vocational education, depression and anxiety. The cut point is around 40.
Discussion
In our population, where all patients needing CR were included, we were able to enrol a patient group that to a very high degree reflected the everyday life population seen in a Danish Coronary Unit. We observed that low self-rated MCS score was associated with an increased risk of readmission, anxiety or depression, and reduced risk factor moderation on blood pressure, waist circumference and smoking status 12 months after ACS.
Readmission
Our readmission rate was 38%, but varied from 52% among the patients with low MCS score to 28% among the patients with the highest MCS score. Zwisler et al. found that 28% were readmitted with cardiac disease within 12 months from the index hospitalisation regardless of randomisation to a CR program or usual care [21]. Another study found that a total of 62% of patients were readmitted during the 12 months after ACS and of these, approximately 53% were due to cardiac causes, and more than half were within 30 days [22]. It was concluded that many readmissions were unrelated to the index stay and thus not easy to predict with common clinical variables.
MCS score may reveal causes unrelated to heart disease for readmission. Studies have shown that patients illness perceptions regarding consequences of coronary artery disease contributed substantially to the health related quality of life 6 months later [23]. However the illness perception can be changed after MI during an early intervention and hence increase CR attendance and the understanding of the disease [24]. The intervention group also returned to work earlier than the control group [24]. Albus reported that cognitive-behavioural individual therapy and group training in combination reduced the number of cardiac events [25]. Based on these findings it may be possible that patients with low initial MCS score could benefit from extra cognitive therapy and hence reduce the risk of readmission and increase CR attendance. The CR staff can initiate this.
Anxiety and depression
The association between low MCS score and symptoms of anxiety and / or depression was to be expected since Nielsen et al. had shown the same association [12] however it could not fully explain the results. Pelle et al. showed that anxiety, depression, negative affectivity and social inhibition were distinct constructs, but the items in the HADS questionnaire loaded diffusely instead of clustering together as proposed [26]. We identified 22% with symptoms of depression after ACS, which matches the reported prevalence of 19.8% in post-MI depression diagnosed through clinical interview [27]. A study in ACS-patients had a sensitivity of HADS-A ≥ 8 of 91% and found that 41.4% of patients had HADS-A ≥ 828. The difference may be due to the exclusion criteria in our study i.e. heart failure and severe comorbidity, in which high prevalence of depression were reported [12,28]. However our exclusion criteria may lead to an underestimation of the prevalence of anxiety and depression among the entire population with ACS.
Risk factor reduction
A few previous studies have investigated and found an association between low mental health after MI and the prognosis, disease severity and other clinical risk factors. However different measures of mental health status were used [12,29-31]. Studies have been conducted in various settings as subgroups of women 32, ejection fraction ≤ 30% [29], follow-up of only 6 months [31] or mental health was assessed 5 years or more after MI [29,32]. The studies reported that low mental health status was associated with a higher risk of adverse outcomes. The recent study by Nielsen et al. reported an association between low mental health and risk or death obtained 3 months after MI admission also when adjusting for anxiety and depression. Patients with low mental health status reported lower phase II CR adherence than patients with high mental health status, however the low mental health group contained a higher proportion of patients with heart failure, readmission rate was not reported and only data on smoking status and physical activity of targets directed for risk factor moderation were reported and none of the studies measured mental health status before phase II CR.
In our study the values of total- and LDL-cholesterol decreased throughout the study, as an indication of that adherence to pharmacotherapy was unaffected by the MCS score. Improved risk factor management on total-cholesterol, LDL-cholesterol, systolic blood pressure and BMI among socially vulnerable patients compared to a control group was reported by Nielsen et al. [33] with the intervention was a 1-2 extra individual consultations with a rehabilitation nurse and a follow-up phone consult 2 months after phase II CR [34]. Ho et al. improved medication and secondary prevention measures through a multifaceted intervention containing support from a collective care with pharmacist and physician, pharmacist tailoring, patient education and voice reminders by phone [35]. Both these trials contained individual consultations. Leifheit-Limson et al. found that lower social support is associated with worse health status and more depressive symptoms over the first year of acute myocardial infarction recovery, particularly for women [36]. Hawkes et al. found the predictors of low MCS score 6 months after MI-discharge were younger age, lower baseline MCS, sedentary living, depression and lower social support, but it was not reported, whether low mental health was associated to readmission [10].
