School children's Lifestyle Behaviours and Their Predictors: Healthy Weight Development Model in Urban Indonesia
Received: 16-Sep-2017 / Accepted Date: 09-Oct-2017 / Published Date: 16-Oct-2017 DOI: 10.4172/2375-4494.1000358
Abstract
Objectives: Child obesity, a major risk factor of non-communicable diseases such as diabetes or heart diseases, has become a major health issue in Indonesia, especially in the wake of economic growth. Nevertheless, child obesity prevention programs and relevant information is limited. Our study aimed to investigate child obesity status, lifestyle behaviours (LSBs) and their predictors, and their structures, in order to develop a model to discuss a collaborative healthy weight development program for schoolchildren in urban Indonesia. There were two objectives of our study: (1) In order to investigate schoolchildren's obesity status, LSBs, and their predictors and (2) In order to examine relationships among schoolchildren's obesity status, LSBs, and their predictors in urban Indonesia.
Methods: The design was a cross-sectional study using physical measurement tools and an 82 item selfdeveloped questionnaire based on interviews for 9 to 11 year old school children in 2015. Sampling included 5 schools resulting in 594 eligible students with 579 (97.5%) responding. Collected data were analyzed by descriptive statistics and a structural equation modeling. The Research Ethics Committee of St. Luke's International University (Approval Number 15-036) approved our study.
Results: Physical measurement classified participants 40% as obese or overweight and 35% as underweight. Descriptive statistics revealed limited behaviours and environments in access to snacks, physical activity (PA), weight-monitoring, obesity education, and support. The models by type of schools and by sex (CFI=0.88-0.91) indicated; boys' trouble sleeping (β=-0.18), private schoolchildren's frequency of junk and outside foods (β=-0.18 and -0.19) predicted Body Mass Index. Safe-PA environment (β=0.17-0.48) and family support (β=0.36-0.59) predicted PA LSBs. For girls, PA-peer presence predicted PA LSBs (β=0.88).
Conclusion: These findings could help developing the effective obesity-prevention programs such as healthy dietary environment, safe-PA-environment, PA-peer-group support for girls, family-involved dietary-PA interventions in urban Indonesia.
Keywords: Child; Obesity; Body weight; Lifestyle; Indonesia
Introduction
Child obesity, a major contributor to adult obesity and the global burden of non-communicable diseases (NCDs), is one of the biggest health issues in the world [1]. Obesity is mainly caused by the lifestyles comprising excessive calorie intake and physical inactivity. It is generally preventable and irreversible change once established [2]. The number of obese or overweight children from the ages of two to 19 increased 26%, from 246 million in 1993 to 311 million in 2013 in the world [3]. Of these children, 83% or 257 million live in low- or middleincome countries [3]. These countries are suffering from a “double burden of malnutrition”; over-nutrition and under-nutrition [4].
Indonesia as a lower-middle income country has experienced socioeconomic changes since the 1990s. Indonesia’s gross domestic product per capita, has increased 5-fold (from 960 USD to 5,214 USD) during the last 30 years [5]. NCDs also have increased from 45% in 1990 [3] to 71% in 2014 [1]. Almost all Indonesians can access highcalorie foods, and 30% of them demonstrate physical inactivity [6]. Average overweight or obesity rate of Indonesian children aged 5-12 is 19% [7].
Indonesia’s child obesity is one of the biggest health issues. Most of the Indonesian lives in urban areas (51%) and Java Island (57%) [8]. Regardless of rural or urban locations, almost all Indonesians are accessible with high-calorie foods, and 30% of them demonstrated physical inactivity [6]. The percentage of overweight or obesity of Indonesian children (5 to 12 years old) was 19%, but in the capital city of Jakarta, has the highest rate at 30%, and the rate is also relatively higher in Java Island in 2013 [9]. Thus, child obesity prevention programmes are especially needed in urban areas.
Although the Indonesian Ministry of Health developed “Guidelines of Schoolchild Overweight and Obesity Prevention” for schoolchildren [10], these guidelines have not been implemented in schools. Thus, developing child obesity prevention programmes in Indonesia is a pressing issue.
Our study aimed to investigate the structures of the child obesity status, lifestyle behaviours (LSBs) and their predictors, and their structures, in order to develop a model to discuss the collaborative obesity prevention programmes for schoolchildren in urban Indonesia. Objectives were as follows: (i) To investigate schoolchildren’s obesity status, LSBs, and their predictors and (ii) To examine relationships among schoolchildren’s obesity status, LSBs, and their predictors in urban Indonesia.
Methods
Study design
Cross-sectional study using physical measurement tools and an 82 item self-developed questionnaire based on interviews was conducted in September 2015 in South Tangerang city, of Banten Province, Indonesia. Participants’ criteria were 9 to 11 year old school children (from the fourth to the sixth graders of the private and national elementary schools) with no chronic diseases or no medication, and who live in the target area by stratified sampling.
Sample size
Sample size was estimated as follows. An interactive two-sided correlation coefficient was calculated based on taking the alternative hypothesis. The researchers set the level of statistical significance at α=0.05, and the power 0.80 (β=0.20), to deny no correlation. Because of limited studies in middle-income countries, the correlation coefficients between lifestyle and BMI were approximately 0.26 to 0.45, following studies conducted in the USA [11,12]. According to the calculation, the needed sample size was 123. Considering an 80% expected response rate, the tentative sample size was 154. This number was based on Hulley’s [13] calculation.
There were various methods of sample size calculation for factor analysis. In this study, researchers followed Polit and Beck [14], who recommended estimating 10 participants per item. The questionnaire contained 82 items; therefore, the sample size could be 820. Considering an 80% response rate, the tentative sample size needed to be 1,025.
Nunnally and Bernstein [15] suggested 300 as adequate for factor analysis. Considering an 80% expected response rate [14], the tentative sample size was 375.
