School-Based Speech-Language Pathologists' Clinical Decision-Making Process in the State of California
Received: 23-May-2018 / Accepted Date: 18-Jun-2018 / Published Date: 25-Jul-2018 DOI: 10.4172/2472-5005.1000133
Abstract
Purpose: The purpose of this survey study was to examine the relationships between knowledge and training in evidence-based practice (EBP) and ethical decision-making processes among school based speech-language pathologists (SLPs) in the state of California, U.S.A. The possible factors that may prevent SLPs from making ethical clinical decision were also explored.
Method: An online survey collected demographic information as well as responses pertaining to school-based SLPs’ understanding and implementation of EBP and ASHA Code of Ethics, and perceptions of possible constraints to ethical decision-making.
Result: All demographic factors are not related to EBP implementation and ethical decision-making. Weak positive correlations were found between ethical decision-making and the use of research evidence as well as between EBP training and understanding the role of school-based SLPs. Factors that may have a notable impact on ethical decision-making include parent’s preference, school district policies, and lack of administrator’s support while caseload, workload, and service delivery model have relatively less impact.
Conclusion: School-based SLPs who had the EBP training more likely incorporated EBP components during their decision-making process. However, the lack of comprehensive understanding of EBP and explicit guidelines of applying EBP to clinical practice may limit the effective implementation of EBP.
Keywords: Ethics; Evidence-based practice (EBP); Clinical decisionmaking; School-based speech-language pathologists; EBP training; Survey
Introduction
Evidence-based practice
Evidence-based practice (EBP) is rooted in medicine, evidencebased medicine, and has been applied to related health care disciplines. It addresses the importance of incorporating external empirical evidence in the clinical decision-making processes. EBP is an important milestone in clinical practice and it has strongly advocated that clinical decisions have to be made based on research evidence rather than personal experience. David Sackett defined EBP as a “the conscientious, explicit and judicious use of current best evidence in making decisions about the care of the individual patient. It means integrating individual clinical expertise with the best available external clinical evidence from systematic research”. EBP emerged from medicine, became widely recognized in 1990s, and has been widely applied to different disciplines such as social work, psychology, and education. Optimal evidence-based practice is provided when practitioners integrate current best evidence, clinical expertise and patient values during decision-making process [1]. EBP promotes the inclusion of best available empirical research through carefully evaluating and integrating evidence to guide the clinical decisionmaking process. EBP is a process that consists of five essential steps, including 1) formatting a question, 2) retrieving the best available evidence, 3) evidence appraisal, 4) selecting intervention approaches based on research evidence, clinician expertise, and client values, 5) continuously monitoring data-based decisions [2]. Similar steps are also recommended by the American Speech-Language and Hearing Association (ASHA) as stated on the ASHA website (www.asha.org). Furthermore, Gillam et al. [3] adapted the six-step EBP approach discussed in the study of Porzsolt et al. [4] and then proposed a modified EBP decision-making process for child language intervention in schools. This revised process recommends a clinical decision should be generated by researching relevant evidence, critically evaluating research evidence, assessment student parent and clinician-agency factors, integrating all evidence to make a decision, and finally evaluating the outcome of the decision.
Even though most practitioners hold positive and supportive attitude toward the implementation of EBP in clinical practice, several challenges remain. First, the theory-practice gap has long been a challenge in clinical practice because of variations in contexts and implicit connection between research evidence and clinical cases [5]. Because of the complexity and heterogeneity of the clinical cases, it is difficult either implementing EBP on a broad scale or making a direct implication to a particular clinical case. Secondly, research data does not automatically translate to clinical evidence or practical information. Continuous and extensive education in interpreting research results and applying research findings to clinical practice is necessary. Clinicians need to be aware of the dynamic relationships among different contributing factors along with the intervention effectiveness and the possible limitations of applying research findings. Lastly, time constraint has been reported as one key factor that prevents clinicians from implementing evidence-based practice.
ASHA introduced the concept of EBP to the profession of speech, language, and hearing in 2004, and the EBP training has been gradually integrated into academic courses and strongly emphasized through ASHA Position Statement, practice policies, and the standards of clinical competence certification [6]. It has been explored that the speech-language pathologists’ (SLPs) attitude towards EBP, the use of EBP guidelines in clinical decision-making process, and perceived barriers in EBP. They discovered that the EBP trainings in graduate programs and clinical fellowships can predict clinicians’ attitude towards EBP. However, there is a discrepancy between positive attitude towards EBP and the implementation of EBP in clinical practice. When making clinical decisions, most SLPs still preferred the use of clinical experience and consulting colleagues than based on research evidence. In a more recent study conducted by Togher et al. [7], they surveyed academic faculty and clinical supervisors about integrating EBP into the SLP training programs, including academic curriculum and clinical practicum. Their findings revealed that despite the positive attitude of EBP, students had difficulty transferring EBP from academic work to clinical practice. Clinicians’ limited knowledge in research methods, the heterogeneity of clinical cases, and imbalance between external research evidence and client’s values may all affect the effectiveness of implementing evidence-based practice clinically.
Ethical principles and codes
Ethics is defined as a set of moral codes and standards practiced by a person or a group of people to determine the right course of action in a situation and appropriate behavior in a society [8]. It is a continuous decision-making process where different values and perspectives are evaluated through a logic and rational reasoning in order to obtain an optimal option [9]. Ethical guidelines are principle-based and above regulations and laws, because it aims the very best behavior rather than the acceptable behavior required by laws.
Among different types of ethics laid out by Horner [10], professional ethics, a protection of interests of patients served, and clinical ethics, an assurance of high quality of service, are more applicable to clinical practices. While most ethical issues and clinical cases involve a complex reasoning process that may not be simply resolved, ethical principles and codes can still provide guidance on making a more appropriate clinical decision. Beauchamp identified four principles that form the ground for bioethics and clinical practice, including 1) Beneficence: An action done for the benefit of others, 2) Non-maleficence: Avoidance of harming others intentionally, 3) Autonomy: Acknowledgement of a person’s right to make decision based on his/her own values and beliefs, and 4) Justice: An equal and fair access to resources and benefits [8,11]. These principles have guided practitioners and clinicians in different disciplines to consider the client’s priority and to address the client’s needs in the clinical decision-making process. In the past few decades, several studies in the field of speech-language pathology have emphasized and applied bioethics through mostly medical clinical cases, such as dysphagia [12,13], aphasia [14] and cognitive-communication disorders [15]. Additionally, these common ethical principles also have been applied to the management of children with autism spectrum disorders and to advocate for interdisciplinary work [16]. Ethical principles and codes provide an important framework for optimal clinical practice and promote the integrity of professional conduct. Cox [16] stated that purposes of ethical codes are ensuring professional competence and conduct, setting standards for optimal behaviors in clinical practice, and providing guidance on how to manage ethical dilemmas. Ethical codes are static; they should be reviewed and updated periodically to address the evolving and dynamic nature of clinical practice and new arising conflicts or challenges. The American Speech-Language Hearing Association (ASHA) Code of Ethics is the foundation of development of professionalism and clinical competence and also provides guidelines for research development and public and professional relationships [17]. The ASHA Code of Ethics was first published in 1952 and it has been revised regularly to reflect the dynamic changes in health care, education laws and regulations, and the evolving ethical issues. Chaborn et al. [11] made direct and clear connections among The ASHA Code of Ethics, bioethics, and professionalism in their article and stated that both professionalism and ethical practice require clinicians to continue the growth in knowledge and skills in these areas for maximizing the quality of service for clients being served. In addition, professional competence is viewed as a moral obligation, and both ethical practice and professional competence are rooted in evidence-based practice [11].
