Sclerosing Cholangitis with Ulcerative Colitis after Bariatric Surgery
Received: 23-May-2017 / Accepted Date: 22-Dec-2017 / Published Date: 29-Dec-2017 DOI: 10.4172/2161-069X.1000546
Abstract
Introduction: 48 years old Iraqi female presented in 2012 with 4 months upper abdominal pain with elevation of the liver enzymes and arthralgia, 1 year after sleeve gastrectomy for obesity with 25 kg weight loss. Labeled as auto immune hepatitis and was started on prednisolone 20 mg and azathioprine 100 mg, attended our center for second opinion. Her past history was impressive for gestational diabetes and ulcerative colitis diagnosed before 15 years and treated for 1 year with remission. Strong family history of diabetes including father, mother, brothers, and her uncle has ulcerative colitis.
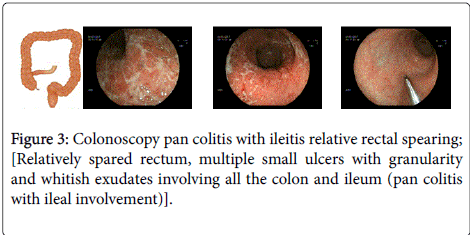
Investigations: Showed high liver enzymes, ALT 159, AST 286, ALP 455 and GGT 378, high eosinophil count. Imaging showed fatty liver with mild dilatation of the biliary system but CT scan, MRI, MRCP were not conclusive. ERCP showed features of sclerosing cholangitis with dominant stricture right hepatic duct, brushing and biopsy showed inflammatory changes. Colonoscopy showed pan colitis with ileal involvement, biopsy showed colitis with eosinophilic infiltration. She was treated with mesalazine, ursodiol, prednisolone and azathioprine. Regular follow over 4 years showed normal liver enzymes and last colonoscopy was reported as normal.
Conclusion: A patient developed elevated liver enzymes after sleeve gastrectomy for obesity. Imaging and endoscopies showed typical sclerosing cholangitis with dominant right hepatic bile duct stricture, colonoscopy showed pan colitis with high eosinophilic infiltration. The problem was the evaluation of the dominant stricture and the exclusion of malignancy.
Keywords: Gestational diabetes; Ulcerative colitis; Fatty liver; Cholangitis
Introduction
Inflammatory bowel disease is associated with extra-intestinal manifestations in a significant proportion of patients [1-3]. The interaction between inflammatory bowel disease (IBD) and hepatobiliary manifestations represents a classic example of liver-gut interaction. The presence of these hepatobiliary manifestations influences the outcome of associated IBD, in particular ulcerative colitis (UC) and vice versa.
Hepatobiliary manifestations constitute one of most common extra intestinal manifestations of IBD. Hepatobiliary manifestations are much more commonly associated with ulcerative colitis (UC) than Crohn’s disease (CD) [4,5]. The pathogenesis of hepatobiliary manifestations associated with UC may be related to liver gut interplay such as in primary sclerosing cholangitis (PSC), PSC/autoimmune hepatitis (AIH) overlap and IgG4 associated cholangitis (IAC).
Case Study
N.S. 48 year’s old Iraqi female worked in Iraq, Yemen and in Dubai UAE for 4 years, moved to Eastern Europe 2014. Presented to medical centres in Dubai 2012 with abdominal 18 months following bariatric sleeve gastrectomy with 25 kg weight loss, vague discomfort right upper quadrant with arthralgia, low back pains, normal bowel habits.
Review of her investigations from different countries before surgery showed raised liver enzymes before surgery.
Laboratory investigations:
• Bilirubin fasting blood sugar 111, AFP 4.3
• Bilirubin 0.7, ALT 159, AST 286, ALP 455, GGT 378.
• WBC 8500 eosinophils 18%.
• IgG 2100, ANA 1/160, Anti SM Positive 1/40 (N 1/10), p ANCA positive 1/80,
• Negative HBS Ag, HCV, AMA, LKM, ttG for celiac disease.
• Low ferritin 7, CA 19.9 normal, PT 13, INR 1, bile acids 11 N 10.
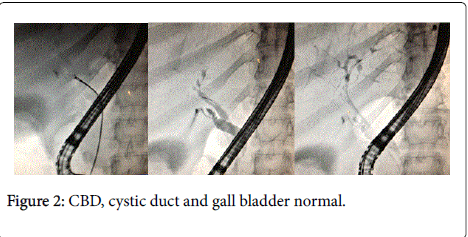
Imaging-Ultra sound fatty liver; dilated biliary system. MRI MRCP, CT scans all inconclusive (Figure 1). ERCP-sleeve gastorplasty/normal pylorus, normal papilla of Vater, bile in the duodenum, normal pancreatic duct, CBD looked normal, cystic duct and gall bladder normal (Figure 2). Tight irregular stenosis just above bifurcation, right sided duct did not fill properly, procedure-papillotomy done, the stenotic lesion was brushed with papillotome and bile was collected for cytology.