Overall the studies agree on a quite high readmission rate not solely related to the cardiac event. There is also a general agreement on predictors of low mental health score, on the importance of finding and treating anxiety or depression and that extra support during CR improve compliance to secondary preventive medications and improved risk factor modification. Systematic assessment of mental health may add to the knowledge of patients that could benefit from extra support to decrease the risk of both readmissions and symptoms of anxiety and depression.
Strengths and limitations
The strengths of the study included the homogeneous study population since we invited all patients with first-time ACS verified by angiogram. They had ejection fraction ≥ 40%, attended CR, had no severe comorbidity, were <80 years old and they have demonstrated the surplus energy to participate the conditions of a randomised controlled trial. Inclusion was performed before hospital discharge, systematic collection of data from three project control visits and follow-up data on 87% of the patients.
The limitations include the fact that the SF-12 deals with the perception on health during the last 4 weeks. In this trial it was completed approximately two weeks after hospitalisation for ACS.
Hawkes et al. also reported MCS and PCS from SF-36 obtained 1-2 weeks after MI discharge and found similar results as stated above [10]. Potentially the self-reported mental health just 2 weeks after ACS was influenced of the cardiac incident and may be reported lower than in patients without ACS, but this was the same in the entire study group. Nevertheless, the average MCS score was highest at baseline and lower at both 4 and 12 months follow-up, which indicates that the baseline MCS score contained information on mental health prior to admission for ACS and a tendency towards reporting a better mental health when evaluating the time just before the index ACS. The effect of low mental health score could have even greater implications if all cardiac patients including heart failure, age ≥ 80 years and more comorbidity reported their mental health. Heart failure seemed to be associated with low mental health in both these Danish studies [11,37] and an increased risk of dying [12].
The study is also limited of being a post-hoc analysis of a RCT powered for measuring a difference in CR adherence. The subgroups is hence quite small and CIs rather wide.
In the supplementary analyses we excluded patients with symptoms of first depression and second depression and anxiety. There was no longer a difference in readmission between patients with the lowest and the highest mental health status, however indications of an association between low MCS score and impaired risk factor management was observed. Confounding was addressed in the supplementary analysis by dichotomising MCS and adjusting for potential confounders, however due to the observational nature of the study, we cannot exclude the possibility of residual or unaccounted confounding factors may still affect the results.
Conclusion
In ACS-patients with preserved left ventricular function, and free of severe comorbidities we found an association between poor self-rated mental health obtained from SF-12 as a low MCS score before phase II CR and the risk of readmission, anxiety or depression and risk factor modification the first year after admission. These points towards a potential role of MCS score as a useful screening tool to identify both patients with need of extra support during CR. More awareness of mental health may improve risk factor moderation and reduce the number of readmissions during the first year after ACS, however further studies on the possible clinical implications of using this tool is clearly required.
Implications for clinicians
• Self-rated mental health by MCS obtained from SF-12 seemed to be a valid screening tool to identify patients at risk of readmission after admission for ACS.
• Low self-rated mental health before phase II cardiac rehabilitation is associated with an increased risk of both readmission for cardiovascular disease and of anxiety or depression and it impaired successful moderation of cardiovascular risk factors.
• Low MCS score should lead to a closer follow-up by a CR team in order to ensure that patients in this category also benefit from CR.
Acknowledgements
The authors would like to thank the patients and the staff of the municipal health care centres and of the hospital rehabilitation units participating in the study as well as the project nurses for their contribution to patient recruitment, intervention and data collection.
Funding
The trial is funded by the Central Region Denmark as a part of the chronic care programme.
Trial registration: clinicaltrials.gov identifier: NTC 01522001
Competing Interests
Authors declare no conflicts of interest.
References
- WHO. World Health Organisation (1993) Needs and action priorities in cardiac rehabilitation and secondary prevention in patients with CHD. Geneva.
- Heran BS, Chen JM, Ebrahim S, Moxham T, Oldridge N, et al. (2011) Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev CD001800.
- Rose M, Timmons SM, Amerson R (2011) Facilitators and barriers in cardiac rehabilitation participation: An integrative review. J Nurse Pract 7: 399-408.
- Jelinek MV, Thompson DR, Ski C, Bunker S, Vale MJ, et al. (2015) 40 years of cardiac rehabilitation and secondary prevention in post-cardiac ischaemic patients. Are we still in the wilderness? Int J Cardiol 179: 153-159.
