SARS-CoV-2 Infections among Crew Members on Board PassengerVoyaging Cruise Ships during a Period of Delta Variant Predominance United States, June-October 2021
Received: 22-Dec-2022 / Manuscript No. omha-22-84441 / Editor assigned: 26-Dec-2022 / PreQC No. omha-22-84441 / Reviewed: 10-Jan-2023 / QC No. omha-22-84441 / Revised: 16-Jan-2023 / Manuscript No. omha-22-84441 / Published Date: 25-Jan-2023 DOI: 10.4172/2329-6879.1000446
Abstract
Objective: Cruise line operations were suspended in U.S. waters due to the COVID-19 pandemic. We describe demographic characteristics, time since completion of a primary series of COVID-19 vaccine and working conditions of crew members testing positive for SARS-CoV-2 following resumption of passenger operations in the United States during a period of Delta variant predominance.
Methods: Ships sailing under CDC’s Framework for Conditional Sailing Order reported SARS-CoV-2 test results, vaccination rates, and hospitalizations/medical evacuations due to SARS-CoV-2 infection to CDC daily. Ships experiencing large outbreaks (≥20 SARS-CoV-2–positive cases among crew/passengers within 14-days) submitted additional case data.
Results: During June-October 2021, 1,079 SARS-CoV-2-positive crew members were reported to CDC; 402 cases from large outbreaks had case-level data and were included in this analysis. All crew members completed a primary series of COVID-19 vaccine before they were infected. Median number of days from completion of a primary series of COVID-19 vaccine to infection was 76 days (interquartile range [IQR]:53–98). Most crew received the Janssen vaccine (n=302; 76%), and Janssen vaccine recipients had lower median number of days from last vaccination to infection than recipients of vaccines from other manufacturers [75 days (IQR: 55–87) vs. 86 days (IQR: 46–125; p=0.03)]. No hospitalizations or medical evacuations for SARS-CoV-2 were reported; 263 infected crew (65%) were asymptomatic at time of testing. Forty percent of infected crew shared either a cabin or restroom with another crew member at time of diagnosis.
Conclusion: We analyzed cases of SARS-CoV-2 infections during the Delta-predominant period among crew members associated with large outbreaks on passenger-voyaging ships. Severe illness was rare and most crew was asymptomatic; however sharing closed spaces with other crew members might increase the risk of exposure to SARS-CoV-2. Enhancements to existing COVID-19 mitigation measures and facilitating booster vaccination might reduce the risk of infections and severe illness in such congregate settings.
Introduction
Cruise ships are residential congregate settings with high risk of transmission of SARS-CoV-2 due to frequent contact and shared spaces with passengers and crew [1]. In March 2020, outbreaks of SARSCoV- 2 on cruise ships resulted in an unprecedented suspension of cruising in the United States under the Centers for Disease Control and Prevention (CDC) No Sail Order (NSO) [2, 3]. In June 2021, passenger operations resumed in U.S. waters as part of the phased approach outlined in the CDC’s Framework for Conditional Sailing Order (CSO) which allowed cruise lines to offer voyages under a comprehensive set of requirements [4,5]. Cruise ships choosing to enter U.S. waters were required by the CSO to follow technical instructions aimed at reducing the introduction and spread of SARS-CoV-2 on board cruise ships to align with national health and safety protocols.
In 2020 COVID-19 outbreaks on cruise ships resulted in hundreds of confirmed cases among passengers and crew, including fatalities [6]. In the first five months of 2021, during the period of the pandemic before the emergence of the Delta variant, SARS-CoV-2 crew attack rates and severe disease associated with COVID-19 decreased on cruise ships. This decrease in disease prevalence among crew occurred at a time of increased vaccine availability, implementation of CSO interventions, and additional efforts from the cruise industry to manage outbreaks [1, 7-9]. An investigation of four COVID-19 outbreaks, occurring during the period of Delta variant predominance, onboard passenger-voyaging cruises operating under the CSO reported attack rates among crew ranging from 6.0% to 11.1% [8]. Similarly, a Delta variant outbreak among a 98% vaccinated crew aboard a U.S. Navy ship after a port visit in Iceland resulted in a 6% attack rate [9].
