Case Report Open Access
Secondary Syphilis with Bone Involvement of the Skull: A Case Report
Herrera-Herrera I*, Escalona-Huerta C, Valle-Zapico JD, Montoya-Bordón J, Ordoñez-González C and Sobrino-Guijarro BDepartment of Radiology, University Hospital Fundación Jiménez Díaz, Madrid, Spain
- *Corresponding Author:
- Isabel Herrera-Herrera
Department of Radiology, University Hospital Fundación Jiménez Díaz
Madrid, Spain
Tel: +34-616318408
E-mail: isabel.herherrera@gmail.com
Received date: June 27, 2017; Accepted date: July 11, 2017; Published date: July 17, 2017
Citation: Herrera-Herrera I, Escalona-Huerta C, Valle-Zapico JD, Montoya-Bordón J, Ordoñez-González C, et al. (2017) Secondary Syphilis with Bone Involvement of the Skull: A Case Report. OMICS J Radiol 6:265. doi: 10.4172/2167-7964.1000265
Copyright: © 2017 Herrera-Herrera I, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Radiology
Abstract
A 40-year-old Human Immunodeficiency Virus (HIV) positive male consulted for headaches and a palpable lump on the scalp with laboratory findings relevant for increased acute phase reactants. Head CT and MR were performed, which showed temporal muscle and adjacent subcutaneous fat swelling, with underlying bone marrow edema and dural enhancement. A positive RPR test and further response to treatment for syphilis clinically confirmed secondary syphilis infection with bone and soft tissue involvement. Osseous involvement in secondary syphilis is relatively uncommon. It may be the first symptom of early-acquired syphilis and should be considered among the differential diagnoses for inflammatory lesions of the skull with overlying soft tissue swelling, especially in HIV positive patients.
Keywords
Syphilis; STD; HIV; Skull; Osteomyelitis; Periostitis
Introduction
Secondary syphilis corresponds to the hematogenous spread of Treponema pallidum and may present with pain secondary to osseous involvement. We report a case of a Human Immunodeficiency Virus (HIV) positive man with Computed Tomography (CT) and Magnetic Resonance (MR) imaging evidence of bone involvement of the skull and soft tissue swelling as initial presentation of early-acquired syphilis.
Case Report
A 40 year-old male with a history of HIV infection presented with a 1-month history of progressive pulsatile headache and neck pain. The patient also complained of a tender lump on the right scalp he had noticed recently. He recalled a minor head trauma 20 days earlier around the time the headaches had begun. He denied having fever, chills, joint pain or rash. The patient had been diagnosed with HIV infection 2 years earlier and was on a single tablet regimen, with good compliance and an undetectable viral load.
Physical examination revealed a 5 cm tender lump on the right temporoparietal region of the scalp with no cutaneous lesions. There was no significant cervical lymphadenopathy. Vital signs were normal, and neurological examination was unremarkable.
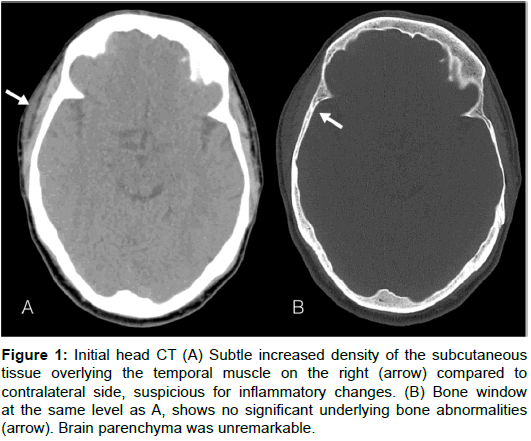
Laboratory tests were significant for increased erythrocyte sedimentation rate of 99 mm/h (normal <20 mm/h), and C-reactive protein of 22.4 mg/dl (normal <0.5 mg/dl). Non-contrast head CT showed subtle soft tissue swelling over the right temporoparietal region without underlying bone abnormalities (Figure 1).
Figure 1: Initial head CT (A) Subtle increased density of the subcutaneous tissue overlying the temporal muscle on the right (arrow) compared to contralateral side, suspicious for inflammatory changes. (B) Bone window at the same level as A, shows no significant underlying bone abnormalities (arrow). Brain parenchyma was unremarkable.