- Lenzen MJ, Scholte op Reimer WJM, Pedersen SS, Boersma E, Maier W, et al. (2007) The additional value of patient-reported health status in predicting 1-year mortality after invasive coronary procedures: a report from the Euro Heart Survey on Coronary Revascularisation. Heart 93: 339-344.
- Meijer A, Conradi HJ, Bos EH, Anselmino M, Carney RM, et al. (2013) Adjusted prognostic association of depression following myocardial infarction with mortality and cardiovascular events: individual patient data meta-analysis. Br J Psychiatry 203: 90-102.
- Roest AM, Martens EJ, Denollet J, de Jonge P (2010) Prognostic association of anxiety post myocardial infarction with mortality and new cardiac events: a meta-analysis. Psychosom Med 72: 563-539.
- Larsen KK, Agerbo E, Christensen B, Søndergaard J, Vestergaard M (2010) Myocardial infarction and risk of suicide: a population-based case-control study. Circulation 122: 2388–2393.
- Jespersen L, Abildstrøm SZ, Hvelplund A, Prescott E (2013) Persistent angina: Highly prevalent and associated with long-term anxiety, depression, low physical functioning, and quality of life instable angina pectoris. Clin Res Cardiol 102: 571–581.
- Hawkes AL, Patrao TA, Ware R, Atherton JJ, Taylor CB, et al. (2013) Predictors of physical and mental health-related quality of life outcomes among myocardial infarction patients. BMC Cardiovasc Disord 13: 69.
- Biering K, Nielsen TT, Rasmussen K, Niemann T, Hjollund NH, et al. (2012) Return to work after percutaneous coronary intervention: the predictive value of self-reported health compared to clinical measures. PLoS One 7: e49268.
- Nielsen TJ, Vestergaard M, Christensen B, Christensen KS, Larsen KK (2013) Mental health status and risk of new cardiovascular events or death in patients with myocardial infarction: a population-based cohort study. BMJ Open 3: e003045.
- Gandek B, Ware JE, Aaronson NK, Apolone G, Bjorner JB, et al. (1998) Cross-Validation of Item Selection and Scoring for the SF-12 Health Survey in Nine Countries?: Results from the IQOLA Project. J Clin Epidemiol 51: 1171–1178.
- Ware JEJ, Koshiki MM, Keller SD (2014) A 12-Item Short-Form Health Survey?: Construction of Scales and Preliminary Tests of Reliability and Validity. Med Care 34: 1-9.
- Bertelsen JB, Refsgaard J, Kanstrup H, Johnsen SP, Qvist I, et al. (2017) Cardiac rehabilitation after acute coronary syndrome comparing adherence and risk factor modification in a community-based shared care model versus hospital-based care in a randomised controlled trial with 12 months of follow-up. Eur J Cardiovasc Nurs 16: 334-343.
- Bertelsen JB, Refsgaard J, Kanstrup H, Johnsen SP, Qvist I, et al. (2013) Hospital-based versus community-based shared care cardiac rehabilitation after acute coronary syndrome: protocol for a randomized clinical trial. Dan Med J 60: A4699.
- Bertelsen JB, Refsgaard J, Kanstrup H, Johnsen SP, Qvist I, et al. (2017) Cardiac rehabilitation after acute coronary syndrome comparing adherence and risk factor modification in a community-based shared care model versus hospital-based care in a randomised controlled trial with 12 months of follow-up. Eur J Cardiovasc Nurs 16: 334–343.
- Fleishman JA, Selim AJ, Kazis LE (2010) Deriving SF-12v2 physical and mental health summary scores: a comparison of different scoring algorithms. Qual Life Res 19: 231–241.
- Martin CR, Lewin RJP, Thompson DR (2003) A confirmatory factor analysis of the Hospital Anxiety and Depression Scale in coronary care patients following acute myocardial infarction. Psychiatry Res 120: 85–94.
- Thombs BD, Magyar-Russell G, Bass EB, Stewart KJ, Tsilidis KK, et al. (2007) Performance characteristics of depression screening instruments in survivors of acute myocardial infarction: review of the evidence. Psychosomatics 48: 185–194.
- Zwisler A-DO, Soja AMB, Rasmussen S, Frederiksen M, Abedini S, et al. (2008) Hospital-based comprehensive cardiac rehabilitation versus usual care among patients with congestive heart failure, ischemic heart disease, or high risk of ischemic heart disease: 12-Month results of a randomized clinical trial. Am Heart J 155: 1106–1113.