Reducing the risk of infection among crew is essential to the continuation of safe cruise travel. Crew members remain on board for months at a time, have limited access to health care beyond what is available on the ship, and work in conditions that could increase their risk of exposure [10,11]. In this report, we use case investigation data to describe the demographic characteristics, vaccination history, living and working quarters, and numbers of crew member close contacts identified per crew member case during the period of Delta variant predominance following the resumption of passenger operations in the United States.
Method
Setting
Under the CSO, cruise ships were defined as commercial, noncargo, passenger-carrying vessels subject to the jurisdiction of the United States with the capacity to carry ≥250 individuals (passengers and crew) and an itinerary anticipating, at a minimum, an overnight stay onboard or a twenty-four (24) hour stay onboard for either passengers or crew [5]. Cruise lines operating under the CSO were required to follow CDC technical instructions developed specifically for cruise ships including: 1) onboard surveillance to identify passengers and crew with COVID-19 and COVID-19-like illness (CLI); 2) implementation of vaccination strategies; 3) training all crew on COVID-19 prevention, mitigation, and response activities; 4) onboard isolation and quarantine; 5) COVID-19 diagnostic and screening testing following CDC technical instructions; 6) onboard medical staffing and resources; and 7) procedures for the disembarkation of passengers who tested positive for SARS-CoV-2 [5].
Analysis Design
Cruise ship healthcare personnel conducted specimen collection and SARS-CoV-2 testing with nucleic acid amplification test (NAAT) or antigen tests. The CSO required crew members are tested every one or two weeks per ship attack rate and before disembarkation. SARSCoV- 2 testing was also performed at the ship’s medical center for close contacts of crew members with a positive NAAT or antigen test result or crew members who reported CLI, defined as at least one of the following symptoms: fever, cough, difficulty breathing, shortness of breath, new olfactory disorder, or new taste disorder; or at least two or more of the following symptoms: sore throat, nasal congestion, rhinorrhea, chills, rigors, myalgias, headache, fatigue, vomiting, or diarrhea. Close contacts were defined as crew members who were less than 6 feet away from a crew member with a positive NAAT or antigen test result or crew member who reported CLI for a total of 15 minutes or more over a 24-hour period based on the infectious period of the case (i.e., starting 2 days before the case had any symptoms (or, for crew members without symptoms, 2 days before the positive specimen collection date) [5]. Embarkation testing results were not included in this analysis, as crew who tested positive upon embarkation were isolated on board for 10 days and did not contribute to onboard transmission.
Cruise ship personnel reported aggregate SARS-CoV-2 test results, vaccination rates, and crew members requiring hospitalization or medical evacuation using CDC’s online COVID-19 surveillance instrument for cruise ships [5]. If ships experienced a large outbreak (≥ 20 SARS-CoV-2 cases among crew or passengers identified in a 14-day period), healthcare personnel on board were requested to collect additional case information such as demographics, symptoms, vaccination history, occupation, living and working quarters, and numbers of crew member close contacts identified per crew member case. Crew and passengers were considered as having completed a primary COVID-19 vaccine series after the date they received the second dose of a two-dose mRNA series or one dose of a single-dose vaccine. Crew members for whom additional case data were not available were excluded from this analysis for having partial or missing data for vaccination history.
