Safe Delivery Service Utilization and Associated Factors among Women of Childbearing Age in Ejere Town, West Shoa, Oromia Regional State, Ethiopia
Received: 01-Aug-2019 / Accepted Date: 08-Jan-2020 / Published Date: 27-Jan-2020 DOI: 10.4172/2161-0711.1000677
Abstract
Background: The impact of health of a woman is significant in many ways. A woman’s health determines her own life, her family’s welfare, and development of her country. However, due to lack of preventive activities and suitable care, most of the maternal mortalities happen in developing countries.
Objective: To assess safe delivery service utilization and factors associated among women of child bearing age who gave birth during the period of two years preceding the study in Ejere town, West Shoa Zone, Oromia Regional State, Ethiopia.
Methods: A community based cross sectional study was conducted in Ejere town from October 26 to November 20, 2015 on 228 childbearing age women. Data were collected by using pre-tested structured questionnaire on magnitude and factors associated with safe delivery.
Results: One hundred forty five (64.4%) and 80 (35.5%) of study subjects were opt to use home delivery and institutional delivery respectively. The multivariate analysis revealed that age, education and antenatal care (ANC) attendance were found to be significant predictors of the safe delivery.
Conclusion: This study showed that majority of women preferred home delivery (64.4%) to safe delivery. Age, education and antenatal care attendance were significant predictors for the choice of women delivery place. Hence, the health institutions and other responsible bodies need make efforts to increase community based health education.
Keywords: Safe delivery; Childbearing age; EJERE town
Abbreviations
WHO: World Health Organization; EMDHS: Ethiopian Mini Demographic and Health Survey: AOR: Adjusted Odds Ratio; CI: Confidence of Interval
Introduction
Pregnancy is normal and healthy state; however, this normal life affirming process carries with it serious risks of death and disability unless proper care is given [1]. The effect of a woman’s health to her own health, to her family’s wellbeing and in general to the economy of her community and her country is critical [2]. Health of a mother has close relationship with the general life condition of women. Deprived maternal health is associated with lack of education, economic opportunities and power over the decision that governs their lives [1,2]. Sub-Saharan Africa and Asia account for 83.8% of maternal death that influenced the global distribution. Though the estimated regional causes of death are not clearly known, there is considerable variation across regions according to point estimates. In northern Africa, haemorrhage accounted for 36.9% of maternal deaths while it accounts only for 16.3% in developed regions. In Latin America and the Caribbean, the main causes of maternal death were hypertensive disorders which contribute to 22.1% of the causes of maternal death in the region. Nearly all maternal deaths attributed to sepsis were recorded in the developing countries with the highest proportion at 13.7% in southern Asia [3]. In 2015, globally about 86% of all maternal deaths were due to direct obstetric causes, mainly by maternal haemorrhage and maternal hypertensive disorder. Majority of these deaths occurred during the antepartum and post-partum periods accounting for 101, 774 and 85, 686 respectively. Antenatal care visit and safe delivery were found to influence magnitude of maternal death [4]. Survival and well-being of the mother and her child is dependent on the health services provided for her during antenatal care visit, at the time of delivery and soon after [1,5]. However, developing countries, mainly Sub-Sahara African countries have low availability and utilization of health care services. Therefore, poor health outcomes among women in Ethiopia could possibly be explained by the low utilization of safe delivery by substantial proportion of women [6].
The women ’ s health facility use may be affected by the independence they have, such as positions in the household, financial independence, mobility, and decision making power regarding one’s own health care. Women of many countries need to seek permission from their husbands because they cannot decide on their own to seek health care [7]. The magnitude of safe delivery in Ethiopia at national level was only 16% in 2014 [8]. Studies conducted in different parts of Ethiopia also show low level of safe delivery that ranges from 12.1% to 38.4% [9-12] that is low when compared to finding from three African countries which range from 48% to 79% [13-15]. Hence, it is important to understand factors that hamper safe delivery as it help us narrow the existing gaps and improve quality of health service delivery to pregnant mothers to reduce maternal morbidity and mortality that are related to pregnancy and childbirth. The aim of this study was to assess the prevalence and factors affecting safe delivery service utilization among women who gave birth within two years preceding the study period in West Shoa, Ejere town.