- Southern DA, Ngo J, Martin BJ, Galbraith PD, Knudtson ML, et al. (2014) Characterizing types of readmission after acute coronary syndrome hospitalization: implications for quality reporting. J Am Heart Assoc 3: e001046.
- French DP, Lewin RJP, Watson N, Thompson DR (2005) Do illness perceptions predict attendance at cardiac rehabilitation and quality of life following myocardial infarction? J Psychosom Res 59: 315–322.
- Petrie KJ, Cameron LD, Ellis CJ, Buick D, Weinman J (2002) Changing Illness Perceptions After Myocardial Infarction?: An Early Intervention. Psychom Med 64: 580–586.
- Albus C (2010) Psychological and social factors in coronary heart disease. Ann Med 42: 487–494.
- Pelle AJ, Denollet J, Zwisler AD, Pedersen SS (2009) Overlap and distinctiveness of psychological risk factors in patients with ischemic heart disease and chronic heart failure: are we there yet? J Affect Disord 113: 150–156.
- Thombs B, Bass E, Ford DE, Stewart KJ, Tsilidis KK, et al. (2006) Prevalence of depression in survivors of acute myocardial infarction. J Gen Intern Med 21: 30–38.
- Frasure-Smith N, Lespérance F (2008) Depression and anxiety as predictors of 2-year cardiac events in patients with stable coronary artery disease. Arch Gen Psychiatry 65: 62–71.
- Piotrowicz K, Noyes K, Lyness JM, McNitt S, Andrews ML, et al. (2007) Physical functioning and mental well-being in association with health outcome in patients enrolled in the Multicenter Automatic Defibrillator Implantation Trial II. Eur Heart J 28: 601–607.
- Lim LL, Johnson NA, O’Connell RL, Heller RF (1998) Quality of life and later adverse health outcomes in patients with suspected heart attack. Aust N Z J Public Health 22: 540–546.
- Nelson EC, Ferreira PL, Cleary PD, Gustafson D, Wasson JH, et al. (1994) Do patients’ health status reports predict future hospital stays for patients with an acute myocardial infarction? Fam Pract Res J 14: 119–126.
- Norekvål TM, Fridlund B, Rokne B, Segadal L, Wentzel-Larsen T, et al. (2010) Patient-reported outcomes as predictors of 10-year survival in women after acute myocardial infarction. Health Qual Life Outcomes 8: 140.
- Nielsen KM, Meillier LK, Larsen ML (2013) Extended cardiac rehabilitation for socially vulnerable patients improves attendance and outcome. Dan Med J 60: A4591.
- Meillier LK, Nielsen KM, Larsen FB, Larsen ML (2012) Socially differentiated cardiac rehabilitation: Can we improve referral, attendance and adherence among patients with first myocardial infarction? Scand J Public Health 40: 286-293.
- Ho PM, Lambert-Kerzner A, Carey EP, Fahdi IE4, Bryson CL, et al. (2014) Multifaceted intervention to improve medication adherence and secondary prevention measures after acute coronary syndrome hospital discharge: a randomized clinical trial. JAMA Intern Med174: 186-193.
- Leifheit-Limson E, Reid K, Kasl SV, Lin H, Jones PG (2010) The Role of Social Support in Health Status and Depressive Symptoms After Acute Myocardial Infarction Evidence for a Stronger Relationship Among Women. Circ Cardiovasc Qual Outcomes 3: 143–150.
- Larsen KK, Christensen B, Sondergaard J, Vestergaard M (2013) Depressive Symptoms and Risk of New Cardiovascular Events or Death in Patients with Myocardial Infarction: A Population-Based Longitudinal Study Examining Health Behaviors and Health Care Interventions. PLoS One 8: e74393.
Citation: Bertelsen JB, Refsgaard J, Kanstrup H, Johnsen SP, Qvist I, et al. (2017) Self-reported Mental Health Status in Patients with Acute Coronary Syndrome: A Strong Predictor of Readmission, of Subsequent Anxiety and Depression and of Poor Risk Factor Modification? J Card Pulm Rehabil 1: 113.
Copyright: © 2017 Bertelsen JB, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Usage
- Total views: 4163
- [From(publication date): 0-2017 - Nov 21, 2024]
- Breakdown by view type
- HTML page views: 3446
- PDF downloads: 717