Data Analysis Data collected from CDC’s online COVID-19 surveillance instrument were used to calculate the average number of crew members onboard during the period of data collection and proportion of crew members who completed a primary vaccine series. Additional analyses were limited to crew members who tested positive for SARS-CoV-2 using a NAAT or antigen assay and for whom additional case data were available as part of a large outbreak investigation. Comparable data were not available for crew members who were not tested or tested negative. Descriptive statistics of demographic characteristics, vaccination history, living and working conditions, and numbers of crew member close contacts identified per crew member case were calculated for SARS-CoV-2-positive crew members who were part of large outbreaks. The number of days since last vaccination was calculated along with the number of close contacts identified. The Kruskall-Wallis test was used to test for statistical differences [12]. Statistical significance was determined at p < 0.05. Data management and analyses were conducted using R (version 3.6.3; The R Foundation), SAS (version 9.4; SAS Institute, Cary, North Carolina), and Microsoft Excel. This activity was deemed not to be research as defined in 45 CFR 46.102(l) and IRB review was not required. §
Result
Between June and October 2021, a total of 1,079 cases of crew members who tested positive for SARS-CoV-2 were reported to CDC by 98 cruise ships operating under the CSO. An estimated daily average of 52,466 crew members were on board passenger-voyaging ships during the same period and 86% had completed a primary vaccine series (data not shown). Twenty-six crew members were excluded from this analysis for having partial or missing data for vaccination history.
Additional case data were available for 402 (37%) SARS-CoV-2- positive crew members on 21 ships who were part of a large outbreak. The remainder of the analysis is for these crew members. All infected crew members with additional information had completed a primary vaccine series prior to their SARS-CoV-2 infection. Demographic characteristics, vaccination history, and illness severity of SARS-CoV- 2-positive crew members with additional case report data from crew members who were part of a large outbreak are presented in [Table 1]. The median age was 37 years (interquartile range [IQR]:31–43 years). Most crew were from the Western Pacific global region (n=180; 45%) followed by Southeast Asia (n=133; 33%), the Americas (n=46; 11%), Europe (n=36; 9%), and Africa (n=7; 2%). Median numbers of days from completion of primary series and from ship embarkation until SARS-CoV-2 infection were 76 days (IQR:53–98 days) and 57 days (IQR:49–78 days), respectively.
| Crew n (%) | ||
|---|---|---|
| Age in years, median (IQR) | 37 (31-43)§ | |
| Age group, in years | ||