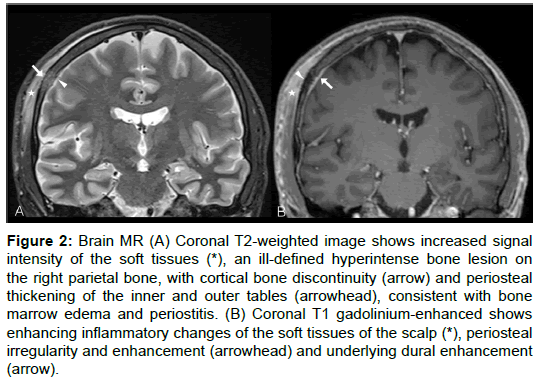
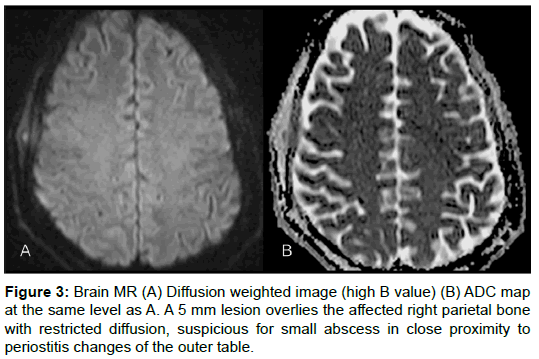
Five days later, MR imaging of the brain was performed using a 1.5T system, without and with gadolinium administration. An irregular area of increased T2-weighted signal intensity and enhancement of the soft tissues on the right temporoparietal scalp were identified. Underlying structures showed signs of bone marrow edema and periostitis of the parietal bone, as well as underlying dural enhancement (Figure 2). A 5 mm soft tissue lesion in contact with the external table and periosteal reaction showed restricted diffusion and was suggestive of a small abscess (Figure 3).
Figure 2: Brain MR (A) Coronal T2-weighted image shows increased signal intensity of the soft tissues (*), an ill-defined hyperintense bone lesion on the right parietal bone, with cortical bone discontinuity (arrow) and periosteal thickening of the inner and outer tables (arrowhead), consistent with bone marrow edema and periostitis. (B) Coronal T1 gadolinium-enhanced shows enhancing inflammatory changes of the soft tissues of the scalp (*), periosteal irregularity and enhancement (arrowhead) and underlying dural enhancement (arrow).
Further work up for infectious conditions revealed a positive quantitative Rapid Plasma Reagin (RPR) test with a titer of 1:64 and a positive Treponema pallidum Hemagglutination Assay (TPHA). The patient was treated initially with IM penicillin G 2400000 U, and completed further penicillin G scheme during the following weeks. There was gradual improvement of the symptoms and the palpable lump had disappeared completely in a 6-week follow up after treatment. A new RPR test decreased to a 1:8 titer confirming a clinical response to secondary syphilis.
Discussion
Syphilis is a chronic systemic venereal disease caused by the spirochete Treponema pallidum, a gram-negative corkscrew shaped bacterium. Syphilis infection has three well-characterized stages with multiple presentations. Primary syphilis is characterized by a chancre at the site of inoculation and regional lymphadenopathy. Untreated hematogenous spread represents the secondary stage, which characteristically presents with a maculopapular rash affecting the palms and soles 2-8 weeks after the chancre appears. About one-third of patients on the secondary stage progress to a tertiary latent form of which one-third develop neurosyphilis [1].
Significant complications are associated with untreated syphilis infection, as are facilitated HIV infection and transmission.
In 2000 and 2001, the national rate of reported primary and secondary syphilis cases in the United States of America was 2.1 per 100,000 populations, the lowest since 1941. However, primary and secondary syphilis infection rate has increased to 7.5 cases per 100,000 in 2015, with a recent increase of 66.7% compared to 2011 (4.5 cases per 100,000) [2].
Epidemiologic surveillance of venereal diseases in Spain reported an infection rate for primary and secondary syphilis of 7.68 cases per 100,000 in 2014. There has been an important rise in the rate of syphilis cases in Spain between 2008 and 2014, similar to afore mentioned trend in the USA [3].
Bones may be affected at all stages of syphilis, but is more characteristic of tertiary syphilis and congenital infection. These forms have become less frequent in the post penicillin era, however, and early stage syphilis infection of the bones can be seen on occasion.
Bone lesions in patients with secondary syphilis most often involve the skull and the long bones of the limbs, particularly the lower limbs. The most common skeletal lesion in early syphilis is periostitis, most frequently affecting the tibiae, followed by the skull, sternum and ribs. Osteolytic lesions are less frequent and most commonly affect the skull and sternoclavicular junction. Patients may present with both periostitis and osteolytic lesions. Involvement of the skull most commonly affects the frontal and/or parietal bones [1,4-12].
Skull involvement may show round osteolytic lesions on conventional radiography, with demineralization or sclerosis of the outer table and diploe, and less involvement of the inner table [7].