Evidence-based ethics in clinical practice
The relationship between ethics and evidence-based practice may not seem to be directly indicated. In fact, ethics and EBP is strongly connected and the relationship cannot be easily disentangled. One of the essential elements of EBP implementation involves moral judgment, which different values have to be weighed and considered before making clinical decisions. Nicholls et al. [2] stressed that all clinical decisions are “value-laden”; different values should be explicitly expressed in clinical practices. Evidence-based clinical decisions involve the tradeoffs between benefits and harms; therefore, clinicians must explore these contested values till the best possible decision may be achieved. Christiansen et al. [18] argued that “the primary EBP is a moral one”; both ethics and EBP emphasize professional credibility and the achievement of the most effective intervention outcome for those being served. They further asserted that it is a professional and moral obligation to make a clinical decision based on ethical principles and implementing evidence based practice. Borry et al. [19] proposed the term “evidence-based ethics” to emphasize the importance of EBP in the ethical clinical decision-making process because “greater knowledge leads to better decision making” [19], p307.
In the same vein, Strech [20] proposed a clinical decision-making framework with evidence-based ethics. He proposed that the use of empirical evidence should be guided by ethical principles (i.e. beneficence, non-maleficence, justice, and autonomy) and based on both quality and relevance of the personal experience and external research evidence. In order to draw an evidence-based and ethical clinical decision, patient’s preference, benefits, harms, and access to resources must be weighed against each other along with empirical information [20], p6. Similarity, Tannahill [21] proposed a decisionmaking triangle that incorporates ethical principles, evidence, and theory in the realm of public health. He claimed that evidence is used to make a judgment that ethical principles must be critically evaluated while theories are taken into consideration to close the gap in the current available evidence.
In the application of evidence-based ethics in clinical practice, Chaborn et al. [11] claimed that ethics provides an important context for EBP because acting for the other’s benefit is essential in both professionalism and ethics. Additionally, both ethical practice and EBP require clinicians to provide the “best possible service” [11]. In order to provide the optimal services, SLPs must constantly develop and advance their clinical skills, maximize benefits, and minimize harm while considering the client’s beliefs, values, and priority. Therefore, ethical practice not only shares a common ground with EBP in clinical decision-making process and practice but also serves as a primary instrument of implementing EBP to ensure that the clinician acts for the good of the client. Principal of The ASHA Code of Ethics also clearly states that clinicians shall use evidence based judgment and every resource to ensure the quality of service [17]. Christiansen et al. [18] emphasized that when evidence is not taken into consideration, the clinical decision is not ethical nor professional. Hence, while implementing evidence-based practices, clinicians ought to apply the principles of bioethics to achieve the most beneficial outcomes for clients being served. The author added that every clinical ethical concern should be carefully evaluated based on medical indications (e.g., medical history, treatment options, accurate diagnosis), client’s preferences and quality of life, and other contextual features (e.g., economic, legal issues, family preferences) [22]. The client’s values, preferences, and interests should always be taken into consideration along with current best available research evidence to promote the client’s autonomy because it is the core value of evidence-based and ethical practice. Lopez et al. [23] conducted a survey study on the occupational therapist’s perceptions on the four factors, including economics, ethics, independent professional judgment, and EBP, during intervention planning process. Their results showed that economic constrains (i.e. reimbursement policies) impeded the implementation of the most effective care plans. Furthermore, practitioners should be aware of the interrelationship among economics, ethics, independent professional judgment, and EBP and how economic factor may affect professional judgment and making ethical decisions. Several challenges that prevent the implementation of EBP were also discussed, such as lack of research evidence, lack of access to research, insufficient training, and insufficient research databank. Moreover, Jette et al. [24] found that lack of time was one of the major barriers for physical therapists to implement EBP followed by inability to apply research to clinical practice.
According to ASHA National Office’s 2001-2006 Trends of Ethics Inquiries, there were approximately 3000 ethical inquires every year. Kenny et al. used a narrative approach to investigate the relationship between how SLPs reacted to ethical dilemmas and the years of experience [22,25]. They found experienced SLPs were more likely to facilitate their ethical reasoning processes using an integrated approach, including case studies, ethical principles, prior experiences, and incorporated insights from different professionals. They also suggested that ethical practices should be reinforced on a regular basis because a clinician’s ethical reasoning ability may not develop concurrently with clinical skills. When clinicians encounter ethical dilemmas, they recommended SLPs use ASHA Code of Ethics, bioethical principles, and ethical decision-making models as guidance.
Factors that prevent the implementation of evidence-based and ethical clinical practice in schools
The Individuals with Disabilities Education Act and No Child Left Behind emphasized the use of “scientifically-based research” as the foundation for education programs and interventions. Section 8101(21) (A) of the Elementary and Secondary Education Act (ESEA) also defines an evidence-based intervention as being supported by strong evidence, moderate evidence, promising evidence, or evidence that demonstrates a rationale and encourages the stakeholders (e.g., state educational agencies, local educational agencies, and educators) to critically consider all relevant evidence during the decision-making process. Every Student Succeeds Act (ESSA) signed by President Obama in 2015 continues to require the state and local educational agencies to provide “evidence-based interventions” to improve student’s academic performance and achieve the desirable outcomes. In the year of 2016, the Department of Education released a new guidance on “using evidence to strengthen education investments” to support evidenced-based instruction and intervention for better outcomes of students through five steps: identification of local needs, selection of relevant and evidence-based intervention, planning for implementation, intervention implementation, and evaluation of the effectiveness of intervention. ASHA also published “Roles and responsibilities of speech-language pathologists in schools” in 2010 and highlighted the necessity of incorporating EBP during the prevention, assessment, and intervention process. Given that EBP has been emphasized by both Department of Education and ASHA, school-based SLPs are obligated to incorporate professional competence, research evidence, and client’s values during the clinical decision-making process.