| 18–29 | 83 (21) | |
| 30–39 | 169 (42) | |
| 40–49 | 111 (28) | |
| ≥50 | 34 (8) | |
| Missing | 5 (1) | |
| Global region of permanent residence | ||
| Western Pacific | 180 (45) | |
| Southeast Asia | 133 (33) | |
| Americas | 46 (11) | |
| Europe | 36 (9) | |
| Africa | 7 (2) | |
| Vaccine manufacturer of primary series | ||
| Janssen (Johnson & Johnson) | 302 (76) | |
| Pfizer-BioNTech | 48 (12) | |
| AstraZeneca | 24 (6) | |
| Sinovac-CoronaVac | 22 (5) | |
| Moderna | 4 (1) | |
| Covishield | 2 (0.5) | |
| No. of days from completion of primary series to positive SARS-CoV-2 test result: | ||
| Median (IQR) | 76 (53–98)§ | |
| No. of days from ship embarkation to positive SARS-CoV-2 test result: | ||
| Median (IQR) | 57 (49–78)§ | |
| Presence of symptoms on day of positive SARS-CoV-2 test result† | ||
| Yes | 139 (35) | |
| No | 263 (65) | |
| Risk factors for severe COVID-19‡ | ||
| Yes | 10 (2) | |
| No | 281 (70) | |
| Missing | 111 (28) | |
| Sought medical attention from ship clinician (i.e., medical center or in-cabin clinician visit) | ||
| Yes | 108 (27) | |
| No | 264 (66) | |
| Missing | 30 (7) | |
| * Crew members were considered as having completed a primary vaccine series two weeks after they received the second dose of a two-dose mRNA series or two weeks after they received one dose of a single-dose vaccine. Vaccine manufacturers were identical for the primary series and the last vaccine received for 401 (99%) crew members. Ships with ≥ 20 SARS-CoV-2 positive cases among crew or passengers identified in a 14-day period were defined as having large outbreaks. § IQR: interquartile range † Crew member reported at least one or more of the following symptoms of COVID-19-like illness: fever, cough, difficulty breathing, shortness of breath, new olfactory disorder, or new taste disorder; or at least two or more of the following symptoms: sore throat, nasal congestion, runny nose (rhinorrhea), chills, rigors, muscle or body aches (myalgias), headache, fatigue, vomiting, or diarrhea. ǂ Includes adults aged 65 years and older, pregnant or recently pregnant people, or people with co-morbid medical conditions. (Underlying Medical Conditions Associated with Higher Risk for Severe COVID-19: Information for Healthcare Professionals | CDC) | ||
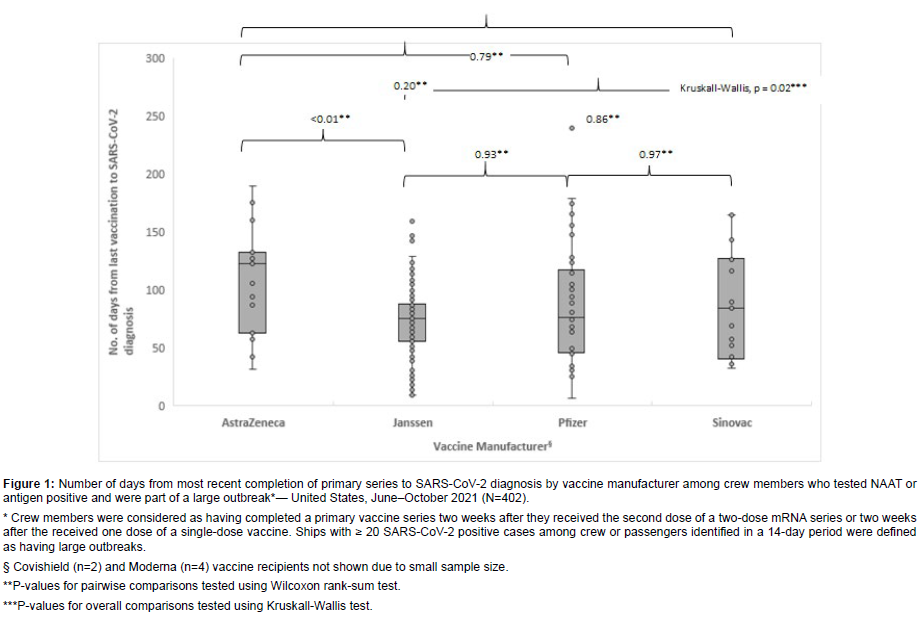
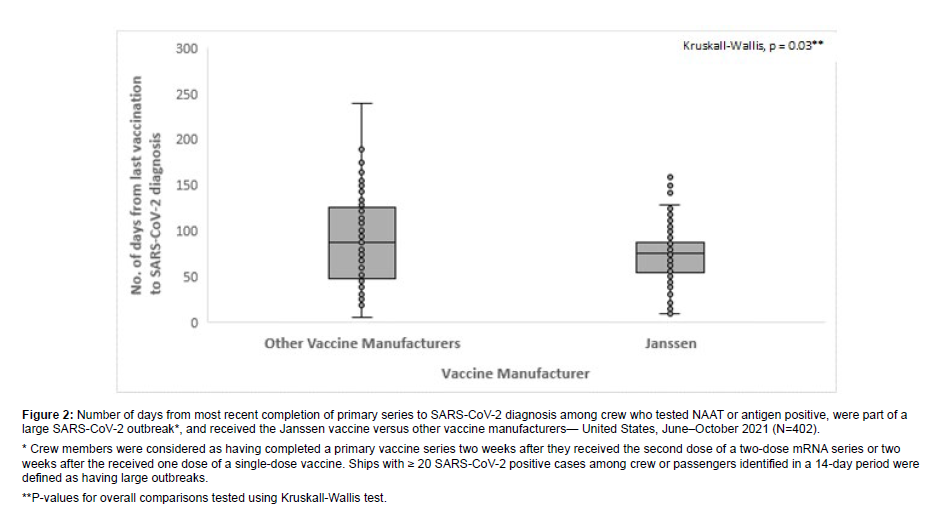
Most SARS-CoV-2-positive crew with additional case data (n=302; 76%) received the Janssen vaccine followed by Pfizer-BioNTech (n=48; 12%), AstraZeneca (n=24; 6%), Sinovac-CoronaVac (n=22; 5%), Moderna (n=4; 1%), and Covishield (n=2; 0.5%) (Table 1). Median number of days from completion of primary series until positive test result was highest among crew members who received the AstraZeneca [115 days (IQR: 61–131 days)] and Sinovac-CoronaVac [87 days (IQR: 42–126 days)] vaccines The median number of days from last vaccination until infection was statistically higher for AstraZeneca vaccine recipients than Janssen vaccine recipients [75 days (IQR: 55–87 days); p=<0.01)] [Figure 1]. Janssen vaccine recipients also had lower median days from completion of primary series until positive test result compared to a composite measure of crew who received vaccines from other manufacturers [86 days (IQR:46–125; p=0.03)] [Figure 2].
