Research Article Open Access
Role of Panoramic Radiographs in the Detection of Osteoporosis
Swapnil Parlani*, Preeti Nair, Surender Agrawal, Rajkiran Chitumalla, Gaurav Beohar, Utkarsh Katar
Department of Prosthodontics, Peoples College of Dental Sciences and Research Centre, Bhopal, India
- *Corresponding Author:
- Swapnil Parlani
Department of Prosthodontics
Peoples College of Dental
Sciences and Research Centre
Bhopal, India
Tel: 919893243002
E-mail: parlaniswap@gmail.com
Received Date: February 01, 2014; Accepted Date: February 22, 2014; Published Date: February 28, 2014
Citation: Parlani S, Nair P, Agrawal S, Chitumalla R, Beohar G et al. (2014) Role of Panoramic Radiographs in the Detection of Osteoporosis. J Oral Hyg Health 2:121. doi: 10.4172/2332-0702.1000121
Copyright: © 2014 Parlani S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Oral Hygiene & Health
Abstract
A study was conducted with 110 subjects to determine whether panoramic-based indices, mandibular cortical thickness (MCT) and Panoramic mandibular index (PMI) could be used as a diagnostic tool to differentiate normal from osteoporotic patient. Both the indices correlated significantly with bone mineral density. It was concluded that using MCT was simple with no calculations. The findings on an OPG will definitely help the dentists to identify patients with undetected low BMD and refer them to medical professionals for bone densitometry. This will help a dentist to plan the treatment accordingly for removable, fixed partial denture or implants.
Keywords
Osteoporosis; Bone density; Panoramic radiography; Diagnostic imaging; Alveolar resorption
Introduction
In human beings, the loss of bone mass with increasing age is a universally observed phenomenon. Human bones decrease in density and increase in porosity beginning at about the third decade of life [1-3]. The effect of general mineral loss of skeleton, osteoporosis, on the jawbones has been studied extensively, especially with new radiologic methods. There is an obvious association between osteoporosis and oral bone loss, the earliest suggestion of which was made by Greon in 1960 [4].
Residual ridge resorption of the jaws is also more rapid in older age group, depleted bone being prone to the injurious impact of mechanical forces [5]. An osteoporotic condition may compound these problems. Osteoporosis is a metabolic disease characterized by low bone mass and micro-architectural deterioration of bone tissues leading to enhanced bone fragility and increased fracture risk. Most experts agree that osteoporosis is also defined by the occurrence of a low trauma fracture, regardless of bone mineral density results [6,7]. Osteoporosis is defined by the WHO as bone mineral density (BMD) greater than 2.5 standard deviations below that of the young adult BMD. Z scores are preferred to measure the deviation for pre-menopausal women and men under the age of 50 years, whereas T scores are preferred for older categories in both the sexes [6,8], i.e., the term Z score is used for younger people less than 50 years of age while T score is used for older people. According to glossary of prosthodontic terms 2005 osteoporosis is a medical condition characterized by a decrease in bone mass with diminished density and concurrent enlargement of bone spaces, which produces porosity and fragility [9].
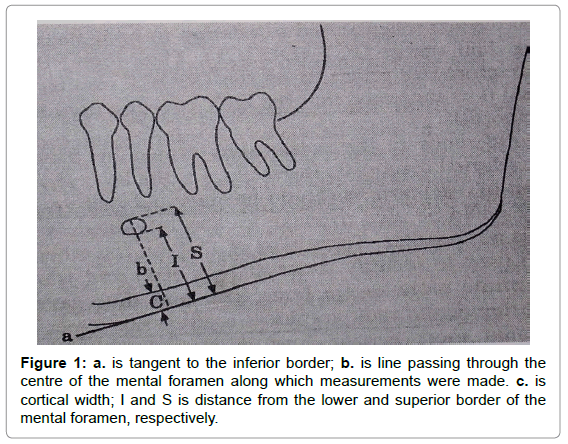
Determination of bone loss in jaws and classification of residual alveolar ridge resorption are often made by using panoramic radiographs. In 1974, Wical and Swoope [10] related residual alveolar ridge resorption to mandibular height below the inferior edge of the mental foramen. In March 1991 Benson et al. [11] presented a new index called “Panoramic Mandibular Index (PMI=C/I in figure 1), which is the ratio of thickness of the mandibular cortex(C) to the distance between the mental foramen and the inferior mandibular cortex (I). He encouraged that other scientists should test the PMI in osteoporotic population.