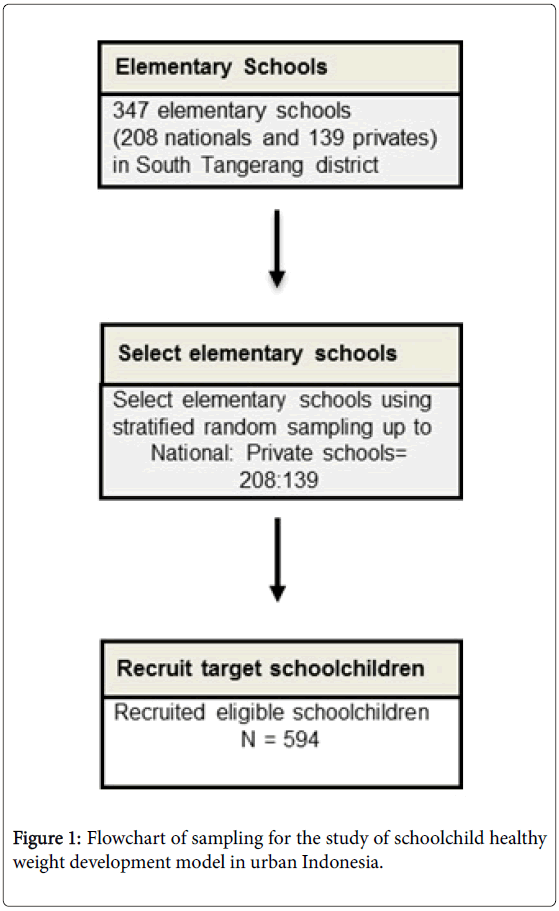
Comparing these sample size, recruiting 1,025 participants was unrealistic in terms of the budget and data management; a total of 154 participants was too small to be representative and to support factor analysis. Therefore, researchers used a recruiting sample size of at least about 600 for this study. Amongst total 347 elementary schools of the target area, researchers randomly selected amongst 208 national and 139 private schools at the same proportion, which are 60%: 40%. Finally, 594 schoolchildren were recruited from these schools (Figure 1).
Participants including both girls and boys were recruited from the South Tangerang District of Banten Province. The number of schoolchildren in the South Tangerang District is 129,240. Using stratified sampling, about 600 school children (national:private=360:240), aged from 9 to 11 (fourth or fifth graders) were selected. Participants criteria was schoolchildren with no chronic diseases or no medication, and who live in the South Tangerang District of Banten Province. Approximately 43,080 of the fourth and the fifth graders live in the target area. Sampling procedure is shown in Figure 1. Stratified random sampling was conducted with three national and two private schools from 347 elementary schools (208 national and 139 private) for about 600 children (360 national and 240 private schoolchildren) in the South Tangerang District.
Study instruments
There were two measurement instruments in this study. One was the questionnaire and another was physical measurement tools.
Physical measurement tools: Participant physical measurement included the following: body mass index (BMI) and step counts. Data directly measured children’s obesity status. The BMI and step counts were the proxy measurement tools of child obesity. Some of these objective data provided the structure between the measurements and other lifestyle predictors of obesity and guided the model development.
Physical measurement tools were weighing scales (Innerscan 50 BC-309-PR, TANITA), height scales (Seca 206, Seca), and pedometers (HJ325, Omron). BMI was calculated by the following formula:
BMI=Weight in kg/ height in m2.
To avoid inaccuracy, weight measurements were taken without shoes or accessories and without heavy items in pockets. Additionally, participants were instructed not to look down and not to hold onto anything. In fact, the scale was guaranteed within 50 grams of accuracy. The scheduling of measurement was between the morning break and lunchtime.
BMI 25 kgm2 at 18 years old was also calculated to examine the obesity status. Major international BMI references were introduced by the International Obesity Task Force (IOTF) and the WHO. The WHO used the overweight cut-off based on age such as plus 2 SDs before age 5 and plus 1 SD after 5 years old gathering data from WHO growth standard and the National Center for Health Statistics (NCHS) 1977 growth reference [16]. IOTF used the data from children in six countries: Brazil, Hong Kong, the Netherlands, Singapore, the USA, and the U.K. IOTF’s overweight cut-off uses the country-averagedcentile corresponding values of BMI 25 at 18 years old [16]. Comparison of the IOTF and WHO cut-offs and revealed that WHO cut-offs estimates higher prevalence or sensitivity of obesity after 5 years old because the data was combined from less fat preschoolers and more fat childhood [16,17]. Bray and Bouchard [17] examined various references of obesity and recommended using IOTF tools when the data collection was conducted before obesity become common place. The researcher uses the IOTF international cut-offs because they consider Asian children’s growth and adjust after 5 years level. In this study, the level of BMI at 18 years level was named from 1 (thinness/underweight), 2 (normal), 3 (overweight), and 4 (obesity).
Height measurement was also done without any accessories or shoes and without any heavy items in pockets. The height scale’s accuracy was within 0.5 cm.
Step counts were measured seven day’s walking record for each student. The researcher instructed children to place pedometers in their right pockets with clips, not to shake them, and to behave as normally as possible. Accuracy was repeatable to within 5% variation. In assessing degrees of obesity, the cut-off for a normal BMI for an 18- year-old Asian is more than 18.5 and less than 23 [18]. The researcher referred to detailed cut-offs for exact ages by month, based on IOTF cut-offs [18].
Self-developed Questionnaire: Schoolchild obesity prevention predictors and lifestyles behaviors questionnaire were developed with 82 items which were consisted of 18 demographic data, 37 items (4- point scales), and 27 items (5-point scales) to examine the relationships among obesity status, LSBs, and predictors. The questionnaire’s content inquired about children’s daily lives, including the following lifestyle behaviors: dietary, physical activities, sleeping, and screen time. The questionnaire’s validity and reliability was tested in a pilot study.