Figure 1: Number of days from most recent completion of primary series to SARS-CoV-2 diagnosis by vaccine manufacturer among crew members who tested NAAT or antigen positive and were part of a large outbreak*— United States, June–October 2021 (N=402). * Crew members were considered as having completed a primary vaccine series two weeks after they received the second dose of a two-dose mRNA series or two weeks after the received one dose of a single-dose vaccine. Ships with ≥ 20 SARS-CoV-2 positive cases among crew or passengers identified in a 14-day period were defined as having large outbreaks. § Covishield (n=2) and Moderna (n=4) vaccine recipients not shown due to small sample size. **P-values for pairwise comparisons tested using Wilcoxon rank-sum test. ***P-values for overall comparisons tested using Kruskall-Wallis test.
Figure 2: Number of days from most recent completion of primary series to SARS-CoV-2 diagnosis among crew who tested NAAT or antigen positive, were part of a large SARS-CoV-2 outbreak*, and received the Janssen vaccine versus other vaccine manufacturers— United States, June–October 2021 (N=402). * Crew members were considered as having completed a primary vaccine series two weeks after they received the second dose of a two-dose mRNA series or two weeks after the received one dose of a single-dose vaccine. Ships with ≥ 20 SARS-CoV-2 positive cases among crew or passengers identified in a 14-day period were defined as having large outbreaks. **P-values for overall comparisons tested using Kruskall-Wallis test.
Thirty-five percent (n=139) of infected crew reported symptoms and 27% (n=108) sought medical attention from the healthcare personnel on board (Table 1). No COVID-19-related onboard hospitalizations, medical evacuations, or deaths were reported. More than 40% of these infected crew members either shared a cabin or a restroom with another crew member at their time of diagnosis [Table 2]. The highest proportion of infected crew (37%; n=148) worked in the restaurant department followed by 29% (n=114) working in housekeeping-related occupations. Forty-two percent (n=167) of cases reported 1 or 2 close contacts among other crew members within two days before symptom onset or before the positive specimen collection and 24% (n=95) reported 3 or more close contacts (Table 2). The occupations of infected crew members had no significant effect on the average numbers of close contacts identified (p=1.00).