Methods and Materials
This study was conducted in West Shoa zone, Ejere town which is located 43 kilometers away from Addis Ababa, capital city of Ethiopia. The town had three local administrative structures called ‘kebeles’. In the town, there were one health center, three health posts and four private clinics. A community based cross-sectional quantitative study was conducted among women of child bearing age who gave birth during the period of two years preceding the study from October 26 to November 20, 2015 to assess the prevalence and factors affecting safe delivery service utilization among women of child bearing age who gave birth during the period of two years preceding the study. All child bearing age women in Ejere town were considered as source population.
The sample size was calculated using single population proportion formula by assuming the prevalence of safe delivery (p) to be 16% [8], the marginal error (d) to be 5%, 95% confidence interval (CI) and 10% non-response rate giving a sample size of 228. The total sample calculated was allocated proportionally to the three kebeles of the town. For selecting the study participants, a systematic random sampling technique was utilized after obtaining list of mothers who gave birth two years preceding the study from health extension workers.
A structured questionnaire was prepared in English by adapting the pertinent variables and terminologies for safe delivery from various studies. The questionnaire was then translated into the local language of the study area, Afan Oromo. The questionnaire was pre-tested on similar population in neighboring town and some modifications were considered based on the responses of the pre-test. Data were collected from the study population by trained data collectors who were trained for two days to enable them explain objectives of the study, informed consent and how to administer questionnaires. The collected data were entered into SPSS version 20.0 after edition and coding. After checking and cleaning for completeness prevalence of safe delivery service utilization was estimated by running frequencies with their 95% CI estimates. Bivariate and multivariate logistic regression analyses were performed to determine factors associated with safe delivery. Multivariate logistic regression was computed for factors that had pvalue of less than 0.2 in the bivariate analysis to investigate independent predictors by controlling for possible confounding factors.
Ethical consideration
The study proposal was approved by Ambo University, College of Medicine and Health Sciences, and letter of permission was written to Ejere town administrative. Verbal consent was obtained from each study participant with brief explanation on the purpose of the study and the right to refuse responding to the questions at any stage when they wanted to do so, and confidentiality was maintained.
Results
Socio-demographic characteristics of the study participants
Two hundred twenty five childbearing age women participated in the study making the response rate 98.7%. The mean age of the participants was 30.8 ± 2.84. Majority of them, 181 (80.4%), were married, 17 (7.6%) were divorced and 11 (4.9%) were widowed. Regarding educational status of the women, 121 (53.8%) of them were not formally educated, 54 (24%) attended primary education, 27 (12%) attended secondary education and only 23 (10.2%) of them attended above secondary education (Table 1).
| Variable (n=225) | Frequency | Percentage (%) | |
|---|---|---|---|
| Age | 15-19 | 3 | 1.3 |
| 20-24 | 44 | 19.6 | |
| 25-29 | 58 | 25.8 | |
| 30-34 | 46 | 20.5 | |
| ≥ 35 | 74 | 3.3 | |
| Ethnicity | Oromo | 196 | 87.1 |
| Amhara | 18 | 8 | |
| Tigre | 9 | 3.9 | |
| Gurage | 2 | 0.9 | |
| Respondent‘s educational status | No formal education | 121 | 53.9 |
| Primary education | 54 | 23.8 | |
| Secondary education | 27 | 12 | |
| Above secondary | 23 | 10.2 | |
| Husband’s educational status | No formal education | 94 | 41.8 |
| Primary education | 39 | 17.5 | |
| Secondary education | 42 | 18.8 | |
| Above secondary | 49 | 21.8 | |
| Average monthly income | <320 | 31 | 13.8 |
| 320-600 | 66 | 29.5 | |
| 601-1000 | 63 | 27.5 | |
| >1000 | 65 | 29 | |
| Religion | Orthodox | 197 | 87.8 |
| Protestant | 24 | 10.7 | |
| Muslim | 3 | 1.3 | |
| Catholic | 1 | 0.04 | |
| Occupation of the women | Housewife | 137 | 60.7 |
| Merchant | 29 | 13 | |
| Employee | 21 | 9.3 | |
| Daily laborer | 10 | 4.4 | |
| Farmer | 16 | 7.1 | |
| Student | 12 | 5.3 | |
| Head of the house | Wife | 45 | 20 |
| Husband | 177 | 78.7 | |
| Other | 3 | 1.3 | |
Table 1: Socio-demographic characteristics of the study participants, Ejere town, West Shoa Zone, Oromia Region, Ethiopia, 2015.