Validity test (content and face validity) was conducted. About content validity, six experts as recommended [19], introduced by Indonesian collaborating faculty members of the UIN Syarif Hidayatullah Jakarta, Indonesian scholars of universities in Indonesia and health professionals in Indonesia were recruited to confirm content validity using the Content Validity Index (CVI) after obtaining consent of research participation. While reviewing the questionnaire, the recruited scholars or professionals rated a checklist using an index of a 4-point scale (1=not relevant to 4=highly relevant). Then, the researcher calculated the average content validity of individual items (I-CVIs), recommended to be 0.78 [19]. Content validity of the overall scale (S-CVIs) should be 0.90 or higher [19]. Average I-CVIs showed 0.92 and S-CVIs showed 0.92, too. Items with less than 0.78 in I-CVIs (Question number 24, 43, 52, 60, 65, 68, and 75) and 0.90 (None in the questions) in S-CVIs were discussed and revised with Indonesian researchers.
For testing face validity, one elementary school was selected. This school was excluded from the main study. In the target school, fourth and fifth graders were nominated as participants for the face validity test. The researcher checked the length of time to answer, comprehensibility, understandability, and respondent burden. This process was conducted with research assistants, and comments were noted. Less valid items were revised with Indonesian researchers. Length of time to answer was approximately 35 minutes on average including the rest. Few children complained about the length of the questionnaire, however, most of the cases children were happy to answer the questions because the research assistants kept entertaining them to be attracted to answer the questionnaire. Comprehensibility was checked by the research assistants and the wording of the questionnaire was modified so that children can comprehend and understand the meaning of the questions.
Reliability test was also conducted. First, details of the components of predictors are as follows. Components of predictors were categorized using principal component analysis. Twelve components were categorized from 35 items that measured predictors and components. Components with a Cronbach alpha less than 0.50 were excluded from the analysis. Five of the twelve components remained: knowledge of obesity, family, school, plus health center support, physical activity safety environment, efficacy control lifestyle behaviors, and family education and support. Reliability of predictors was examined to assess item consistency of instruments. Components with a Cronbach alpha less than 0.50 were excluded from the analysis. All five components were examined and the total Cronbach α of the predictors was 0.68. Predictors including knowledge of obesity, family, school, plus health center support, physical activity safety environment, efficacy control lifestyle behaviors, and family education and support are named as follows.
Knowledge of obesity: Six items were included in this component. This component was named knowledge of obesity because items included knowledge of obesity prevention.
Family, school, and health center support: Seven items were included in this component. This component was named family, school, and health center support because items included support or education from family, school, and or health center.
Physical activity safety environment: Three items were included in this component. This component was named physical activity safety environment because items included safety of exercise such as no fear of road accidents, air pollution, and or being kidnapped.
Efficacy control lifestyle behaviors: Four items were included in this component. This component was named efficacy control LSBs because items included efficacy of controlling dietary amount, exercise time, and screen-time.
Family education and support: Three items were included in this component. This component was named family education and support because items included family’s education and support of dietary and rest patterns toward children.
Second, details of the components of lifestyle behaviors are as follows. Reliability of lifestyle behaviors was examined to assess item consistency of instruments. All five components of lifestyle behaviors relating to obesity were examined and total Cronbach α was 0.70. Lifestyle behaviors such as PA preference, healthy diet, healthy sleep and rest, PA willingness, and fruits-vegetables preference were named as follows.
Physical activity preference: Three items were included in this component. This component was named ‘PA preference’ because items included prefer or not lazy exercising.
Healthy diet choices: Seven items were included in this component. This component was named ‘healthy diet’ because items included dietary contents, frequency, and eating style.
Healthy sleep and rest experience: Four items were included in this component. This component was named ‘healthy sleep and rest experience’ because items included rest pattern after the meal, daytime sleepiness, and staying up late.
Physical activity willingness: Three items were included in this component. This component was named ‘physical activity willingness’ because items included independent exercise behavior, exercise frequency, and length of exercise.
Fruits-vegetables preference: Two items were included in this component. This component was named ‘fruits-vegetables preference’ because items included preference of fruits and vegetables.
Ethical considerations: The Research Ethics Committee of St. Luke’s International University (Approval Number 15-036) approved the study. After the schools’ approval of research collaboration, principals of the sample schools delivered request letters for study participation, consent form, and withdrawal form to guardians. Guardians confirmed children’s own will and signed the consent form of participation on behalf of children if they decide to participate. Consented children brought forms back to their schools. Guardians were informed of the purpose, methods, advantages, disadvantages, contact information of the researchers in a written consent form. In case the child participants might not completely understand the research information, an oral explanation was provided using plain language at children’s level.
Results
Stratified sampling included five schools resulting in 594 eligible students with 579 (97.5%) responding. Girls were 48.9% and boys were 51.1%; national schoolchildren were 61.3% and private schoolchildren were 38.7%. Only 25% of them were normal weight and other 75% were overweight, obesity, or underweight (Table 1). Schoolchildren’s daily snack expenses were around one United States dollar which can be purchased 10 donuts in the snack shops. Time to the snack shops was around three minutes. At the same time, time to the sports facilities was around 8 minutes. Their step counts per day were around 6,500 steps. Sleep hours were around 8.2 hours.
| n (%) | |
|---|---|
| Participant schoolchildren | 579 (100) |
| Girls/ Boys | 283/296 (48.9/51.1) |
| National/ Private | 355/224 (61.3/38.7) |
| Normal weight | 146 (25.2) |
| Underweight | 199 (34.4) |
| Overweight | 106 (18.3) |
| Obesity | 129 (22.3) |
| Mean ± SD | |
| Age | 121.6 ± 7.9 |
| Body Mass Index at current age (kg/ ?) | 17.7 ± 3.9 |
| Snack expenses per day (U. S. Dollars) | 0.84 ± 0.52 |
| Minutes to snack shop | 2.9 ± 2.9 |
| Minutes to sports facility | 8.3 ± 4.5 |
| Step counts per day | 6,448 |
| Sleep hours | 8.2 ± 1.1 |
Table 1: Participants characteristics.