The panoramic radiographs are widely used for routine examination of denture patients. It would be useful to know whether radiographic changes in mandible could have a role in detection of osteoporosis. It would put the dentist in a position to identify such patients, modify the treatment plan and refer such patients for prompt management [6-8]. Such radiographs have the added advantage of a high requirement need for treatment planning (compared to the rest of the body), and less full body radiation exposure [12].
Materials and Methods
In the study, 110 subjects above 30 years of age, reporting to People’s College of Medical Sciences were examined. None of the subjects were known to have any endocrine, metabolic, skeletal disorders, or undergoing hormonal replacement therapy or taking calcitonin, bisphosphonates with the exception of intake of low doses of calcium or vitamin D. Other exclusion criteria were tobacco/alcohol abuse, bone destructive lesions of jaw/ metabolic bone diseases, renal diseases, connective tissue disorders, patients on corticosteroids or chemotherapy and /or radiotherapy and women with a history of surgically induced menopause.
The study was approved by the ethical committee of People’s College of Dental Sciences and Research Centre. Written consent was obtained from each included subject prior to commencement of the study.
The values for bone mineral density were determined by ultrasonometer device (Achilles Express, GE Medical Systems) at the heel. T-score was automatically calculated by the built-in software in the device, as the difference between the subject bone mineral density and the average density in a reference healthy 30 year old of the same sex and ethnicity, divided by the standard deviation of the reference population (WHO Scientific Group 2000). Each subject was grouped according to WHO criteria of T-score as normal, osteopenic or osteoporotic i.e. if the T-score value is below -2.5 the subject is osteoporotic, if T-score is between -1.1 to -2.4 the subject is osteopenic and if T-score is above -1.0 the subject is normal.
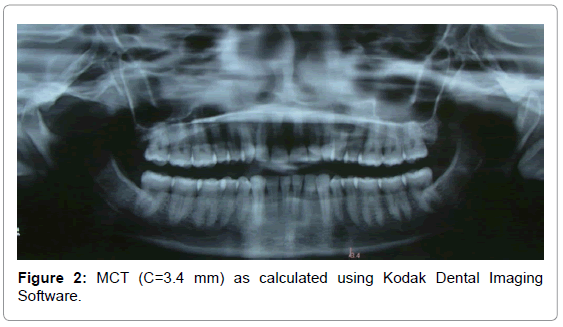
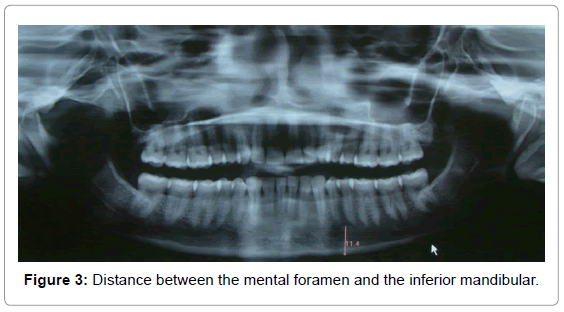
The mandibles were examined on panoramic images taken with radiographic apparatus, Kodak 8000C digital Panoramic and Cephalometric system (Trophy, France), by a single operator. Each panoramic radiograph was viewed by an oral radiologist in a blinded fashion [13] i.e. the radiologist was unaware of the T scores of the subjects. Two measurements each of mandibular cortical thickness (MCT=C in Figure 1) and Panoramic mandibular index (PMI=C/I in Figure 1) were recorded on both the sides of mandible using Kodak Dental Imaging Software 6.7. MCT (Figure 2) is the thickness of cortical bone at the lower border of mandible, below mental foramen. The PMI is the ratio of the thickness of the mandibular cortex to the distance between the mental foramen and the inferior mandibular cortex (I in Figure 3).
The results of the study of panoramic images were compared with the T-score grouping of the subjects. The data were expressed as mean and standard deviation. Analysis of variance (ANOVA) was performed to determine group differences in morphometric analysis. Pearson correlation coefficients were used to identify relation between variables. P values were considered to be statistically significant if less than 0.05.
Results
The present study examined 110 subjects, with the age range of 30- 76 years and a mean of 50. 11.81% (n=13) of total subjects had normal T-scores, 69.09% (n=76) were osteopenic and 19.09% (n=21) were osteoporotic subjects. There was no significant difference between the right and the left sides with either parametric or nonparametric test. Therefore only the measurements from the right side were used in further calculations.