Reasons for their choice of delivery place
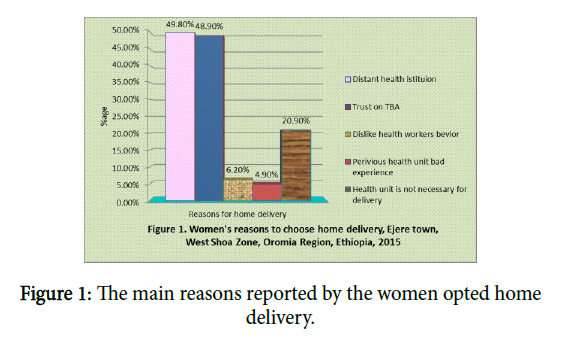
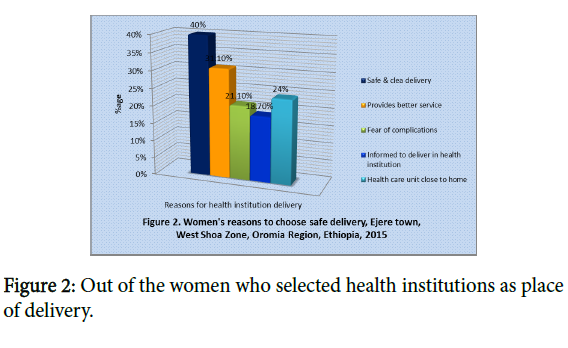
There were various reasons reported by respondents for their choice of last delivery place. Distance of health institution, 112 (49.8%) and trust on traditional birth attendants, 110 (48.9%) were the main reasons reported by the women opted home delivery (Figure 1). Out of the women who selected health institutions as place of delivery, 90 (40%) of them pointed out safe and clean delivery as a reason for their selection (Figure 2).
Decision on place of delivery
The study participants reported that last delivery took place at home for 145 (64.4%) of them, and in health institution for 80 (35.5%) of them. Regarding decision making on place of delivery, 76 (33.8%) of respondents reported to decide jointly (husband and wife), 65 (28.9%) by their husbands, 60 (26.7%) by themselves and the rest 24 (10.7%) of them reported that decision is made by traditional birth attendants.
Past obstetric practices
Majority, 176 (78.2%), of the respondents had their first marriage at age greater than eighteen years. The age at first pregnancy was greater than eighteen years for 185 (82.3%) of the study participants. Out of 156 (69.3%) of the study participants who reported to use antenatal care for the last pregnancy, 74 (47.4%) claimed to visit the antenatal care clinic two to five times. Fifty two (23.1%) of the women faced obstetric difficulties during the last pregnancy and 46 (88.4%) of these women visited health institution to seek care for the difficulties they had faced (Table 2).
| Variables | Categories | Frequency | Percentage (%) |
|---|---|---|---|
| Age at first marriage | <18 | 49 | 21.8 |
| >18 | 176 | 78.2 | |
| Age at first pregnancy | <18 | 40 | 17.8 |
| >18 | 185 | 82.2 | |
| Gravidity/total number of pregnancy | 1 | 57 | 25.3 |
| 5-Feb | 116 | 51.6 | |
| >5 | 52 | 23.1 | |
| Parity/total number of birth | 1 | 59 | 26.2 |
| 5-Feb | 117 | 52 | |
| >5 | 49 | 21.8 | |
| Use of antenatal care for the last pregnancy | Yes | 156 | 69.3 |
| No | 69 | 30.7 | |
| Number of visits (n=156) | 1 | 21 | 13.5 |
| 5-Feb | 74 | 47.4 | |
| >5 | 61 | 39.1 | |
| Any previous obstetric | Yes | 52 | 23.1 |
| difficulties | No | 173 | 76.9 |
| Specific measures taken for the difficulty (n=52) | Visit health institution | 46 | 88.4 |
| Traditional (massage, herbs) | 5 | 9.6 | |
| Nothing | 1 | 1.9 |
Table 2: Women’s past obstetrical practices in Ejere town, West Shoa Zone, Oromia Region, Ethiopia, 2015.