Radiographs and CT may show characteristic worm-eaten appearance of osteolytic lesions. However, both of them may fail to demonstrate signs of early periostitis or osteomyelitis as happened initially in our case. MR imaging and bone scintigraphy may show otherwise inconspicuous inflammatory signs of early bone involvement. MR imaging may show bone marrow signal abnormalities, with focal enhancement of the calvarial lesion and of the adjacent soft tissue inflammatory changes. Most prominent in our case was the periosteal enhancement with the development of a probable milimetric abscess. Underlying dural enhancement similar to our case has been previously described [6,7-12].
Positivity for a non-treponemal test like RPR should follow confirmation with a treponemal test, in our case TPHA. A subsequent drop in RPR titres following a proper antibiotic scheme clinically confirms syphilis infection. Identification of spyrochetes on biopsy material is variable, with reported organism identification by dark field microscopy in only 50% of biopsies in early stage syphilis infection with bone involvement [7]. Previous case reports with bone lesion biopsy or excision were negative for microorganism identification and/ or culture, with a clinical confirmation of syphilitic osteomyelitis after proper antibiotic treatment response [4-7,9,11,13].
Patients with secondary syphilis may present with pain in the general region of the affected bones with localized erythema, tumefaction and warmth, as well as headaches and generalized symptoms like asthenia and anorexia, all of which resolve progressively after adequate treatment [1,7,9].
Conclusion
Although an unusual presentation, skull involvement with soft tissue swelling and underlying meningeal enhancement should prompt ruling out secondary syphilis in the proper clinical setting. The recent increase in the rate of HIV and syphilis infections of the 21st century may also mean a significant rise in the number of early acquired syphilis osseous lesions seen in daily radiological practice.
References
- Akgoz A, Mukundan S, Lee TC (2012) Imaging of rikettsial, spirochetal, and parasitic infections. Neuroimag Clin N Am 22: 633-657.
- https://www.cdc.gov/std/stats15/std-surveillance-2015-print.pdf
- http://www.isciii.es/ISCIII/es/contenidos/fd-servicios-cientifico-tecnicos/fd-vigilancias-alertas/fd-enfermedades/pdf_2016/RENAVE_INFORME_ANUAL_2014.pdf
- Ollé-Goig JE, Barrio JL, Gurgui M, Mildvan D (1988) Bone invasion in secondary syphilis: Case reports. Sex Trans Infect 64:198-201.
- Rademacher SE, Radolf JD (1996) Prominent osseous and unusual dermatologic manifestations of early syphilis in two patients with discordant serological statuses for human immunodeficiency virus infection. Clin Infect Dis 23: 462-467.
- Gurland IA, Korn L, Edelman L, Wallach F (2001) An unusual manifestation of acquired syphilis. Clin Infec Dis 32: 667-669.
- Huang I, Leach JL, Fichtenbaum CJ, Narayan RK (2007) Osteomyelitis of the skull in early acquired syphilis: evaluation by MR Imaging and CT. Am J Neuroradiol 28: 307-308.
- Egan KM, Walters MC (2012) Osseous and meningeal involvement in secondary syphilis. Dermatol Online J 18: 1.
- Park KH, Lee MS, Hong IK, Sung JY, Choi SH, et al. (2014) Bone involvement in secondary syphilis: a case report and systematic review of the literature. Sex Trans Dis 41: 532-537.
- Naraghi AM, Salonen DC, Bloom JA, Becker EJ (2010) Magnetic Resonance Imaging features of early acquired syphilis. Skeletal Radiol 39: 305-309.
- Son C, Samples D, Brenner A, Floyd J (2015) Osteolytic calvarial lesions as initial presentation of latent neurosyphilis. J Clin Neurosci 22: 909-910.
- Kang SH, Park SW, Kwon KY, Hong WJ (2010) A solitary skull lesion of syphilitic osteomyelitis. J Korean Neurosurg Soc 48: 85-87.
- Bezalely S, Jacob G, Flusser G, Ablin J (2014) Syphilis: an unusual manifestation? BMJ Case Rep 2014: bcr2014204871.
Relevant Topics
- Abdominal Radiology
- AI in Radiology
- Breast Imaging
- Cardiovascular Radiology
- Chest Radiology
- Clinical Radiology
- CT Imaging
- Diagnostic Radiology
- Emergency Radiology
- Fluoroscopy Radiology
- General Radiology
- Genitourinary Radiology
- Interventional Radiology Techniques
- Mammography
- Minimal Invasive surgery
- Musculoskeletal Radiology
- Neuroradiology
- Neuroradiology Advances
- Oral and Maxillofacial Radiology
- Radiography
- Radiology Imaging
- Surgical Radiology
- Tele Radiology
- Therapeutic Radiology
Recommended Journals
Article Tools
Article Usage
- Total views: 6007
- [From(publication date):
August-2017 - Mar 30, 2025] - Breakdown by view type
- HTML page views : 5191
- PDF downloads : 816