Descriptive statistics for the various clinical parameters studied have been charted in Table 1. Table 2 indicate that pearson correlation matrix shows significant correlation (p<0.05) between the T-scores and mandibular cortical thickness. According to the pearson correlation coefficient, T-scores correlated positively with the panoramic mandibular index (p<0.05). Results of one-way ANOVA (Table 3) revealed significant differences between mean MCT and PMI scores of osteoporotic, osteopenic and normal groups of the study population. Table 4 shows distribution of MCT and PMI according to age. In any age group if the subject is osteoporotic the MCT values are lower (2.4 to 3.0).
| N | Mean | ||
|---|---|---|---|
| MCT | Normal | 13 | 6.3385 |
| osteopenic | 76 | 4.4184 | |
| osteoporotic | 21 | 2.9238 | |
| Total | 110 | 4.3600 | |
| PMI | normal | 13 | .57811015 |
| osteopenic | 76 | .39810477 | |
| osteoporotic | 21 | .30833307 | |
| Total | 110 | .40223990 | |
Table 1: T- Score distribution according to MCT & PMI.
| df | F | P* | |
|---|---|---|---|
| MCT | 2 | 51.284 | .000 |
| PMI | 2 | 18.828 | .000 |
*value of P is significant at P<0.05
Table 2: Pearson’s correlation coefficients for T Score and MCT, PMI.
| Dependent Variable | T-SCORE | Mean Difference | P |
|---|---|---|---|
| MCT | Osteoporotic vsosteopenic | 1.49461 | .000 |
| Osteoporotic vs normal | 3.41465 | .000 | |
| Osteopenicvs normal | 1.92004 | .000 | |
| PMI | Osteoporotic vsosteopenic | .089771701 | .012 |
| Osteoporotic vs normal | .269777082 | .000 | |
| Osteopenicvs normal | .269777082 | .000 |
Table 3: Results of post-hoc Tukey’s test.
| Age | TSCORE | MCT | PMI | |
|---|---|---|---|---|
| 30-39 Years | normal | Mean | 6.2667 | .54767574 |
| N | 9 | 9 | ||
| Std. Deviation | .85878 | .146796473 | ||
| osteopenic | Mean | 4.3333 | .42824085 | |
| N | 24 | 24 | ||
| Std. Deviation | 1.37134 | .170286898 | ||
| Total | Mean | 4.8606 | .46081400 | |
| N | 33 | 33 | ||
| Std. Deviation | 1.51677 | .170725288 | ||
| 40-49 Years | normal | Mean | 6.5500 | .62185478 |
| N | 2 | 2 | ||
| Std. Deviation | .91924 | .099635463 | ||
| osteopenic | Mean | 4.4389 | .40292392 | |
| N | 18 | 18 | ||
| Std. Deviation | 1.02964 | .103778160 | ||
| osteoporotic | Mean | 2.4500 | .27232143 | |
| N | 2 | 2 | ||
| Std. Deviation | .21213 | .002104485 | ||
| Total | Mean | 4.4500 | .41095378 | |
| N | 22 | 22 | ||
| Std. Deviation | 1.30448 | .123746477 | ||
| 50-59 Years | normal | Mean | 6.7000 | .63809524 |
| N | 1 | 1 | ||
| Std. Deviation | ||||
| osteopenic | Mean | 4.3000 | .35746189 | |
| N | 8 | 8 | ||
| Std. Deviation | .88156 | .061417413 | ||
| osteoporotic | Mean | 2.8889 | .25676530 | |
| N | 9 | 9 | ||
| Std. Deviation | .41667 | .070947657 | ||
| Total | Mean | 3.7278 | .32270434 | |
| N | 18 | 18 | ||
| Std. Deviation | 1.20333 | .112443706 | ||
| 60-69 Years | normal | Mean | 6.2000 | .70454546 |
| N | 1 | 1 | ||
| Std. Deviation | ||||
| osteopenic | Mean | 4.3765 | .37452706 | |
| N | 17 | 17 | ||
| Std. Deviation | .68422 | .120915427 | ||
| osteoporotic | Mean | 3.0778 | .35572816 | |
| N | 9 | 9 | ||
| Std. Deviation | .52387 | .129638787 | ||
| Total | Mean | 4.0111 | .38048366 | |
| N | 27 | 27 | ||
| Std. Deviation | .97244 | .135804314 | ||
| More than 69 Years | osteopenic | Mean | 4.7889 | .38876623 |
| N | 9 | 9 | ||
| Std. Deviation | 1.19525 | .092824356 | ||
| osteoporotic | Mean | 2.8000 | .41791045 | |
| N | 1 | 1 | ||
| Std. Deviation | ||||
| Total | Mean | 4.5900 | .39168065 | |
| N | 10 | 10 | ||
| Std. Deviation | 1.29052 | .087999581 | ||
No subject is osteoporotic in 30-39 age years group
No subject is normal in more than 69 years group
Table 4: Distribution of MCT & PMI according to age.