Even though a clear connection between EBP and IDEA regulations was clearly highlighted, several challenges remained to prevent schoolbased SLPs to implement EBP, such as time constraints, lack of research evidence, insufficient training in and exposure to research designs, and other external factors Whitmire et al. [26], Hoffman examined the relationships among school based SLPs’ training in EBP, resources available in workplaces, and EBP implementation. The findings revealed that even though majority of school-based SLPs expressed the interests in continuous training in EBP, the implementation of EBP in schools is still a working progress. State and local educational agencies should work with SLPs to provide more support and reduce barriers of EBP implementation in order to facilitate evidence-based practice in school settings. They also stated that formal EBP training did not explain the difference in clinical service delivery, and the SLP’s ability to apply research evidence to clinical practice should be strengthened.
While a single factor cannot explain the difficulty of implementation of EBP and best practice in school, Brandel proposed a school-based intervention decision making model that examined how students, SLPs, and workplaces influence clinical service delivery. Their survey results indicated that SLPs’ recommendations were based on the student’s individual needs which aligned with ASHA and IDEA policies. However, caseload size and work places had an influence on the recommended service delivery model, especially in preschool settings with the most severe disabilities. Hutchins also surveyed a group of school-based SLPs to investigate the relationships among caseload, workload, job satisfaction, and best practice in the state of Vermont. Their findings showed a negative correlation between lack of time and providing best practice. A higher caseload and workload may contribute to less time to deliver optimal services, which leads to lower job satisfaction and SLP retention rate. Moreover, the method of service delivery, such as group treatment, may be more associated with workload than the students’ needs.
According to 2016 ASHA annual School Survey, 43% of schoolbased SLPs identified compromising quality of services as an ethical challenge even though the percentage of agreement decreased as the SLP’s years of experience increased. Nearly 50% of school-based SLPs reported that optimal service may not be delivered due to several reasons. The major concerns consistently reported by school-based SLPs from 2000 to 2016 included excessive paperwork, high caseloads, high workloads, and limited time to implement optimal service delivery models. These concerns all have a negative impact on the implementation of evidence based practice and SLPs’ ability to provide the best possible service to their students.
Purposes of current study
Most research to date examining the relationship between ethical issues and clinical decision-making focused on either a specific disorder, such as dysphagia, or a particular setting, such as private practice [27]. These studies examining ethical issues in the field of speech-language pathology mainly focused on medical settings and private practice [15,13]. Among these studies, dysphagia received more attention than other communication disorders [12]. According to ASHA [28], about 53% of the SLPs work in schools. However, no research to date examined the relationship between EBP and ethical practice in the school-based SLPs. Although Hoffman examined the implementation of EBP in school-based SLPs in a national large-scale survey study, their study did not investigate the use of EBP in decisionmaking process nor possible factors, such as caseload, that may prevent SLPs from providing the best possible service to their clients/students. Majority of the literature that investigates the relationship between ethical issues and clinical decision-making is categorized as Level IV Evidence that contained the opinion of authorities and/or reports of expert committees through the discussion of clinical cases (ASHA, n.d.). Since California is one of the states that school-based SLPs may have large caseloads and subsequently high workloads, examining the factors that may impact the ethical decision-making process may provide valuable insight to the field of speech-language pathology. To date, there has been limited research investigating the relationship between SLP’s training in EBP and application of ethical principles during clinical decision-making process in schools. Therefore, this current study aimed to discover not only the relationships between the knowledge of EBP and the implementation of EBP, but also California school-based SLPs’ perception on factors related to unethical clinical decisions. The study was designed to answer the following questions.
1. What is California school-based SLPs’ understanding of evidence-based practice and ASHA Code of Ethics?
2. What are California school-based SLPs’ self-perceptions on the implementation of evidence-based practice?
3. What are California school-based SLPs’ perceptions on factors that may prevent them from making ethical clinical decisions when qualifying a student for speech and language services?
Methods
Procedure
According to the report from US Bureau of Labor Statistics in May 2016, approximately 11430 speech-language pathologists work in various settings in the state of California. With the estimated 53% SLPs who work in school setting on ASHA 2016 school-survey, it was estimated that 6,000 school-based SLPs would be potential participants in the study. The inclusion criteria of this survey study were SLPs who 1) hold both a valid Certificate of Clinical Competence in Speech- Language Pathology (CCC-SLP) and California State License in Speech-Language Pathology and 2) have experience working in K-12 schools in the state of California. The participants were limited to SLPs who worked in K-12 schools because the current study only examined the perceptions and responses from SLPs who provide clinical service to clients/students in school settings. A list of email addresses publicly available on California school district websites were complied. The online survey invitation was sent to either the speech-language pathology programs or special education programs in the school districts and the program coordinators were encouraged to disseminate the invitation to qualified SLPs. Additionally, the survey invitation was also sent to the directors of ten (10) California Speech- Language Hearing Association (CSHA) Districts. Word-of-mouth communication was also encouraged in order to facilitate the participant recruitment. The IRB approval was granted by California State University, Long Beach Instructional Review Board on April 4, 2017 and the online survey was available for approximately three months, from April 11, 2017 to June 30, 2017.
Participants
The SLPs who provided the consent and satisfied the recruitment criteria were invited to participate the survey study at any time and any location during the data collection period. The survey return rate could not be calculated because the data regarding online survey access could not be estimated. The survey was anonymous, and each participant was only allowed to take the survey only once through web browser/device restrictions. One hundred and sixty-four (=164) responses were collected with one respondent did not agree to participate in the study. Among the 163 participants, 19 participants did not meet the recruitment criteria, such as not holding both CCCSLP and CA state license or not having experience working in schools. These participants (=19) who did not meet the recruitment qualifications were directed to the last page of the survey to discontinue the survey. This resulted in a final sample size of 144, which represent approximately 2% of California school-based SLPs. All qualified precipitants were taken to the background information section to begin the survey. The mean years of holding CCC-SLP was 12.36 years (=10.51), with a range of 0-37 years. The mean years of working in public schools was 11.75 years (=9.52), with a range of 1-37 years. Because the participant had the option of skipping any question he or she was not willing to respond till the end of the survey, the number of responses to each question ranged from 133 at the beginning of the survey to 116 at the end of the survey. Table 1 summarizes demographic data for the participants in this study. Most participants (=52) aged between 30 to 39 years (39.11%), 18 participants aged between 20-29 years 15 (13.5%), 28 participants aged between 40-49 years (21.1%), 23 participants aged between 50-59 years (17.3%), and 12 participants aged between 60-69 years (9.0%). None reported older than 70-years-old. Ninety (=90) participants have a bachelor’s degree in Communication Disorders and Science or Speech- Language Pathology along with their Master’s degree (67.7%) while 43 participants (32.3%) have a bachelor’s degree in other majors, such as linguistics or psychology. Most participants (=115, 86.5%) reported working in K-5 schools, 37 participants (27.8%) reported working in middle schools, and 43 participants (32.2%) reported working in high schools. Please note that participants were allowed to select more than one response for this question, and 62 participants (46%) reported that they worked in more than one type of settings.