Decision on place of delivery
The study participants reported that last delivery took place at home for 145 (64.4%) of them, and in health institution for 80 (35.5%) of them. Regarding decision making on place of delivery, 76 (33.8%) of respondents reported to decide jointly (husband and wife), 65 (28.9%) by their husbands, 60 (26.7%) by themselves and the rest 24 (10.7%) of them reported that decision is made by traditional birth attendants.
Report by mothers on health service factors affecting their choice of delivery place
In this study, all of the study participants reported that the presence of health institution providing delivery service in their vicinity can affect their behavior to use the services. However, 58 (25.8%) and 97 (30.1%) of the respondents were not satisfied by the services provided in health institutions and believed home as better place of delivery respectively (Table 3).
| Variables | Categories | Frequency | Percentage (%) |
|---|---|---|---|
| Presence of health institution which gives delivery service | Yes | 225 | 100% |
| No | 0 | 0 | |
| Satisfaction with delivery services given at health units | Yes | 167 | 74.2 |
| No | 58 | 25.8 | |
| Reasons for lack of satisfaction (n=58) | It kills time | 26 | 44.8 |
| Unable to perform cultural ceremonies | 4 | 6.9 | |
| Unpleasant approach of health workers | 28 | 48.3 | |
| Difference between giving birth at home and health facility | Yes | 196 | 87.1 |
| No | 29 | 12.9 | |
| Better place of delivery | Home | 97 | 30.1 |
| Health unit | 126 | 57 |
Table 3: Health service factors that affect women’s choice of delivery place in Ejere town, West Shoa Zone, Oromia Region, Ethiopia, 2015.
Determinants of women’s choice of delivery place
From socio-demographic characteristics; age and educational status of women and their husbands ’ educational status had shown significant association with women’s choice of delivery place. Those women who were in the age group of 20-24 [AOR=2.1, 95% CI: 1.20, 5.50] and 25-29 [AOR=1.40, 95% CI: 1.10, 3.10] were more likely to choose health facility as delivery place than women who were in the age group of thirty five and above. Women who attended secondary education and above [AOR=3.20, 95% CI: [2.50, 3.04] were more likely to choose health facility as their delivery place compared to women who were not formally educated. Those women whose husbands attended secondary education and above [AOR=2.40, 95% CI: 3.10, 6.30] were more likely to choose health facility as their delivery place when compared to women whose husbands were not formally educated. Receiving antenatal care had also shown significant association with choice of delivery place. Women who had antenatal care visit [AOR=3.40, 95% CI: 1.43, 8.25] were more likely to choose health facility as delivery place than women who did not have any antenatal care visit (Table 4).