Structural equation modeling (SEM) was conducted by type of school and by gender to investigate the structures among obesity status, LSBs, and their predictors. In total, 10 latent variables (five LSBs and five predictors) consisting of 42 observed variables were entered into the model and the relationships among them were examined. Five components of the LSBs were categorized by three LSBs: dietary, physical activity, and sleep. Dietary LSBs consisted of two components: fruits-vegetables preference and healthy dietary. PA LSBs consisted of PA willingness and PA preference. Sleep LSBs consisted of sleeping and rest patterns. Observed variables with factor loadings of less than 0.35 were omitted from the model. All path coefficients in the model were statistically significant. Some models included a single observed variable from the results of the correlation analysis because the latent variables were not always the strongest subscales in the model.
Obesity status and lifestyle behaviors
‘No happy eating’ had a slight negative influence on BMI (β=-0.11; p=0.031).
Physical activity lifestyle behaviors and their predictors
‘PA safety environment’ and ‘family education and support’ had slight positive influences on PA preference LSBs (β=0.16; p=0.035 and 0.21; p=0.037, respectively). ’PA safety environment’, ‘family education and support’, and ‘Family, school, and HC support’ had positive influences on PA willingness LSBs (β=0.25, 0.43, and 0.36; p=0.019, 0.037, and 0.007, respectively).
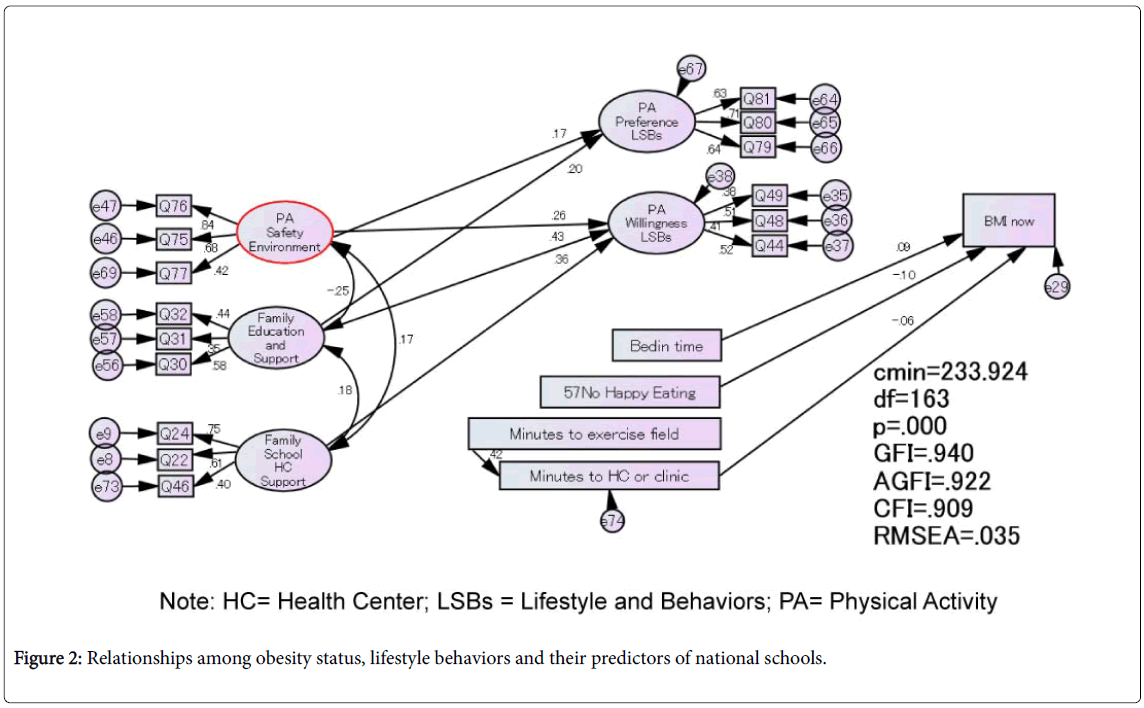
Structural equation modeling of national schools
SEM of the national schools was conducted. Goodness of model fit was evaluated by several fit indices. The p-value of Chi-square test was p=0.000; Confirmatory Fit Index (CFI) was 0.909; Goodness of Fit Index (GFI) was 0.940; Adjusted Goodness of Fit Index (AGFI) was 0.922; the root mean square error approximation (RMSEA) was 0.035 (Figure 2). In national schools, the predictor of dietary LSBs was ‘knowledge of obesity’. Predictors of PA LSBs were ‘family education and support’ and ‘family, school, and HC support’. The predictor of sleep LSBs was ‘family, school, and HC support’.