| Public School SLPs | ||
|---|---|---|
| Variable | Frequency | Percentage |
| Age (n=133) | ||
| 20-29 | 18 | 13.5% |
| 30-39 | 52 | 39.1% |
| 40-49 | 28 | 21.1% |
| 50-59 | 23 | 17.3% |
| 60-69 | 12 | 9.0% |
| 70-79 | 0 | 0.0% |
| Bachelor’s degree in CSD/SLP (n=133) | ||
| Yes | 90 | 67.6% |
| No | 43 | 32.3% |
| School settings (multi-select) (n=133) | ||
| K-5 | 115 | 86.5% |
| Middle School | 37 | 27.8% |
| High School | 43 | 32.3% |
| Average monthly caseload (n=133) | ||
| Less than 50 students | 38 | 28.6% |
| 50-59 | 55 | 41.4% |
| 60-69 | 26 | 19.5% |
| 70-79 | 9 | 6.8% |
| 80-89 | 2 | 1.5% |
| More than 90 students | 3 | 2.3% |
Table 1: The summary of participants’ background information.
The largest number of participants (n=55, 41.4%) reported their average monthly caseload was between 50-59 students, 38 participants (28.6%) had less than 50 students on their caseload, 26 participants (19.5%) had monthly average 60-69 students on their caseload, 9 participants (6.8%) had monthly average 70-79 students on their caseload, 2 participants (1.5%) had monthly average 80-89 students on their caseload, and only 3 participants (2.3%) reported their average their average monthly caseload was more than 90 students.
Measurement
This survey study aimed to explore whether the EBP and ethical principles were implemented during the clinical decision-making process. Additionally, the survey also intended to discover factors that may prevent school-based SLPs from making ethical clinical decisions, such as qualifying a student for speech and language services. The survey was web-based and developed and delivered through survey engine Survey Monkey® (www.surveymonkey.com). Once the participant provided the consent and met the inclusion criteria, the participant continued to the section for collecting background information. The background information section consisted of 7 questions: 1) three multiple-choice questions regarding the SLP’s age, monthly caseload, average evaluation time, 2) two open-ended questions which required the participant to fill in the number of years of holding CCC-SLP and years of working in K-12 schools, 3) one open-ended question about the participant’s undergraduate major, and 4) one multiple-choice questions asking the participant’s work settings (i.e. K-5, middle school, high school) where they have been working in the past 5 years. The participant was allowed to skip questions, which resulted in 133 our 144 participants (92.4%) completed all 7 questions in the background information section. The rest of the survey contained five independent sections. This study only focuses on analyzing two sections, including EBP knowledge/implementation and factors related to unethical clinical decisions. The EBP section contained 14 questions pertaining to school-based.
SLP’s understanding and experience with EBP and ASHA Code of Ethics using a 5-point Likert scale (i.e. strongly disagree to strongly agree). The other section included 15 possible factors that may prevent school-based SLPs from making an ethical clinical decision based on a 5-point Likert scale (i.e. not related at all to strongly related). The participant had the option of skipping any questions he or she was not willing to answer. Please see Appendix 1 for the consent page and Appendix 2 for the complete list of survey questions.
Results
The survey probed California school-based SLPs to indicate within a range of strongly disagreed to strongly agreed or not related at all to strongly related with statements regarding their EBP knowledge and implementation and their perceptions on factors related to unethical clinical decisions. The survey data were analyzed using descriptive and nonparametric analyses via SPSS Version 24.0. A Spearman’s rankorder correlational analysis was used to evaluate the relationship between the factors related to EBP implementation and ethical clinical decision making process.
EBP knowledge and training
Participants were asked to report if they know what EBP is and if they had EBP class/training either in their graduate programs or via CEU courses. Majority of the respondents (n=124, 96.1%) indicated that they either strongly agreed (n=115, 89.1%) or somewhat agreed (n=9, 7.0%) that they have heard about evidence-based practice. Only three respondents (n=3, 2.32%) indicated that they have never heard about EBP. Additionally, majority of the respondents (n=115, 89.1%) indicated that they strongly agreed (n=65, 50.4%) or somewhat agree (n=50, 38.7%) that they know EBP well enough to explain it to other professionals. Ten respondents (n=10, 7.7%) were neutral, two (n=2, 1.6%) disagreed and two (n= 2, 1.6%) strongly disagreed that they can explain EBP to other professional. Table 2 outlines a summary of the descriptive data described.
| Variable | Strongly | Somewhat | Neural | Somewhat | Strongly |
|---|---|---|---|---|---|
| disagree | disagree | agree | agree | ||
| Have heard about | n=3 | n=0 | n=2 | n=9 | n=115 |
| EBP (n=129) | 2.3% | 0% | 1.6% | 7.0% | 89.1% |
| Know EBP well | n=2 | n=2 | n=10 | n=50 | n=65 |
| to explain to | 1.6% | 1.6% | 7.7% | 38.7% | 50.4% |
| others (n=129) |
Table 2: Self-Reports on EBP Knowledge.
Regarding to EBP training, majority of the respondents (n=83, 64.9 %) indicated that they either strongly agreed (n=59, 46.1%) or somewhat agreed (n=24, 18.8%) that they had training in EBP during their master’s program. Only eleven respondents (n=11, 8.6%) somewhat disagree and twenty respondents (n=20, 15.6%) strongly disagree that they had EBP training when they were in graduate programs. Similarly, majority of the respondents (n=90, 70.3 %) indicated that they either strongly agreed (n=52, 40.6%) or somewhat agreed (n=38, 29.7%) that they had attended a continuing education unit (CEU) course focusing on EBP. Only eleven respondents (n=7, 5.5%) somewhat disagree and twenty respondents (n=13, 10.2%) strongly disagree that they had had attended a CEU course focusing on EBP. Table 3 shows the descriptive data of self-report on EBP training.
| Variable | Strongly | Somewhat | Neural | Somewhat | Strongly |
|---|---|---|---|---|---|
| disagree | disagree | agree | agree | ||
| EBP Training in | n=20 | n=11 | n=14 | n=24 | n=59 |
| graduate program | 15.6% | 8.6% | 10.9% | 18.8% | 46.1% |
| (n=128) | |||||
| Take EBP CEU | n=13 | n=7 | n=18 | n=38 | n=52 |
| courses (n=128) | 10.2% | 5.5% | 14.0% | 29.7% | 40.6% |
Table 3: Self-Reports on EBP Training.