| Variables | No (%) (n = 225) | Delivery place | COR (95% CI) | AOR ( 95% CI) | ||
|---|---|---|---|---|---|---|
| Age | 15-19 | 3(1.3) | 1(0.4) | 2(0.9) | 5.40(.947-30.4) | .23(.15-3.6) |
| 20-24 | 44(19.5) | 14(6.3) | 30(13.1) | 4.10(2.3-7.2)* | 2.1(1.2-5.5)* | |
| 25-29 | 58(25.8) | 20(8.7) | 38(17.1) | 2.60(1.5-4.3)* | 1.4(1.1-3.1)* | |
| 30-34 | 46(20.5) | 30(13.5) | 16(7) | 1.39(.793-2.4) | .45(.19-1.08) | |
| >35 | 74(33) | 54(24) | 20(9) | 1 | 1 | |
| Respondent’s education | No formal education | 121(53.9) | 98(43.7) | 23(10.3) | 1.14(1.0-2.05)* | 3.2 (2.5-3.04)* |
| Primary | 54(23.8) | 20(9) | 34(14.8) | .096(.028-.33) | .16(.24-1.02) | |
| Secondary | 27(12) | 1(0.7) | 26(11.3) | 2.30 (1.43-2.29)* | .06(.10-9.40) | |
| Above secondary | 23(10.3) | 12(5.5) | 11(4.8) | 1 | 1 | |
| Respondent’s occupation | House wife | 137(60.7) | 94(41.9) | 43(18.8) | .15(.057-.389) | 1.1(.302-3.85) |
| Merchant | 29(13.1) | 14(6.3) | 15(6.8) | .36(.124-1.02) | 2.6(.62-11.15) | |
| Gov’t/NGO employee | 21(9.2) | 2(1.1) | 19(8.1) | 2.50(.663-9.18) | 4.9(.63-39.4) | |
| Daily laborer | 10(4.6) | 4(2) | 6(2.6) | .44(.125-1.58) | 4.09(.75-22.4) | |
| Farmer | 16(5.2) | 14(6.1) | 2(1.1) | .06(.016-.224) | 1.3(.23-7.37) | |
| Student | 12(5.2) | 3(1.3) | 9(3.9) | 1 | 1 | |
| Husband’s education | No formal education | 94(42) | 79( 35.2 ) | 15(6.8) | 1.20(9-22)* | 2.4(3.1-6.3)* |
| Primary | 40(17.5) | 27(12 ) | 12(5.5) | .05(.02-.11) | .34(.108-1.054) | |
| Secondary | 42(18.8) | 22( 9.6) | 21(9.2) | 1.90(.043-2.24)* | .33(.117-6.95) | |
| Above secondary | 49(21.7) | 5(2) | 44(19.7) | 1 | 1 | |
| Husband’s occupation | Farmer | 121(54.1) | 97(43.4) | 24(10.7) | .15(.005-.04) | .21(.052-.868) |
| Merchant | 42(18.6) | 16(7) | 26(11.6 | .1(.034-.31) | .32(.082-1.21) | |
| Daily laborer | 28(12.2) | 18(7.4) | 9(4.8) | .04(.013-.13) | .19(.045-.767 | |
| Gov’t/NGO employee | 3(15.1) | 2(.9) | 32(14.2) | 1 | 1 | |
| Monthly income | <320 | 31(13.8) | 28 (12.2) | 3 (1.5) | .08(.035-.196) | .64(.18-2.36) |
| 320-600 | 66(29.5) | 49(21.6) | 17 (7.9) | .24(.144-.404) | .65(.27-1.56) | |
| 601-1000 | 63(27.7) | 30(13.3) | 32(14.4) | 0.72(0.438-2.172) | 0.92(0.45-4.87) | |
| >1000 | 65(29) | 27(11.6) | 39 (17.5) | 1 | 1 | |
| Attended ANC | Yes | 156(69.6) | 71(31.4) | 85(38.2) | 10.80(5.9-19.7)* | 3.4(1.43-8.25)* |
| No | 69(30.4) | 61(27.3) | 8(3.1) | 1 | 1 | |
| Number of visits | 1 | 30(19.4) | 19(12.2) | 11(7.2) | .45(.194-.98)* | .52(.154-1.72) |
| 4-Feb | 106(68) | 43(27.6) | 63 (40.4) | 1.08(.55-2.15) | .86 (.023-6.37) | |
| ³ 5 | 20(12.5) | 8(5.3) | 12(7.2) | 1 | 1 | |
AOR: adjusted odds ratio, COR: crude odds ratio, ANC: antenatal care, NGO: non-governmental organization, * P value<0.05.
Table 4: Bivariate and multivariate analysis for factors associated with safe delivery, Ejere town, West Shoa Zone, Oromia Region, Ethiopia, 2015.
Discussion
This study revealed that the proportion of the study participants who reported to choose safe delivery is 36.5%. According to this study, decision to choose between safe delivery and home delivery is made by husband and wife jointly (33.8%), husband only (28.8%), women themselves (26.6%), and by traditional birth attendants (10.7%). It also showed various factors that affect women’s choice of safe delivery.