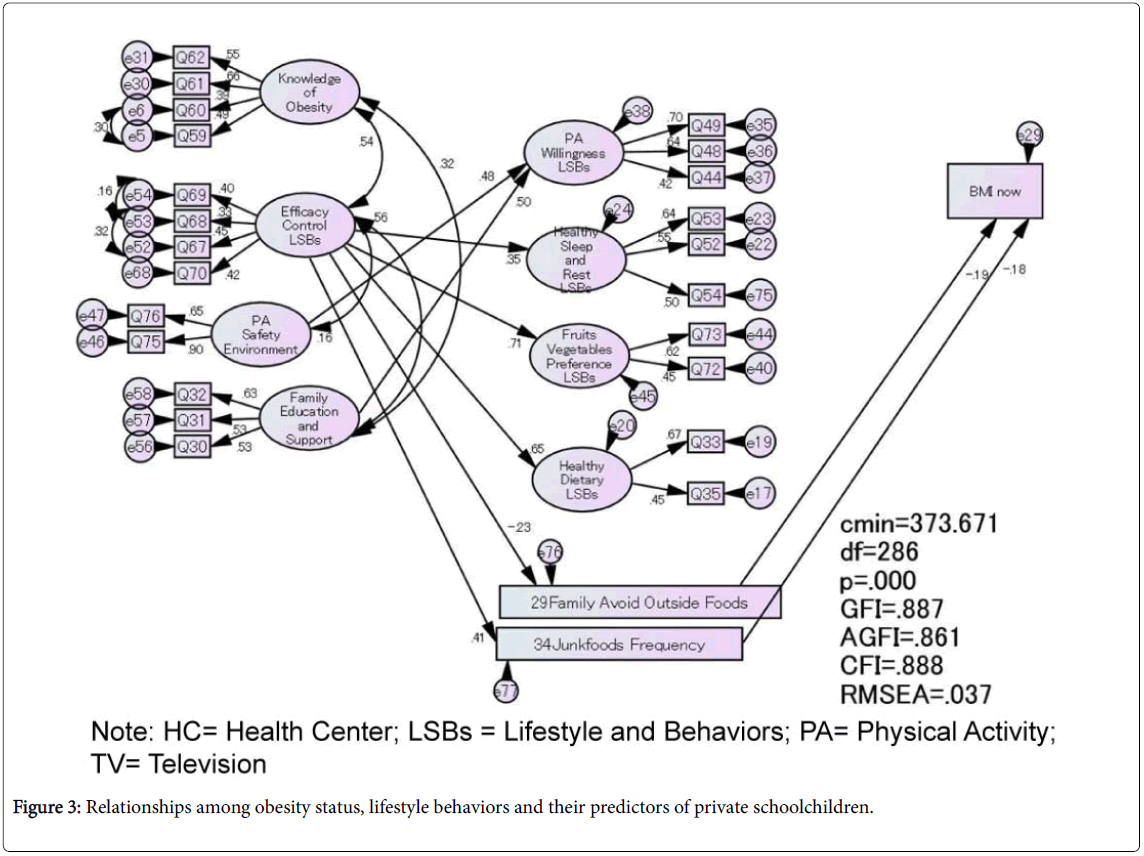
Structural equation modeling of private schools
SEM of private schoolchildren was conducted. The p-value of Chisquare test was p=0.000, CFI was 0.888, GFI was 0.887, AGFI was 0.861, and the RMSEA was 0.037 (Figure 3). In private schools, the predictor of dietary LSBs was ‘efficacy control LSBs’. Predictors of PA LSBs were ‘efficacy control LSBs’ and ‘PA safety environment’. The predictor of sleep LSBs was ‘efficacy control LSBs’.
Obesity status and lifestyle behaviors
‘Junk food frequency LSBs’ and ‘Family avoid outside foods’ had slight negative influences on BMI (β=-0.18 and -0.19; p=0.000 and 0.010, respectively). These LSBs decreased BMI in private schools.
Dietary lifestyle behaviors and their predictors
‘Efficacy control LSBs’ had strong positive influences on fruitsvegetables preference LSBs (β=0.71; p=0.000) and healthy dietary LSBs (β=0.65; p=0.000).
Physical activity lifestyle behaviors and their predictors
‘Family education and support’ and ‘PA safety environment’ had positive influences on PA willingness LSBs (β=0.50 and 0.48; p=0.000 and 0.000 respectively).
Sleep lifestyle behaviors and their predictors
‘Efficacy control LSBs’ had a positive influence on sleep and rest patterns LSBs (β=0.35; p=0.003).
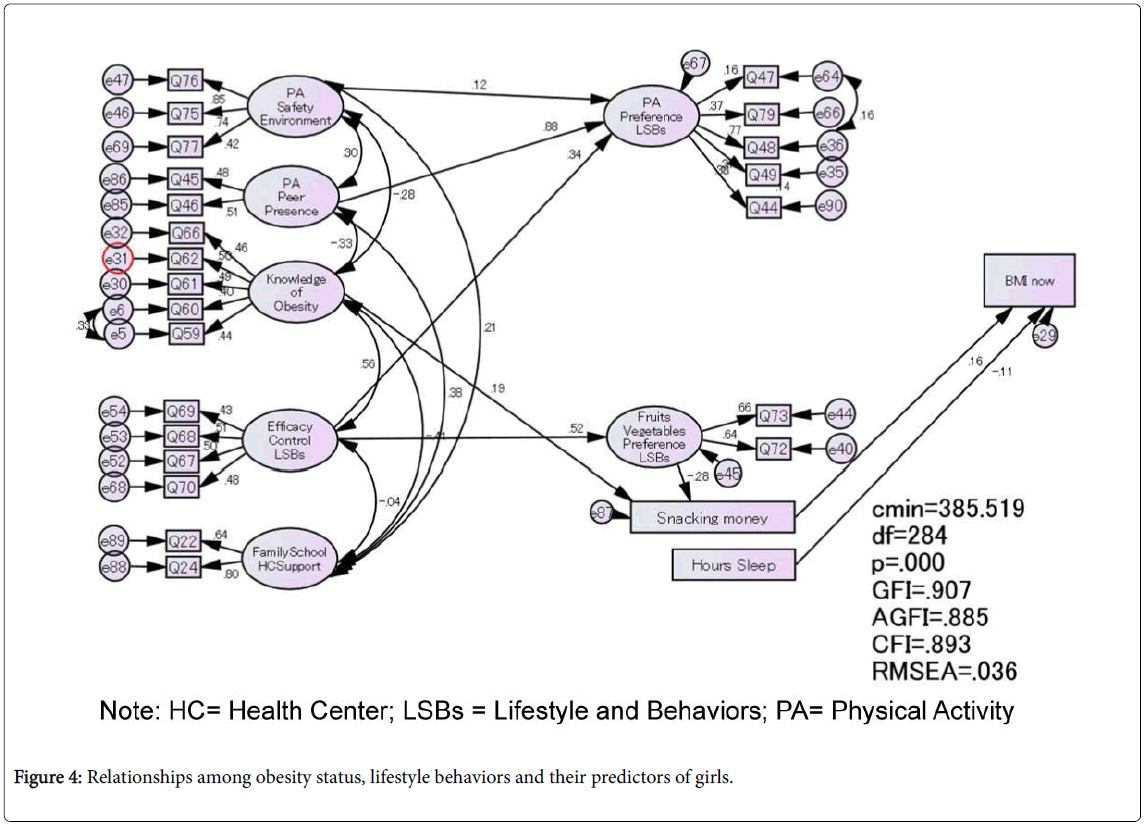
Obesity status and lifestyle behaviors
‘Sleeping hours’ and ‘snacking money’ had a slight positive influence on BMI (β=-0.11 and 0.16; p=0.010 and 0.001, respectively).