Knowledge of ASHA policies and statements
The participants were asked to report if they are familiar with ASHA Code of Ethics and Position Statements. Majority of the respondents (n=122, 95.3%) indicated that they either strongly agreed (n=84, 65.6%) or somewhat agreed (n=38, 29.7%) that they are familiar with the ASHA Code of Ethics. Additionally, 116 SLPs (90.6%) reported that they have read the position statement published by ASHA about roles and responsibilities of speech-language pathologists in schools. One hundred and twenty-five SLPs (n=125, 97.6%) indicated that they know their roles and responsibilities as a school-based SLP. Table 4 is the summary table of the participants’ responses on knowledge of ASHA statements.
| Variable | Strongly | Somewhat | Neural | Somewhat | Strongly |
|---|---|---|---|---|---|
| disagree | disagree | agree | agree | ||
| ASHA Code of | n=0 | n=1 | n=5 | n=38 | n=84 |
| Ethics (n=128) | 0% | 0.8% | 3.9% | 29.7% | 65.6% |
| ASHA Position | n=2 | n=2 | N=8 | n=29 | n=87 |
| Statements | 1.6% | 1.6% | 6.2% | 22.7% | 67.9% |
| (n=128) | |||||
| Role as school- | n=0 | n=1 | n=2 | n=24 | N=101 |
| based SLPs | 0% | 0.8% | 1.6% | 18.7% | 78.9% |
| (n=128) |
Table 4: The responses on familiarity with ASHA Code of Ethics and Position Statement.
EBP guideline implementation
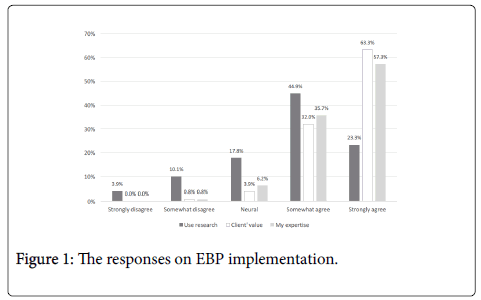
The participants were asked to report whether they implement the EBP guidelines. Figure 1 illustrates the responses about the implementation of current research evidence, the client’s values, and self-expertise into clinical decision making. More school-based SLPs (n=81, 63.3%) strongly agreed that they always consider the client’s values, which is higher than referring to current research for assessment plans frequently (n=30, 23.3%) and confidence in their own expertise (n=74, 57.3%). Sixty-three participants (n=63, 49.6%) strongly agreed that EBP is an important part in their clinical decisionmaking process, and fifty-one respondents (n=51, 39.8%) strongly agreed that they make their clinical decisions based on EBP guidelines. Similarly, sixty three SLPs (n=63, 49.6%) indicated they strongly agree that they use EBP guidelines to set annual goals for their students. Table 5 is the summary table of the participants’ responses on EBP implementation.
| Variable | Strongly | Somewhat | Neural | Somewhat | Strongly |
|---|---|---|---|---|---|
| disagree | disagree | agree | agree | ||
| Use EBP for | n=0 | n=5 | n=15 | n=44 | n=63 |
| annual goals | 0% | 3.9% | 11.8% | 34.7% | 49.6% |
| (n=127) | |||||
| EBP is part of | n=0 | n=2 | n=14 | n=48 | n=63 |
| decision-making | 0% | 1.6% | 11.0% | 37.8% | 49.6% |
| process (n=127) | |||||
| Make decisions | n=0 | n=2 | n=11 | n=64 | n=51 |
| based on EBP | 0% | 1.6% | 8.6% | 50% | 39.8% |
| guidelines | |||||
| (n=128) |
Table 5: The responses about making clinical decisions based on EBP guidelines.
Factors related to ethical decisions
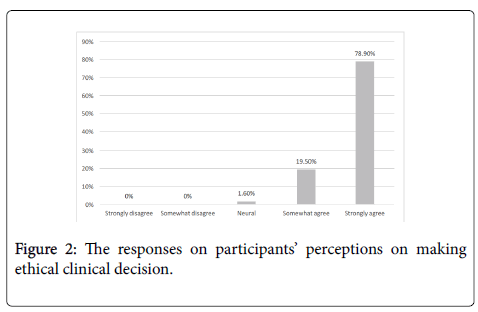
School-based SLPs were asked to report whether they believe they have been making ethical clinical decisions. Almost all the respondents (n=126, 98.4%) indicated that they either strongly agreed (n=101, 78.9%) or somewhat agreed (n=25, 19.5%) that their clinical decisions are ethical. Figure 2 shows the self-perception on making ethical clinical decisions.
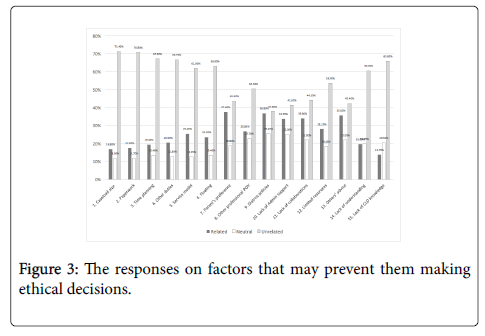
Respondents were asked to identify factors that may prevent them from making ethical decisions. The top five mostly identified factors that may prevent them from making ethical decisions were parent’s preference (n=44, 37.6%), school district’s policies (n=42, 36.8%), lack of support from administration (n=39, 33.7%), lack of collaborations with other IEP team members (n=40, 33.9%), and advice from more experienced colleagues (n=42, 35.6%). The top five mostly identified factors that the respondents do not consider preventing them from making ethical decisions are caseload size (n=85, 71.4%), paperwork and documentation (n=85, 70.8%), time planning (n=80, 67.2%), other duties (e.g., providing in service) n=78, 66.7%), and lack of knowledge of diverse linguistic and cultural backgrounds 20 (n=77, 65.8%). Figure 3 illustrates the responses for factors that may prevent them making an ethical decision.
Nonparametric analyses
A Spearman’s rank-order correlational analysis was run to evaluate the relationship between the EBP principle implementation and ethical clinical decision-making process. Many statistically significant correlations were revealed. There was a strong positive correlation between using EBP guidelines to set annual goals and incorporating EBP in clinical decision making process, which was statically significant, rs(126)=.78, p<.001. Another strong positive correlation, rs(125)=.68, p<.001, was between using EBP guidelines to set annual goals for students and making clinical decisions based on EBP guidelines. Unsurprisingly, the relationship between incorporating EBP as part of clinical decision-making process and making clinical decisions based on EBP guidelines is also a strong positive correlation, rs (124)=.67, p<.001. The relationship between making an ethical clinical decision and making decisions based on EBP guidelines is a statistically significant moderate positive correlation, rs (126)= .39, p<. 01.