Biopsy forceps did not open properly at the stenotic area and good biopsies not obtained, the impression was klatskin tumor, the result of the bile smear cytology was negative for malignancy. Colonoscopy showed pan colitis with ileal involvement biopsy nonspecific colitis with excess eosinophils (Figures 3 and 4).
Colonic biopsy shows chronic destructive cryptal colitis with predominance of eosinophils (Colonic eosinophilia)+mild ileitis, no granuloma, no cellular dysplasia, no malignancy.
Diagnosis
Colitis with sclerosing cholangitis, dominant structure, Cholangio carcinoms
Management: Tests for parasites chlonorchis sinensis, opisthorchiscand and liver flukes were negative. Given short course for parasites albendazole bid for 3 days.
Labelled as autoimmune hepatitis based on low titre ANA positivity, positive anti smooth antibody positive, p ANCA positive. ERCP done showing features of sclerosing cholangitis with dominant stricture right hepatic duct, brushing and biopsy showed inflammatory changes.
Discussion
Primary sclerosing cholangitis on the back ground of chronic ulcerative colitis complicated by dominant stricture, the problem of the diagnosis of cholangio carcinoma is not easy in this patient brush cytology negative. The significance of eosinophil infiltrates pause another problem especially the problem of biliary parasites for that reason she was treated with albendazole [6-8]. Her quiescent colitis since 1996 colitis seemed active though with no symptoms. Her liver enzymes were elevated 5 years before surgery which may point to liver involvement since that time.
The differential diagnosis included: Eosinophilic gastroenteritis.
Parasites including: chlonorchis sinesis, opisthorchis, other parasites strongyloides, enterobius, trichuris trichiura (whipworm), fasciola hepatica, IGG 4 disease and drugs.
Final diagnosis
Sclerosing cholangitis with dominant right hepatic duct stricture associated with ulcerative colitis.
Comments
Patients with primary sclerosing cholangitis are at an increased risk of developing cholangiocarcinoma, which is difficult to diagnose because the biliary tree is already distorted,the diagnosis is difficult to make. Patients with IBD and a cholestatic pattern of liver biochemical test elevations should undergo imaging of the hepatobiliary system because of the relatively high pretest probability of PSC. This patient should have been tested 4 years back.
Ultrasonography or computed tomography (CT) may be useful for planning further diagnostic and therapeutic strategies in selected patients, but they are usually insufficient for a diagnosis of PSC because normal findings do not exclude the diagnosis. Ulcerative colitis has been reported in 25% to 90% of patients with PSC. The true prevalence of UC in PSC is probably closer to 90% when rectal and sigmoid biopsies are routinely obtained [8,9].
More than 7% of patients with ulcerative colitis may have PSC. Diagnosis of primary sclerosing cholangitis: a liver biopsy is not necessary for the diagnosis of PSC in patients with typical cholangiography findings [10]. A liver biopsy is recommended to diagnose small duct PSC if high-quality MRC (or ERC) is normal and in patients with disproportionally elevated aminotransferases to identify additional or alternative disease process.
References
- Lee YM, Kaplan MM (1995) Primary sclerosing cholangitis. N Engl J Med 332: 924-933.
- Fausa O, Schrumpf E, Elgjo K (1991) Relationship of inflammatory bowel disease and primary sclerosing cholangitis. Semin Liver Dis 11: 31-39.
- Angulo P, Lindor KD (1999) Primary sclerosing cholangitis. Hepatology 30: 325-332.
- Molodecky NA, Kareemi H, Parab R (2011) Incidence of primary sclerosing cholangitis: A systematic review and meta-analysis. Hepatology 53: 1590-1599.
- Bambha K, Kim WR, Talwalkar J (2003) Incidence, clinical spectrum, and outcomes of primary sclerosing cholangitis in a United States community. Gastroenterology 125: 1364-1369.
- Kaplan GG, Laupland KB, Butzner D (2007) The burden of large and small duct primary sclerosing cholangitis in adults and children: A population-based analysis. Am J Gastroenterol 102: 1042-1049.
- Lindkvist B, Benito de Valle M, Gullberg B, Björnsson E (2010) Incidence and prevalence of primary sclerosing cholangitis in a defined adult population in Sweden. Hepatology 52: 571-577.
- Bergquist A, Lindberg G, Saarinen S, Broomé U (2005) Increased prevalence of primary sclerosing cholangitis among first-degree relatives. J Hepatol 42: 252-256.
- Escorsell A, Parés A, Rodés J (1994) Epidemiology of primary sclerosing cholangitis in Spain: Spanish association for the study of the liver. J Hepatol 21: 787-791.
- Tung BY, Brentnall T, Kowdley KV (1996) Diagnosis and prevalence of ulcerative colitis in patients with sclerosing cholangitis (abstract). Hepatology 24: 169A.
Citation: Fayadh MH (2017) Sclerosing Cholangitis with Ulcerative Colitis after Bariatric Surgery. J Gastrointest Dig Syst 7: 546. DOI: 10.4172/2161-069X.1000546
Copyright: © 2017 Fayadh MH. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4174
- [From(publication date): 0-2017 - Apr 05, 2025]
- Breakdown by view type
- HTML page views: 3379
- PDF downloads: 795