Dietary lifestyle behaviors and their predictors
‘Efficacy control LSBs’ had a positive influence on fruits-vegetables preference LSBs (β=0.52; p=0.000).
Physical activity lifestyle behaviors and their predictors
‘PA safety environment’, ‘PA peer presence’, and ‘Efficacy control LSBs’ had positive influences on PA preference LSBs (β=0.12, 0.88, and 0.34, p=0.025, 0.038, and 0.005, respectively).
Structural equation modeling for girls
SEM for girls was conducted. The p-value of Chi-square test was p=0.000, CFI was 0.893, GFI was 0.907, AGFI was 0.885, and the RMSEA was 0.036 (Figure 4). Regarding girls, the predictor of dietary LSBs was ‘efficacy control LSBs’. The predictor of PA LSBs was ‘efficacy control LSBs’. The predictor of sleep LSBs was ‘family education and support’.
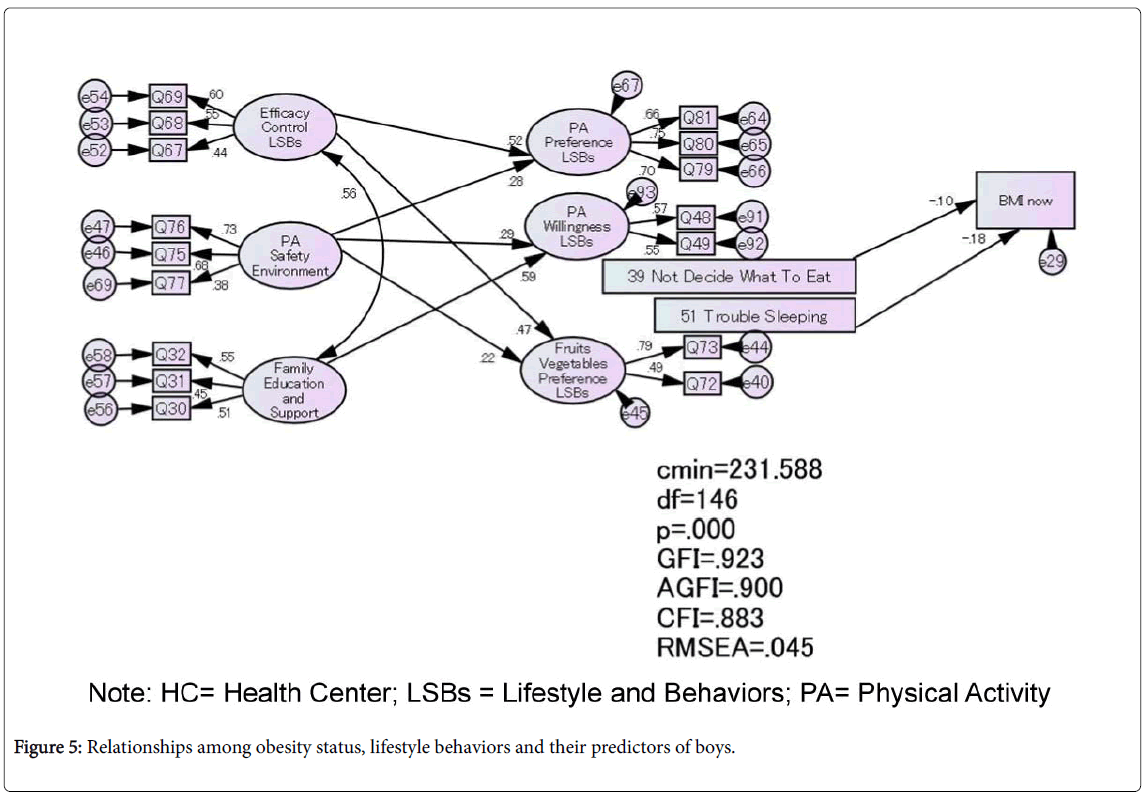
Structural equation modeling for boys
SEM for boys was conducted. The p-value of Chi-square test was p=0.000, CFI was 0.883, GFI was 0.923, AGFI was 0.900, and the RMSEA was 0.045 (Figure 5). Regarding boys, the predictor of dietary LSBs was ‘efficacy control LSBs’. Predictors of PA LSBs were ‘family education and support’ and ‘efficacy control LSBs’. The predictor of sleep LSBs was ‘family, school, and HC support’.
Obesity status and lifestyle behaviors
‘No trouble sleeping’, and ‘Not decide what to eat’ had slight negative influences on BMI (β=-0.18 and -0.10; p=0.005 and 0.044, respectively).
Dietary lifestyle behaviors and their predictors
‘Efficacy control LSBs’ had a positive influence on fruits-vegetables preference LSBs (β=0.47; p=0.000).