The prevalence of safe delivery in this study was 35.5%. This finding is higher than studies conducted in Tigray and Amara regions, which revealed 4.1% and 12.1% respectively [16,17]. The possible reasons for the difference could be low coverage of institutional delivery and low awareness of study participants about safe delivery for the previous studies. This in turn, might be due to, nowadays, Health Extension Workers are available in the community providing health information on maternal health care and the government had been working to increase maternal health service coverage to achieve Millennium Development Goals during that time. It is also higher (16%) than the report of Ethiopian Mini Demographic and Health Survey (EMDHS) of 2014 [8]. This might occurred due to that the EDHS report was an average of different regions of the country, that is, it includes urban and rural areas while the current study involved only one district town. However, this is lower than the reports from other developing countries like 79.3% in Nigeria and 46% in India [18]. Variation in socio-economic status and health care facilities of the countries might be a possible reason for the difference.
Most of the decisions on place of delivery were made at least by involvement of the woman: women themselves, husband and wife jointly, husband only and traditional birth attendants (26.6%, 33.8%, 28.8% and 10.7%) respectively. Despite the fact that women ’ s involvement seems to be higher in decision making, the power of women to decide without interference is relatively low (26.6%) indicating importance of some interventions.
Women who were in the earlier age (20-24 years and 25-29 years) were more likely to choose safe delivery compared to women who were thirty five years of age or more [AOR = 2.1, 95% CI: 1.2, 5.5] and [AOR = 1.4, 95% CI: 1.1, 3.1] respectively. The difference observed between the age groups might be due to better understanding of younger women about the importance of giving birth in health facilities. The older women were unwilling to choose safe delivery because they might be influenced by traditional practices of home delivery. This finding is consistent with study conducted in Sekela, Amara region [17].
Educational status of the women was found as one of the significant predictors for choice of safe delivery. Women who attended secondary education and above were more likely to choose safe delivery compared to women who were not formally educated [AOR = 3.2, 95% CI: 2.50, 3.04]. Studies conducted in Sekela, Amara region, Northern Gondar, Nigeria and Southern Tanzania had shown similar results with this finding [17,18]. Formal education may influence women to seek for more information about their health conditions helping them develop positive attitude toward safe delivery.
This study also revealed that safe delivery is significantly associated with husbands ’ educational status. Accordingly, women whose husbands were with no formal education were less likely to choose safe delivery when compared to women whose husbands attended secondary education and above [AOR = 2.4, 95% CI: 3.1, 6.3]. This finding is similar with other study conducted in India [18]. If husbands are educated, there may be less probability for restricting their wives mobility and decision for seeking health care. They may also have positive attitude toward health institution utilization for delivery [5]. This might be because if someone is educated, there would be more tendencies to care for one’s own and one’s family’s healthiness. The current study revealed that delivery place preference has significant association with antenatal care utilization. The odds of seeking safe delivery were more likely [AOR= 3.4, 95% CI: 1.43, 8.25] among women who utilized antenatal care than women who didn’t utilize antenatal care. Studies conducted in Jimma zone and Metekel zone show similar findings. This is possibly due to the advice and information given during antenatal care to the mothers regarding importance of safe delivery and the potential complications of delivery when it occurs at home.
Limitations
It is not possible to determine potential temporal relationship between safe delivery and various factors due to the study design and respondents' recall bias.
Conclusion
In conclusion, magnitude of safe delivery was relatively low in the study area and the study revealed that age of the respondents, women’s and husbands’ educational status and ANC attendance were significant predictors for safe delivery. Hence, it is necessary for health institutions and health offices in the study area to use health extension workers for educating mothers to seek safe delivery. As indicated in this study, for some mothers, cultural beliefs were barriers to seek safe delivery which needs working with influential people in the community to break the barriers and enable mothers attend their delivery in health institutions. In general, increasing awareness of mothers and community at large about the importance of safe delivery is essential.
Acknowledgements
We are grateful to Ambo University for providing ethical approval for the study. The study participants are also appreciated for their participation.