| Crew n (%) | |
|---|---|
| Shared cabin at time of diagnosis | |
| Yes | 161 (40) |
| No | 180 (45) |
| Missing | 61 (15) |
| Shared restroom at time of diagnosis§ | |
| Yes | 168 (42) |
| No | 155 (39) |
| Missing | 79 (20) |
| Working quarters | |
| Restaurant | 148 (37) |
| Housekeeping | 114 (29) |
| Other technical staff† | 33 (8) |
| Entertainment | 31 (8) |
| Casino | 24 (6) |
| Bar | 14 (4) |
| Shops/Spa | 13 (3) |
| Guest services | 11 (3) |
| Deck | 8 (2) |
| Medical | 4 (1) |
| Number of close contacts | |
| 0 | 44 (11) |
| 1-2 | 167 (42) |
| 3 or more | 95 (24) |
| Missing | 96 (24) |
| * Close contacts were defined as crew members who were less than 6 feet away from an infected crew member for a total of 15 minutes or more over a 24-hour period based on the infectious period of the case (i.e., starting 2 days before the case had any symptoms (or, for crew members without symptoms, 2 days before the positive specimen collection date). § Shared restrooms varied by ship and may or may not have been located within sleeping quarters. Ships with ≥ 20 SARS-CoV-2 positive cases among crew or passengers identified in a 14-day period were defined as having large outbreaks. † e.g., administrative, engine room/engineering, and Information Technology |
|
Discussion
This is the first description of SARS-CoV-2 infections among cruise ship crew members during the Delta variant period since passenger voyaging operations resumed in in the United States in June 2021; it demonstrates the continued risk of SARS-CoV-2 infection in these congregate settings despite high vaccination coverage and implementation of other COVID-19 mitigation measures. Crew members onboard cruise ships live and work in spaces with high population density and have frequent close contact with other crew and passengers, which likely increases their risk of exposure to the SARSCoV- 2 virus [1]. Demographic characteristics, vaccination history, living and working conditions, and numbers of crew member close contacts identified per crew member case were reported to the CDC from a total of 402 SARS-CoV-2-positive crew members onboard 21 cruise ships cruise ships experiencing outbreaks while operating under the CSO, and to our knowledge, represents the largest sample available of crew members who tested positive for SARS-CoV-2 after passengervoyaging resumed.
Resumption of passenger-voyaging cruising under U.S. jurisdiction occurred during the emergence of the SARS-CoV-2 Delta variant, prior to the availability of booster vaccinations [13, 14]. The Delta variant’s higher transmissibility compared to wild type and increased ability to evade immune protection could partially explain outbreaks among crew members despite vaccination requirements and protocols to manage COVID-19 [15]. Our analysis estimated the period prevalence of SARSCoV- 2 infection to be 2.1% of approximately 52,000 crew members, which is a reliable indicator of asymptomatic and symptomatic infection during this time period given that ships operating under the CSO conducted prospective, active SARS-CoV-2 surveillance. In comparison, prevalence rates among crew members reported from other cruise ships that experienced outbreaks over the same period were much higher (ranging from 6.0% to 11.1%) than those reported in this investigation [8]. This difference is likely due to our inclusion of all crew cases reported onboard cruise ships sailing under the CSO rather than only from ships experiencing SARS-CoV-2 outbreaks. Our analysis did not examine vaccine effectiveness among crew members; however, our findings are seemingly consistent published descriptions of waning vaccine effectiveness over time since vaccination [16]. In our analysis, 75% of cases were reported more than 50 days after the crew member’s last vaccination and none of the infected crew members required hospitalization or medical evacuation. More than three quarters of crew members included in our analysis had received the Janssen vaccine, possibly because of the convenience of the single-dose primary series; however, our findings indicated that Janssen vaccine recipients had significantly fewer days from completion of primary series of vaccine to positive test result compared to crew who received vaccines from other manufacturers. In addition, only three of the six vaccines listed were approved or authorized for use in the U.S. during the time of this investigation. This is likely because most infected crew with additional case data were from Western Pacific or Southeast Asian global regions. The cruise industry could assist crew members with remaining up to date with their vaccines by providing or facilitating vaccinations, which includes additional doses for individuals who are immunocompromised, and booster doses as recommended by CDC and World Health Organization guidance [17-18]. Studies have shown that people who are up to date with their vaccines are less likely to experience severe illness [19-20].