Physical activity lifestyle behaviors and their predictors
‘Efficacy control LSBs’ and ‘PA safety environment’ had positive influences on PA preference LSBs (β=0.52 and 0.28; p=0.000 and 0.000, respectively).
In summary, SEM by type of school, by gender, and by obesity status was conducted. The model revealed the relationships among obesity status, LSBs and their predictors. Most of LSBs positively influenced BMI.
Boys’ trouble sleeping (β=-0.18) was associated with obesity. Private schoolchildren’s consumption of junk and outside foods (β=-0.18 and -0.19) was associated with obesity. Safe PA environment (β=0.17-0.48) and family support (β=0.36-0.59) predicted PA LSBs. For girls, PA peer presence predicted PA LSBs (β=0.88).
Discussion
Our study found that severity of the obesity and overweight rate (40%), which was exceedingly higher than the national average. It was an alarming issue in target area. It was much higher than the obesity or overweightness of the Indonesian average and in Jakarta (19% and 30%, respectively) of 5 to 12 years old in 2013 [20].
Obesity prevention in Indonesia is an alarming issue like in other low- and middle-income countries. The number of obese and overweight children from the ages of 2 to 19 increased 26% in these 20 years and 83% or 257 million live in low- or middle-income countries [3]. Obesity and overweight rates in these emerging countries [1] such as Mexico, Brazil, Turkey, and Malaysia (68, 52, 62, and 44%, respectively), all of which attained economic growth prior to Indonesia might predict the future risk scenario for Indonesia. It seems clear that earlier obesity prevention is needed.
Our study showed that the participant schoolchildren might exceed their calorie intake because of their enough pocket money and snack accessibility. Conversely, they have a lack of exercise such as less stepcounts than average (10,000 steps or more) and have less accessibility to the sports facilities. They also sleep less than ideal sleeping hours (9 to 11 hours per day).
Our study also revealed the predictors of obesity of boys and private schoolchildren. Boys’ short sleep can be associated with their long screen time such as playing TV games or using smart phones.
Our study also showed the predictors of PA LSBs. Children refrain playing outside because of road accidents. The number of cars and motorcycles has significantly increased, and air pollution is so severe that people wear surgical masks in town. Undisciplined drivers and the car-dominant traffic system cause frequent road accidents, hence, threatening pedestrians. Approximately 8% of Indonesians die of accidental injuries [3]. In 2010, the number of road traffic deaths was 31,234 [21], the highest in Southeast Asia and the eighth highest in the world.
Implementations of healthy weight development programmes are a pressing issue because of the rapid lifestyle changes in Indonesia. There are three foci to tackle this challenge: (i) development of the school health system; (ii) implementation of the healthy weight development programme at school and community; and (iii) development of a healthy weight environment.
School health system development in Urban Indonesia
Needs of health educations were shown in the model that ‘family education and support’ and ‘family, school, and health centre support’ had an influence on LSBs in all schools, gender, and obesity status. A school health system, which can implement the healthy weight development programmes is needed. Installation of equipment such as physical activity monitoring and weighing scales is needed. Development of school health human resources such as school health nurse, nutritionist, and health center staff are needed. Development of the training programme for human resources such as school health nurses, nutritionists, and health center staff are also required.
Healthy weight development programme implementation
Programme development focusing on predictors is needed at homes, schools, community, and national policy levels. Results of this study showed the importance of PA, dietary, and sleep LSBs. PA and dietary combination support groups at community and school level are needed. A previous study showed dancing [22] and school vegetable garden [23] interventions were effective in reducing BMI. School meal programme is also a possible programme so that children can learn appropriate dietary contents, eating style, and frequency such as the one implemented in Vietnam [24].
During the dissemination of this study, researchers observed that children really respected their teachers at schools. Therefore, schoolled programmes seemed to be effective in implementing the programme. We also observed that children also love dancing with music in target schools. Healthy weight programmes such as growing vegetables, cooking class with those grown vegetables with their guardians, and dancing with music during morning assembly, led by teachers are recommended by school health stakeholders.
Healthy environment development
Accessibility to healthy foods environment: Children reported enough knowledge and efficacy regarding eating behaviours, however they also reported high snack expenses. This lifestyle behavior predicted obesity status especially in private school. Food environment was obesogenic in terms of accessibility and affordability. For accessibility, by replacing healthier foods in canteens or small shops inside and outside schools could provide healthier foods to children. For affordability, education for parents about the pocket money for snacks is needed. In addition, education for better choice of foods is needed from an earlier period. Dietary education should include such information and practice as how to read food labels, healthy contents of foods, amount and frequency of food intake.
Physical activity safety environment: The model showed PA safety environment was an important predictor of PA LSBs. Safer road conditions, development of public sports facilities, and a safer society for children could be provided by the government and the community so that children have no worries about accidents. Formulating PA peer support group in the community and schools are recommended so that children could feel safe and be motivated to exercise.
Girls’ physical activity peer support environment: The model showed girls’ invited physical activity behaviors. Generally girls feel unsafe if they do not exercise with some friends outside. Presence of friends or family motivated girls to exercise, therefore peer support and maintenance are important to promote PA.
Good sleep environment: Descriptive statistics showed children’s short sleep. The model identified sleep lifestyle behaviors influenced on obesity status. Meta-analysis of 696 studies on obesity and sleep also revealed that children with short sleep had nearly double the risk of obesity than normal sleepers (OR: 1.89; 95% CI: 1.46-2.43; p<0.0001) [25]. Long screen-time could be a possible predictor of short sleep although there were no correlations between screen-time and sleep LSBs in the model. Education for screen-time reduction such as no television or computers in the child’s room means involving the family in the decision.