No correlation was found between the number of years working in the school system and using EBP guidelines in clinical decision making; no correlation was found between the number of years working in the school system and making ethical clinical decisions. Additionally, no correlation was found between caseload and using EBP guidelines in clinical decision making and between caseload and making ethical clinical decisions. A moderate positive correlation was found between using EBP guidelines in decision-making and making ethical clinical decisions (r (126)=.31, p<.01). Tables 6 and 7 summarized the correlation coefficients of the variables related to EBP implementation and making ethical clinical decisions.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | ||
| .19* | ||||||||||||||||
| 1. | Heard of | 1.00 | .40** | .20* | .30** | .09 | .15 | .03 | .11 | .21** | .11 | .30** | -.03 | -.03 | ||
| EBP | ||||||||||||||||
| 2. | Know EBP | 1.00 | .43** | .48** | .25** | .22** | .14 | .42** | .51** | .24** | .21** | .09 | .16* | .42** | ||
| well | ||||||||||||||||
| 3. | EBP | 1.00 | .09 | .21* | .20* | -.13 | .25** | .24** | .24** | .25** | .03 | .16* | .30** | |||
| Training | ||||||||||||||||
| 4. | EBP CEU | 1.00 | .28** | .05 | .27** | .41** | .36** | .07 | .11 | .06 | .03 | .30** | ||||
| courses | ||||||||||||||||
| 5. | Use research | 1.00 | .19* | .22** | .50** | .48** | .21* | .32** | .22** | .14 | .48** | |||||
| 6. | Client’s | 1.00 | .30** | .24** | .24** | .30** | .27** | .35** | .23** | .30** | ||||||
| value | ||||||||||||||||
| 7. | My expertise | 1.00 | .37** | .26** | .19* | .18* | .30** | .22** | .36** | |||||||
| 8. | Use EBP for | 1.00 | .78** | .37** | .25** | .31** | .29** | .68** | ||||||||
| goals | ||||||||||||||||
| 9. | Clinical | 1.00 | .35** | .22** | .32** | .31** | .67** | |||||||||
| decisions | ||||||||||||||||
| 10. Code of | 1.00 | .58** | .36** | .35** | .30** | |||||||||||
| ethics | ||||||||||||||||
| 11. Position | 1.00 | .43** | .32** | .24** | ||||||||||||
| Statement | ||||||||||||||||
| 12. Role as | 1.00 | .46** | .34** | |||||||||||||
| school SLP | ||||||||||||||||
| 13. Ethical | 1.00 | .39** | ||||||||||||||
| decisions | ||||||||||||||||
| 14. EBP | 1.00 | |||||||||||||||
| Decisions | ||||||||||||||||
*p< .05, **p<.01.
Table 6: The correlation matrix for EBP knowledge and EBP implementation.
| 1 | 2 | 3 | 4 | 5 | 6 | |
| 1. Age | 1.0 | .74** | .71** | .04 | -.17 | -.13 |
| 2. Year CCC | 1.0 | .91** | .12 | -.14 | -.11 | |
| 3. Year in School | 1.0 | .20* | -.13 | -.16 | ||
| 4. Caseload | 1.0 | -.06 | -.14 | |||
| 5. Using EBP in decision making | 1.0 | .31** | ||||
| 6. All clinical decisions are ethical | 1.0 |
*p< .05, **p<.01.
Table 7: The correlation matrix for EBP implementation and making ethical decisions.
Discussion
Optimal clinical decision-making processes require the implementation of evidence based practice and ethical/moral judgment [11] In order to provide the most appropriate services, SLPs must make decisions that maximize benefits and minimize harm while considering the client’s beliefs, values, and priority. Since clinicians have the moral and professional obligation to ensure the best practice is delivered, incorporating ethical principles into evidence-based practice during clinical decision-making processes ensures that the clinician acts for the good of the client. As indicated by Strech [20], the use of empirical evidence should be guided by ethical principles and based on both quality and relevance of the personal experience and external research evidence. The purposes of this survey study were to explore california school-based SLPs’ knowledge of evidence-based practice and The ASHA Code of Ethics, their perceptions on the implementation of EBP guidelines and ethical principles during their clinical decision-making processes, and factors that may prevent them from make ethical decisions clinically.
Table 6 summarized the correlation coefficients of the variables related to EBP knowledge and implementation.
California school-based SLPs’ understanding of evidencebased practice and The ASHA Code of Ethics (Question 1)
Almost all the participants (96.1%) reported that they know what EBP is and majority of them (64.9%) have training on EBP in graduate programs and 70% of the participants stated that they had attended a continuing education unit course focusing on EBP. Additionally, 95.3% of the participants stated that they are familiar with The ASHA Code of Ethics. The survey results indicate that most California school-based SLPs who participated in this survey study eported positively on understanding not only The ASHA Code of Ethics but also ASHA’s Position Statement and their roles as school-based SLPs. This positive outcome may result from the long-term effects of ASHA’s advocacy and governance, a comprehensive curriculum and emphasis on these guidelines through academic training programs, and the requirement of continuing education learning throughout SLPs’ professional career. Nevertheless, although most of the school-based SLPs considered they understand EBP and their clinical decisions are ethical, surprisingly, a weak correlation was found between ethical clinical decision-making and the use of research evidence. These clinicians may not view the overarching goal of EBP as an ethical one or they do not associate ethical principles with EBP implementation. These participants seem to understand evidence-based practice and their roles as school-based SLPs, but view ethical principles as separate entities instead of an integrated clinical delivery system of providing the best possible speech and language services.
The lack of comprehensive understanding of evidence-based practice and ASHA Code of Ethics may also contribute to the potential difficulties in incorporating research evidence in the clinical practice. This may also explain why majority of the participants reported that they know evidence-based practice but do not feel confident to explain it to other professionals.
California school-based SLPs’ self-perception on the implementation of evidence-based practice (Question 2)
Majority of the participants (87.4%) reported that EBP was an important part of their decision-making processes, and many of them (89.8%) also indicated that they made their clinical decisions based on EBP guidelines. Additionally, large number of these school-based SLPs (84.3%) stated that they followed EBP guidelines to set annual goals for their students.