References
- WHO (2004) Beyond the numbers: Reviewing maternal deaths and complications to make pregnancy safer. Geneva.
- Say L, Chou D, Gemmill A, Tunçalp Ö, Moller AB, et al. (2014) Global causes of maternal death: A WHO systematic analysis. Lancet Global Health 2: e323-33.
- Kassebaum NJ, Barber RM, Bhutta ZA, Dandona L, Gething PW, et al. (2016) Global, regional, and national levels of maternal mortality, 1990–2015: A systematic analysis for the global burden of disease study 2015. Lancet 388: 1775-812.
- Mahdi SS, Habib OS (2010) A study on preferences and practices of women regarding place of delivery. World Health Organization.
- Birmeta K, Dibaba Y, Woldeyohannes D (2013) Determinants of maternal health care utilization in Holeta town, central Ethiopia. BMC health services research 13: 256.
- Amano A, Gebeyehu A, Birhanu Z (2012) Institutional delivery service utilization in MunisaWoreda, South East Ethiopia: a community based cross-sectional study. BMC pregnancy childbirth 12: 105.
- Teferra AS, Alemu FM, Woldeyohannes SM (2012) Institutional delivery service utilization and associated factors among mothers who gave birth in the last 12 months in Sekela District, North West of Ethiopia: A community-based cross sectional study. BMC pregnancy childbirth 12: 74
- Hagos S, Shaweno D, Assegid M, Mekonnen A, Afework MF, et al. (2014) Utilization of institutional delivery service at Wukro and Butajera districts in the Northern and South Central Ethiopia. BMC pregnancy and childbirth 14: 178.
- Fotso JC, Ezeh A, Oronje R (2008) Provision and use of maternal health services among urban poor women in Kenya: What do we know and what can we do?. J Urban Health 85: 428-442.
- Esena RK, Sappor MM (2013) Factors associated with the utilization of skilled delivery services in the Ga East Municipality of Ghana Part 2: Barriers to skilled delivery. Int J Sci Tech Res 2: 195-207.
- Mageda K, Mmbaga EJ (2015) Prevalence and predictors of institutional delivery among pregnant mothers in Biharamulo district, Tanzania: A cross-sectional study. Pan Afr Med J 21: 51.
- Tsegay Y, Gebrehiwot T, Goicolea I, Edin K, Lemma HH, et al. (2013) Determinants of antenatal and delivery care utilization in Tigray region, Ethiopia: A cross-sectional study. Int J Equity Health 12: 30.
- Iyaniwura CA, Yussuf Q (2009) Utilization of antenatal care and delivery services in Sagamu, south western Nigeria. Afr J Reprod Health 13: 111-112.
- Singh PK, Rai RK, Alagarajan M, Singh L (2012) Determinants of maternity care services utilization among married adolescents in rural India. PLoS ONE 7: e31666
- Babalola S, Fatusi A (2009) Determinants of use of maternal health services in Nigeria-looking beyond individual and household factors: BMC Pregnancy Childbirth 9: 43.
- Mpembeni RNM, Killewo JZ, Leshabari MT, Massawe SN, Jahn A, et al. (2007) Use pattern of maternal health services and determinants of skilled care during delivery in Southern Tanzania: implications for achievement of MDG-5 targets. BMC Pregnancy Childbirth 7:29.
- Yegezu RT, Kitila SB (2014) Assessment of factors affecting choice of delivery place among pregnant women in Jimma Zone, South West Ethiopia: Cross Sectional Study. J Women’s Health Care 4: 211.
- Tura G, Mariam AG (2008) Safe delivery service utilization in metekel zone, North West Ethiopia. Ethiopia J Health Sci 17: 213-222.
Citation: Muse TB, Wanjo MI (2020) Safe Delivery Service Utilization and Associated Factors among Women of Childbearing Age in Ejere Town, West Shoa, Oromia Regional State, Ethiopia. J Community Med Health Educ 10: 677. DOI: 10.4172/2161-0711.1000677
Copyright: © Muse TB, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2791
- [From(publication date): 0-2020 - Nov 17, 2025]
- Breakdown by view type
- HTML page views: 1920
- PDF downloads: 871