Several limitations of our study should be acknowledged. The study design of this study was a cross sectional study. We tried our best to represent the target population correctly. However the results of our study were generalizable only among the participant children, and they may not be applicable to those who were out of the range. Future comparisons among different prefectures, different ethnic groups, and different countries are inevitable. In addition, future programme implementation based on this cross sectional study is needed to test the effectiveness of this child obesity prevention model.
Conclusion
There were two major findings from this study. First, the study provided a description of schoolchild weight status, lifestyle behaviors relating to weight status, and their predictors in urban Indonesia. Second, the study identified the relationships among schoolchild weight status, lifestyle behaviors, and their predictors and developed a child healthy weight model for South Tangerang District, Banten Province, Indonesia.
The theoretical framework based on the PRECEDE-PROCEED model, a literature review, and the interview was tested using the structural equation modeling. The framework assumed there were associations between and among weight status, lifestyle behaviors, and their predictors; The framework also assumed that weight status was predicted by lifestyle behaviors; lifestyle behaviors were predicted by lifestyle behaviors predictors.
Schoolchildren had accessibility and affordability to small snack shops, limited access to sports facilities, limited exercise (stepcounts), less sleep, and lot of screentime (TV and games).
Development of school child healthy weight programmes to promote or support healthy lifestyle behaviors are needed. At government level, it is recommended to develop healthy dietary environment, physical activity safety environment, and school health system to implement obesity prevention programme. At programme level, it is necessary that PA and dietary combination programme such as school meal, peer physical activity group, obesity education involving family and students at community and school level.
This study contributed to provide information on schoolchild obesity status, obesity prevention lifestyle behaviors, and their predictors in urban Indonesia.
In summary, our analysis suggested that healthy lifestyle education for schoolchildren, safe PA environment, and peer PA group would be effective in future healthy weight development programme.
Acknowledgments
We thank the participant children and their guardians, school staff, and all research assistants of the UIN Syarif Hidayatullah Jakarta. This study was funded by the JSPS Grant-in-Aid for Young Scientists (Startup) research, a Research Fellowship Programmes of the UIN Syarif Hidayatullah Jakarta, a Yamaji Fumiko Professional Nursing Education and Research Foundation, a Ogura Kazuharu Memorial Nursing Research Fund, and St. Luke’s International Studies Fund. Funding sources have no roles.
References
- World Health Organization (2014) Commission on Ending Childhood Obesity.
- Luttikhuis H, Baur L, Jansen H, Shrewsbury VA, O'Malley C et al. (2009) Interventions for treating obesity in children. Cochrane Database Syst Rev.
- Institute for Health Metrics and Evaluation (2014) Global Burden of Disease (GBD) Visualizations.
- Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, et al. (2013) Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 382: 427-451.
- World Health Organization (2014) Noncommunicable Diseases (NCD) Country Profiles.
- Ministry of Health Republic of Indonesia (2013) Indonesia Basic Health Research.
- Ministry of Health Republic of Indonesia (2013) Health Minister Decree No.30/2013 on Information and Daily Suggestion of Sugar, Salt and Fat in Labelling for Processed and Fast Food.
- Ministry of Health Republic of Indonesia (2012) Child Healthy Weight Development Model in Indonesia. Guidelines of School child Overweight and Obesity Prevention.
- Grimes C, Riddell L, Campbell J, Nowson C (2013) Dietary Salt Intake, Sugar-Sweetened Beverage Consumption, and Obesity Risk. Pediatr 131: 14-21.
- Rutkowski EM, Connelly CD (2011) Obesity Risk Knowledge and Physical Activity in Families of Adolescents. J Pediatr Nurs 26: 51-57.
- Hulley SB, Cummings SR, Browner WS, Grady DG, Newman TB (2001) Designing clinical research: An epidemiologic approach (2nd edn.), Lippincott Williams & Wilkins, Philadelphia.
- Polit DF, Beck CT (2012) Essentials of nursing research: Appraising evidence for nursing practice (8th edn.), Lippincott Williams & Wilkins, Philadelphia.
- Nunnally JC, Bernstein IH (1994) Psychometric theory (3rd edn.), McGraw-Hill, New York.
- Cole TJ, Lobstein T (2012) Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obesity 7: 284-294.
- Bray G, Bouchard C (2014) Handbook of Obesity. Taylor & Francis CRC Press, Boca Raton, Florida.
- International Obesity Task Force (2014) Extended International (IOTF) Body Mass Index Cut-Offs for Thinness, Overweight and Obesity in Children.
- Polit DF, Beck CT, Owen SV (2007) Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Res Nurs Health 30: 459-467.
- World Health Organization Country Office for Indonesia (2014) Injury Prevention.
- Fitzgibbon ML, Stolley MR, Schiffer L, Van Horn L, Kaufer Christoffel K, et al. (2005) Two-year follow-up results for Hip-Hop to Health Jr.: A randomized controlled trial for overweight prevention in preschool minority children. J Pediatr 146: 618-625.
- Centers for disease control and prevention (2014) School-Based Obesity Prevention Strategies for State Policymakers. Child Healthy Weight Development Model in Indonesia.
- Le DS, Trung N (2012) School meal program in Ho Chi Minh City, Vietnam: Reality and future plan. Asia Pac J Clin Nutr 21: 139-143.
- Cappuccio FP, Taggart FM, Kandala N, Currie A, Peile E, et al. (2008) Meta-analysis of short sleep duration and obesity in children and adults. Sleep 31: 619-626.
Citation: Ogata A (2017) Schoolchildren’s Lifestyle Behaviours and Their Predictors: Healthy Weight Development Model in Urban Indonesia. J Child Adolesc Behav 5: 358. DOI: 10.4172/2375-4494.1000358
Copyright: © 2017 Ogata A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 5346
- [From(publication date): 0-2017 - Apr 05, 2025]
- Breakdown by view type
- HTML page views: 4452
- PDF downloads: 894