Optimal and evidence-based services are provided when clinicians integrate current best evidence, clinical expertise and patient values during decision-making processes [1]. Regarding EBP implementation, more California school-based SLPs participated in this study (63.3%) considered the client’s values more than applying current research evidence (23.3%) or their own expertise (49.6%). In other words, more school-based SLPs incorporated client’s values during their decisionmaking process than integrated research evidence or used their clinical expertise. Although most participants reported that they make decisions and set annual goals based on EBP guidelines, notably fewer of them use research evidence to support their decision-making process when the EBP components were broken down. A plausible reason to explain this discrepancy may be SLPs know the components of evidence-based practice, but have difficulty in implementing all EBP components or have limited understanding of the ultimate goal of EBP. Our findings supported Kenney’s results, that exposure to research and EBP increased the attitude toward EBP but there was still a discrepancy between positive attitude toward EBP and the self-reported implementation of EBP in clinical practice. Togher et al. [7] also suggested the clinicians had difficulty transferring EBP from academic training to clinical decision-making process. Therefore, the lack of comprehensive understanding of EBP and explicit guidelines about how to implement EBP clinically may contribute to the difficulty in implementing EBP in the clinical decision-making process. Comparing to the use of research evidence, more California school-based SLPs in this study reported they took the client’s values into consideration during their decision-making process. However, how the SLPs consider the client’s values and what values SLPs consider is worth further investigation. It is important to point out that parent's preference was reported as one of the most influential factors that may prevent California school-based SLPs from making ethical decisions. Therefore, how the clinicians find a balance between the student’s needs and the parent’s preferences is a challenging task that frequently leads to ethical dilemmas.
Autonomy is one of the bioethical principles that highlights the acknowledgement of a person’s right to make decisions based on his/her own values and beliefs. Since parent’s preferences play an important role in clinical decision-making processes, it is crucial for SLPs be conscious about the possible bias from parents’ preferences which may prevent them from providing the optimal clinical services.
California school-based SLPs’ perception on factors that may prevent them from making ethical clinical decisions when qualifying a student for speech and language services (Question 3)
Among the fifteen (15) factors that may prevent the school-based SLPs from making ethical decisions, our participants reported that five factors are more likely to prevent them from making ethical clinical decisions. These factors, rank from most strongly to less strongly related, are parent’s preference, school district’s policies, lack of support from administration, lack of collaboration with other IEP team members, and advice from more experienced colleagues.
As discussed above, parents’ preferences may become an ethical dilemma for school based SLPs. Ethical dilemmas arise frequently in clinical practice when values, principles, and norms are in conflict. Clinicians sometimes have to prioritize one ethical principle than the others to make a decision that maximize the benefits and reduce the harm while two or more principles and obligations are in conflict [27]. Clinicians should be aware of these possible dilemmas and conflicts and keep the dialogue open with parents and students when facing these challenges.
Our participants reported that several external factors related to school districts may play an important role in their clinical decisionmaking processes, such as school districts’ policies and lack of support from administrations. As suggested by Lopez et al. [23], economic constraints (i.e. reimbursement policies) may impede the implementation of the most effective care plans. Therefore, they suggested that clinicians should be aware of the interrelationship among economics, ethics, independent professional judgment, and EBP and how economic factors may affect professional judgment and ethical decision-making. The results of this study can bring these external factors to school-based SLPs’ attention, so they have to be carefully taken these factors into consideration during decisionmaking processes.
According to ASHA (2002), workload is defined as time spent on direct and indirect services to students, such as documentation, collaboration and planning on RTI and classroom based intervention, IEP meetings, and so forth. Excessive caseload and workload have been reported to have a negative impact on the implementation of EBP and the ability to provide the best possible service. A few studies also indicated that caseload or workload can have a negative impact on service delivery model and the quality of service in schools. Thus, it is fascinating to discover that most of our participants reported that their caseload or workload did not have a notable impact on making an ethical decision. Majority of the participants (41.4%) reported their average caseload of 50-59 students followed by less than 50 students (28.6%), which can be considered a relatively manageable caseload. Kats suggest an unmanageable caseload consists of more than 55 students. Additionally, 2014 ASHA School Survey results revealed that nearly 50% of school-based SLPs reported that optimal service may not be delivered due to multiple reasons, including excessive paperwork and high caseloads/workloads, and limited time to incorporate optimal service delivery models. Because our participants’ caseload is relatively manageable, they may not feel caseload or workload has a significant impact on preventing them from making ethical clinical decisions.
According to the results of 2014 ASHA School Survey, 77-83% school-based SLPs reported increased caseload/workload. Kats also indicated caseload remained to be a concern for school-based SLPs. Although ASHA no longer recommend a specific caseload number, only five states including California, Florida, Michigan, Ohio, and Virginia, have the median caseload size beyond 55. Although the majority of our participants did rate the caseload and workload as significant influential factors, school-based SLPs should understand that caseload and workload can have a negative impact on their clinical practice. ASHA has been promoting that reasonable workload is required and essential for SLPs to be productive in all required activities and duties (ASHA, n.d.).
Clinical implications
Although ASHA Code of Ethics and evidence-based practice have been incorporated into SLP training programs, an SLP’s ethical reasoning may not develop concurrently with clinical experience and skills [22,25]. Therefore, the training and continuing education about implementation of ethical principles and evidence based practice should be offered on a regular basis to support the development of optimal clinical decision-making skills. It is also recommended that SLPs should review ASHA Code of Ethics, bioethical principles, and ethical decision-making models when encountering ethical dilemmas to brainstorm best solutions. It is imperative to highlight the interconnection between ethical principles and evidence-based practice because ethics provides an important context for evidencebased practice and both ethical practice and professional competence are rooted in evidence-based practice [11]. The ethical principles and EBP guidelines should be reviewed on a regular basis because our findings indicated that training in EBP are strongly related to making ethical clinical decisions. Therefore, ASHA evidence map, ASHA Learning Portals, Code of Ethics and Position Statements should not only be integrated into SLP graduate training programs, but also highlighted in continuing education courses and professional learning communities. Because ASHA Code of Ethics is a general guideline, it does not provide explicit guidelines for complex clinical issues. The implementation of ethical and evidence-based practice requires additional support, such as case studies and training on incorporating ethical principles into clinical decision-makings. Additionally, school districts may develop specific guidelines to assist clinicians managing complex clinical issues and ethical dilemmas. Workshops can be offered to include a comprehensive review of possible constraints that can prevent SLPs from making ethical decisions and offer feasible resolutions supported by administrations and school districts to facilitate the implementation of EBP and ethical principles.
Self-reflection can be used as a method to constantly evaluate the clinician’s own decision-making process and clinical practice. As suggested by Christiansen et al. [18] it is a professional and moral obligation to make a clinical decision based on ethical principles and EBP guidelines. Self-reflection and self-evaluation can facilitate the development of critical thinking and problem-solving abilities necessary to manage ethical dilemmas. During the self reflection process, clinicians can be more conscious about the factors that may prevent them from making an ethical clinical decision. This can support the development of possible solutions to overcome the clinical ethical dilemmas.