Discussion
There is evidence that a huge number of dental panoramic radiographs, offering greater opportunities for studying bones, are taken every year. The present study therefore utilizes panoramic radiographs [14].
It is statistically possible to show positive correlations and dependencies between the mineral density of the skeleton and changes in the mandibular cortex shown on panoramic X-ray images. These findings were partly successful due to standardization of head positioning, which in normal practice is very difficult when images are taken by different practitioners at different times. All the radiographs, in which the incisors were too wide or narrowed, were repeated as these radiographs were considered to be distorted. The study suggests that if the inferior mandibular cortical thickness (MCT) is low, the tendency toward osteoporosis is high.
from any radiograph must be considered in the light of radiographic magnification variation. In our study the same X-ray unit was used for all patients, but any research using MCT obtained from radiographs from different panoramic machines would need to modify the measurements appropriately to permit comparison. Measurements from panoramic radiographs must also be selected with reference to the potential error caused by positioning inaccuracies. Horizontal measurements vary markedly with relatively small antero-posterior positioning differences. However, vertical measurements are not similarly affected [15] and it is likely that typical antero-posterior and head-tilting positioning inaccuracies would not significantly affect MCT [16], being a vertical measurement.
PMI has no significant advantage over MCT as a measure of mandibular BMD. There were greater problems of repeatability with PMI than with MCT, which appeared to be due to problems in identification of the mental foramen in some patients. This problem of confident identification of the mental foramen has been noted previously [17]. Furthermore, it has been shown [18,19] that the mental foramen may sometimes be multiple, compounding the identification problem. Although it is possible that identification of the mental foramen may be improved by observer calibration, or by averaging repeated measurements, the results here suggest that PMI is unlikely to offer any advantages over MCT as a tool for general osteoporosis assessment or as a means of assessing mandibular BMD prior to implantology [16]. Moreover looking at the OPG one can have an idea of MCT but PMI is to be calculated.
The limitations in our study were that the number of subjects was relatively small. One area of future research would be to look at the thickness of cortical layers longitudinally to see whether any signs of osteoporosis could be detected. Longitudinally studies of mandibular bone density may also be fruitful than cross-sectional studies in the evaluation of the role of dental radiography in assessing patients for osteoporosis [20]. However there are newly proposed systems like kernel-based support vector machine (SVM) and an automatic approach utilizing a histogram based automatic clustering (HAC) algorithm with a support vector machine (SVM) to analyse dental panoramic radiographs [21,22].
Conclusion
This study was initiated to establish the basis of a preliminary diagnostic modality that may be useful to dental practitioners caring for patients at high risk for osteoporosis, because osteoporosis has been associated with tooth loss, excessive residual ridge resorption, delayed healing after tooth removal, referred dental pain caused by thinned walls of the maxillary sinus, and periodontal disease [2].
T-scores correlated positively with the panoramic mandibular index (p<0.05) and mandibular cortical thickness (p<0.05). The study suggests that if the inferior mandibular cortical thickness (MCT) is low, the tendency toward osteoporosis is high. In any age group if the subject is osteoporotic the MCT values are lower (2.4 to 3.0).
References
- Drozdzowska B, Pluskiewicz W, Tarnawska B (2002) Panoramic-base mandibular indices in relation to mandibular bone mineral density and skeletal status assessed by dual energy X-ray absortiometry and quantitative ultrasound. Dentomaxillofac Radiol 31: 361-367.
- Von Wowern N (1982) Microradiographic and histomorphometric indices of mandibles for diagnosis of osteopenia. Scand J Dent Res 90: 47-63.
- Kribbs PJ, Chesnut CH 3rd, Ott SM, Kilcoyne RF (1990) Relationships between mandibular and skeletal bone in a population of normal women. J Prosthet Dent 63: 86-89.