Cruise ship crew members live in close quarters, often with regular interaction with other crew and passengers [21], putting them at risk of exposure to the SARS-CoV-2 virus. In our investigation, restaurant and housekeeping positions were the most frequently reported occupations among cases, and more than 40% of crew members who tested positive were sharing a closed space with another crew member at the time of diagnosis. Restaurant and housekeeping positions typically represent the largest departments on cruise ships, although the composition of crew members varies by cruise line [21]. Although we cannot say that those working in these areas are at higher risk because we cannot calculate attack rates by working quarters, our results identified a high number of cases in these positions which suggests enhancing mitigation measures for crew members working in these positions might reduce numbers of infections among vaccinated crew members. Further research might help ascertain whether crew member’s probability of being exposed to pathogens is affected by their occupations and living conditions and the extent to which crew are a vector to passengers or vice versa. The CDC developed specific strategies that have evolved over the course of the pandemic to assist the cruise industry with mitigating the spread of COVID-19 on board [22]. Cruise lines should continue to monitor the frequency and severity of cases so that resources can be allocated appropriately.
This investigation was subject to several limitations. First, the conclusions from this sample of crew members who tested positive for SARS-CoV-2 may not be generalizable to all crew members operating on passenger-voyaging cruise ships. In addition, case data was collected by cruise ship clinicians and was subject to the disclosure of symptoms by the crew member being tested or evaluation in a medical center. Data were not collected from crew members who did not test positive for SARS-CoV-2, and detailed case report data was available for only 37% of all reported cases during the investigation, and only from crew members who were identified as part of a large outbreak, which may not represent characteristics found among sporadic cases among the crew. It is also important to note that crew members were not asked if they had been infected in the past as previous infection confers some level of immunity. Second, although we compared time from last vaccination to infection by the type of vaccine received by crew members, this analysis did not evaluate vaccine effectiveness and did not adjust for other risk factors for SARS-CoV-2 infection, such as age, presence of underlying medical conditions and race and ethnicity. In addition, some sample sizes from among the 6 vaccines listed were small and underpowered to detect significant differences. Finally, cases reported here occurred during Delta variant predominance (in US). Available data may be biased towards ships with outbreaks of SARSCoV- 2 because those ships provided detailed case data to the CDC.
In conclusion, COVID-19 transmission continues to occur among cruise ships crew despite vaccination and implementation of mitigation strategies. Continuous prevention and mitigation efforts are needed to protect the health and safety of crew onboard and should account for shared spaces and specific working conditions that may increase the risk of exposure to the SARS-CoV-2 virus.
Disclaimer
The findings and conclusions of this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- Guagliardo SAJ, Prasad PV, Rodriguez A, Fukunaga R, Novak RT, et al. (2022) Cruise ship travel in the era of coronavirus disease 2019 (COVID-19): A summary of outbreaks and a model of public health interventions. Clin Infect Dis 74: 490-497.
- Federal Register (2020) No sail order and suspension of further embarkation. Accessed May 20, 2022.
- Cruise Lines International Association (2020) CLIA announces voluntary suspension in U.S. cruise operations. Washington, DC: Cruise Line International Association. Accessed May 20.
- Kordsmeyer AC, Mojtahedzadeh N, Heidrich J, Militzer K, von Münster T, et al. (2021) Systematic review on outbreaks of SARS-CoV-2 on cruise, Navy and cargo ships. Int J Environ Res Public Health 18:5195.
- Centers for Disease Control and Prevention (CDC). Technical Instructions for CDC’s COVID-19 Program for Cruise Ships Operating in U.S. Waters. Accessed May 20.
- Moriarty LF, Plucinski MM, Marston BJ, Kurbatova EV, Knust B, et al. (2020) Public Health Responses to COVID-19 Outbreaks on Cruise Ships- Worldwide. MMWR Morb Mortal Wkly Rep 69: 347-352.
- Lee BU (2021) A high attack rate of 90% of SARS-CoV-2 Delta variant infections in crew personnel on a single navy ship. J Travel Med 28(8).