Limitations of the study
Similar to the studies of Dowden in the state of Washington and in the state of Vermont, our study intended to serve as an exploratory study investigating how California school-based SLPs implement evidence-based practice and their clinical decision-making processes. However, one of the significant limitation of our study is the small sample size. Only school-based SLPs who held ASHA's Certificate of Clinical Competence (CCC) and California state license were recruited, and the recruited participants only consist of about 2% of California school-based SLPs. This resulted in a weak external validity, so the results of this survey study may not generalize to all California school-based SLPs. For example, the results may not reflect the opinions of California school-based SLPs who do not hold ASHA’s CCC. Similar to survey studies utilized rating scales, a common limitation is the lack of qualitative information needed to understand the causes of various issues. It was also challenging to keep the survey concise but also comprehensive for collecting all required information. In addition, respondents may be biased or unable to provide truthful answers to the survey questions. Possible confounding factors include fatigue, avoidance of embarrassment, or favorability of the experimenter. Finally, the participant recruitment of this survey study was through distributing the survey link via emails sent to school districts across the state of California and ten California Speech- Language-Hearing Association districts. Despite the survey was available for about three months, a few California school-based SLPs approached the principle investigator after the closure of this survey. There may be more SLPs were not even aware of this survey study.
Future research
Future research should consider replicating this study in other states or through a national survey to increase the reliability, validity, and significance of the study. In addition, collecting both quantitative and qualitative data is recommended in order to draw on the strengths of both approaches. The inclusion criteria can also be expanded to all school-based SLPs to reflect more accurate perceptions on the practical issues in this population. Moreover, survey questions can be revised to more specially ask how respondents implement evidence-based practice guidelines and ethical principles in clinical practice and their perceptions on the interconnection between evidence-based practice and ethical clinical conducts. For example, questions can explore how clinicians incorporate the client's values and what values clinicians consider during the decision making processes. Our study did not focus on ethical dilemmas; therefore, it may be worthy to examine the level of constraints that prevent SLPs from making ethical clinical decisions and how school-based SLPs manage these ethical dilemmas since most of the studies focused on clinicians in non-school settings [22,25]. Lastly, our study only analyzed the survey data using correlational analyses and frequencies among different factors. Future research may conduct a hypothesis testing to compare the perceptions from different groups of participants. For example, how differently monthly caseloads, years of experience, or school settings can impact on clinical decision making.
References
- Nicholls S , Newson A, Ashcroft R (2016) The need for ethics as well asevidence in evidence-based medicine. J Clin Epidemiol 77: 7-10.
- Gillam SL, Gillam RB (2006) Makingevidence-based decisions about child language intervention in schools. LangSpeech Hear Serv Sch 37: 304-315
- PorzsoltF, Ohletz A, Gardner D, Ruatti H, Meier H, et al. (2003) Evidence-baseddecision making: The 6-step approach. A C P J Club 139: 1-6.
- Caty ME, Kinsella EA, Doyle PC (2016) Reflective practice inspeech-language pathology: Relevance for practice and education. CanadianJournal of Speech-Language Pathology and Audiology 40: 81-91.
- Schmitt M, Justice L (2012) Evidence-based practice:A retrospective overview and proposal for future directions. EBP Briefs 7: 1-6.
- Togher L,Yiannoukas C, Lincoln M, Poer E, Munro N, et al. (2011) Evidence-based practicein speech-language pathology curricula: A scoping study. Int Speech Lang.Pathol 13: 459-468.
- Kummer A,Turner J (2011) Ethics in the practice of speech-language pathology in healthcare settings. Semin Speech Lang 32: 330-337.
- PayneKT (2011) Ethics of disability: Foundation of the profession ofspeech-language pathology. Semin Speech Lang 32: 279-288.
- Horner J(2003) Morality, ethics, and law: Introductory concepts. Semin Speech Lang 24:263-274.
- Chaborn S, Morris J, Lemoncello R(2011) Ethical deliberation: A foundation for evidence- based practice. SeminSpeech Lang 32: 298-308.
- Sharp H, Genesen L (1996) Ethicaldecision-making in dysphagia management. Am J Speech Lang. Pathol 5: 15-22.
- Schreck J (2015) A bioethics primerfor speech-language pathologists and audiologists working with older adults.Amer J Speech-Lang Pathol Special Interest Group 15 Perspectives on Gerontology20: 4-10.
- Brady L, Kirschner K (1995) Ethicalissues for persons with aphasia and their families. Top Stroke Rehabil2:76-83.
- Goldsmith T(1999) Ethical issues facing the speech-language pathologist in the acute caresetting. American Speech-Language Pathology Special Interest Group 2Neurophysiology and Neurogenic Speech and Language Disorders 20-24.
- Cox DJ (2012) From interdisciplinaryto integrated care of the child with autism: The essential role for a code of ethics.J Autism Dev Disord 42: 2729-2738.
- Christiansen C, Lou J (2001) Ethicalconsiderations related to evidence-based practice. Am J Occup Ther 55: 345-349.
- Borry P, Schotsmans P, Dierickx K (2006)Evidence-based medicine and its role in ethical decision-making. J Eval ClinPract 12: 306-311.
- StrechD (2008) Evidence-based ethics: What it should be and what it shouldn’t. BMCMedical Ethics 9.
- TannahillA (2008) Beyond evidence-to ethics: A decision making framework for healthpromotion, public health and health improvement. Health Promotion International23: 380-390.
- KennyB, Lincoln M, Balandin S (2010) Experienced speech-language pathologists’responses to ethical dilemmas: An integrated approach to ethical reasoning. AmJ Speech Lang Pathol 19: 121-134.
- Lopez A, Vanner E, Cowan A, Samuel A, Shepherd D (2008)Intervention planning facets-Four facets of occupational therapy interventionplanning: Economics, ethics, professional judgment, and evidence-based practice.Am J Occup Ther 62: 87-96.
- Jette D,Bacon K, Batty C, Carlson M, Ferland A,et al. (2003) Evidence-based practice:Beliefs, attitudes, knowledge, and behaviors of physical therapist. Phys Ther83: 786-805.
- Kenny B,Lincoln M, Blyth K, Balandin S (2009) Ethical perspective on quality ofcare: The nature of ethical dilemmas identified by new graduate and experiencedspeech pathologists. Int J Lang Commun Disord 44: 421- 439.
- Whitmire K, Rivers K, Mele-McCarthyJ, Staskowski M (2014) Building asevidence based for speech-language services in the school: Challenges andrecommendations.
- Flatley D,Kenny B, Lincoln M (2014) Ethical dilemmas experienced by speech-languagepathologists working in private practice. Int J Speech Lang Pathol 16: 290-303.
- American Speech-Language-Hearing Association(2016) 2016 Schools Survey report: SLP caseload characteristics
Citation: Sun L, Hung PF (2018) School-Based Speech-Language Pathologists' Clinical Decision-Making Process in the State of California. J Speech Pathol Ther 3: 133. DOI: 10.4172/2472-5005.1000133
Copyright: © 2018 Sun L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 7576
- [From(publication date): 0-2018 - Apr 03, 2025]
- Breakdown by view type
- HTML page views: 6690
- PDF downloads: 886