- Groen JJ, Duyvensz F, Halsted JA (1960) Diffuse alveolar atrophy of the jaw (non-inflammatory form of paradental disease) and pre-senile osteoporosis. GerontolClin (Basel) 2: 68-86.
- Klemetti E (1996) A review of residual ridge resorption and bone density. J Prosthet Dent 75: 512-514.
- White SC, Rudolph DJ (1999) Alterations of the trabecular pattern of the jaws in patients with osteoporosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 88: 628-635.
- Lindsay R, Christiansen C, Einhorn TA, et al. (1997) Who are candidates for prevention and treatment for osteoporosis? Osteoporos Int 7: 1-6.
- Lenchik L, Sartoris DJ (1997) Current concepts in osteoporosis. AJR Am J Roentgenol 168: 905-911.
- The Academy of prosthodontics (2005) Glossary of prosthodontic terms. J Prosthet Dent 94.
- Wical KE, Swoope CC (1974) Studies of residual ridge resorption. II. The relationship of dietary calcium and phosphorus to residual ridge resorption. J Prosthet Dent 32: 13-22.
- Benson BW, Prihoda TJ, Glass BJ (1991) Variations in adult cortical bone mass as measured by a panoramic mandibular index. Oral Surg Oral Med Oral Pathol 71: 349-356.
- Ledgerton D, Horner K, Devlin H(1997) Osteoporosis research: a dental perspective. Radiography 3: 265-277.
- Balcikonyte E, Balciuniene I, Alekna V (2004) Panoramic Radiographs in Assessment of the Bone Mineral Density. Stomatologija, Baltic Dental and Maxillofacial Journal 6:17-19.
- Taguchi A (2010) Triage screening for osteoporosis in dental clinics using panoramic radiographs. Oral Dis 16: 316-327.
- Xie Q, Soikkonen K, Wolf J, Mattila K, Gong M, et al. (1996) Effect of head positioning in panoramic radiography on vertical measurements: an in vitro study. DentomaxillofacRadiol 25: 61-66.
- Horner K, Devlin H (1998) The relationship between mandibular bone mineral density and panoramic radiographic measurements. J Dent 26: 337-343.
- Klemetti E, Kolmakov S, Heiskanen P, Vainio P, Lassila V (1993) Panoramic mandibular index and bone mineral densities in postmenopausal women. Oral Surg Oral Med Oral Pathol 75: 774-779.
- Yosue T, Brooks S, Arbor A (1989) The appearance of the mental foramina on panoramic and periapical radiographs. I. Experimental evaluation. Oral Surgery, Oral Medicine, Oral Pathology 68:360-364.
- Yosue T, Brooks SL (1989) The appearance of mental foramina on panoramic and periapical radiographs. II. Experimental evaluation. Oral Surg Oral Med Oral Pathol 68: 488-492.
- Mohajery M, Brooks SL (1992) Oral radiographs in the detection of early signs of osteoporosis. Oral Surg Oral Med Oral Pathol 73: 112-117.
- Kavitha, Akira Asano, Akira Taguchi, Takio Kurita, Mitsuhiro Sanada (2012) Diagnosis of osteoporosis from dental panoramic radiographs using the support vector machine method in a computer-aided system. BMC Medical Imaging 12:1.
- Kavitha MS, Asano A, Taguchi A, Heo MS (2013) The combination of a histogram-based clustering algorithm and support vector machine for the diagnosis of osteoporosis. Imaging Sci Dent 43: 153-161.
Relevant Topics
- Advanced Bleeding Gums
- Advanced Receeding Gums
- Bleeding Gums
- Children’s Oral Health
- Coronal Fracture
- Dental Anestheia and Sedation
- Dental Plaque
- Dental Radiology
- Dentistry and Diabetes
- Fluoride Treatments
- Gum Cancer
- Gum Infection
- Occlusal Splint
- Oral and Maxillofacial Pathology
- Oral Hygiene
- Oral Hygiene Blogs
- Oral Hygiene Case Reports
- Oral Hygiene Practice
- Oral Leukoplakia
- Oral Microbiome
- Oral Rehydration
- Oral Surgery Special Issue
- Orthodontistry
- Periodontal Disease Management
- Periodontistry
- Root Canal Treatment
- Tele-Dentistry
Recommended Journals
Article Tools
Article Usage
- Total views: 17595
- [From(publication date):
March-2014 - Jul 15, 2025] - Breakdown by view type
- HTML page views : 12603
- PDF downloads : 4992