- Moritz ED, Oraka E, Jean-Louis M, Scott S, White S et al. (2022) Outbreaks of SARS-CoV-2 test positive COVID-19 among highly-vaccinated populations on four cruise ships after resumption of passenger cruising – United States, August–November 2021. In Development.
- Servies TE, Larsen EC, Lindsay RC, Jones JS, Cer RZ, et al. (2022) Notes from the field: Outbreak of COVID-19 among a highly vaccinated population aboard a U.S. Navy ship after a port visit - Reykjavik, Iceland, July 2021. MMWR Morb Mortal Wkly Rep 71: 279-281.
- Codreanu TA, Pingault N, O'Loughlin E, Armstrong PK, Scalley B (2021) The healthy crew, clean vessel, and set departure date triad: Successful control of outbreaks of COVID-19 on board four cargo vessels.Prehosp Disaster Med 36: 611-620.
- ZuckermanDM (2021) Emergency Use Authorizations (EUAs) Versus FDA Approval: Implications for COVID-19 and Public Health. American Journal of Public Health111:1065-1069.
- Feir-Walsh BJ, Toothaker LE (1974) An Empirical Comparison of the Anova F-Test, Normal Scores Test and Kruskal-Wallis Test Under Violation of Assumptions. Educational and Psychological Measurement. 34(4):789-799.
- World Health Organization (2022) Tracking SARS-CoV-2. Accessed August 23.
- Bolze A, Luo S, White S (2022) SARS-CoV-2 variant Delta rapidly displaced variant Alpha in the United States and led to higher viral loads. Cell Rep Med 3(3): 1-6.
- He X, He C, Hong W (2021) The challenges of COVID-19 Delta variant: Prevention and vaccine development. MedComm 2: 846-854.
- Collier AY, Brown CM, McMahan KA, Jingyou Y, Jinyan L, et al. (2022) Characterization of immune responses in fully vaccinated individuals after breakthrough infection with the SARS-CoV-2 delta variant.Sci Transl Med 14: 641.
- Centers for Disease Control and Prevention (2022) COVID-19 Vaccine Boosters.
- World Health Organization (2022) Interim statement on booster doses for COVID-19 vaccination. Accessed June 23.
- Mbaeyi S, Oliver SE, Collins JP, Godfrey M, Goswami ND, et al. (2021) The Advisory Committee on Immunization Practices' Interim Recommendations for Additional Primary and Booster Doses of COVID-19 Vaccines - United States, 2021.MMWR Morb Mortal Wkly Rep. 70(44): 1545-1552.
- Rotshild V, Hirsh-Raccah B, Miskin I, Mordechai M, Matok I (2021)Comparing the clinical efficacy of COVID-19 vaccines: a systematic review and network meta-analysis.Sci Rep 11(1): 227-277.
- Cruiseshipjobs.com (2022) Career advice.
- Centers for Disease Control and Prevention (2022) Guidance for cruise ships on the mitigation and management of COVID-19.
Indexed at, Google Scholar , Crossref
Indexed at, Google Scholar , Crossref
Indexed at, Google Scholar , Crossref
Indexed at, Google Scholar , Crossref
Indexed at, Google Scholar , Crossref
Indexed at, Google Scholar , Crossref
Indexed at, Google Scholar , Crossref
Indexed at, Google Scholar , Crossref
Indexed at, Google Scholar , Crossref
Indexed at, Google Scholar , Crossref
Indexed at, Google Scholar , Crossref
Citation: Oraka E, Moritz ED, Jean-Louis M, Scott S, White S, et al. (2023) SARSCoV- 2 Infections among Crew Members on Board Passenger-Voyaging Cruise Ships during a Period of Delta Variant Predominance United States, June–October 2021. Occup Med Health 10: 446. DOI: 10.4172/2329-6879.1000446
Copyright: © 2023 Oraka E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1653
- [From(publication date): 0-2023 - Dec 04, 2024]
- Breakdown by view type
- HTML page views: 1460
- PDF downloads: 193